Significant outcomes
-
Patients with anxiety had greater chance for emergency admission, higher Numerical Rating Scale (NRS) result, occurrence of cachexia and neuropsychiatric symptoms, longer duration of treatment, higher albumin concentration and lower glucose concentration.
-
Patients with neuropsychiatric symptoms had greater chance for emergency admission, higher Performance Status (PS) scale note, occurrence of dyselectrolytemia and lower albumin concentration.
-
Patients with neuropsychiatric symptoms had more than 7 times greater chance for death.
Limitations
-
The article presents a retrospective study (the data were obtained from medical records after the patient was discharged from the hospital);
-
The mental state of the patients was assessed by specialists in palliative medicine, not by psychiatrists.
Introduction
Anxiety and neuropsychiatric symptoms are the serious and frequent problems of patients suffering from stomach cancer. These symptoms worsen the quality of life and decrease patient’s prognosis.
In our research, we treat neuropsychiatric symptoms such as psychosis, delirium, cognitive impairment and confusion. Because of higher frequency of anxiety, we exclude it from the group of neuropsychiatric symptoms and make own category.
According to the data provided by World Health Organization, stomach cancer is the third (behind cancers of the lung and colorectum) most common cause of death from cancer globally. It is also the 6th most common cancer worldwide with an estimated 1.03 million new cases per year in 2018 (Stewart et al., Reference Stewart and Wild2014).
Taking into consideration the fact that stomach cancer is a frequent neoplasm worldwide and that it is often in advanced stages when found, a large number of patients with this kind of cancer are admitted to the palliative care departments.
Because of the frequency of this cancer, we decided to focus on wide spectrum of its consequences. Some neuropsychiatric disturbances, such as anxiety and other symptoms mentioned above, seemingly disconnected with neoplastic process, can have an impact on each other. That is why the aim of our study was to find factors connected with anxiety and neuropsychiatric symptoms. When we eliminate prognostic factors, we could reduce those signs. Knowledge of the consequences allows us to understand how important it is to avoid those situations.
Material and methods
We retrospectively analysed 134 patients (44 women and 90 men) who suffer from stomach cancer, admitted to the Palliative Care Unit of the University Hospital in Cracow. Patients had detailed physical examination. Doctors collected medical history including history taken from family and caregivers upon admission. Laboratory parameters including morphology, sodium, potassium, total and ionised calcium concentration, lactate dehydrogenase (LDH) activity were taken on admission. The average age of women was 63.11 years old, and the average age of men was 64.97 years old. Infiltration and metastasis of gastric cancer to surrounding organs were observed in 126 patients, including 2 patients who had metastases to central nervous system and 11 patients who had metastases to bones. Anxiety and neuropsychiatric symptoms were assessed on a structured medical interview and physical examination results.
We used univariate and multivariate logistic regression analysis to determine possible predictors, symptoms and consequences of anxiety and neuropsychiatric symptoms in terminal stomach cancer patients in 3 moments: at admission, during hospitalisation and at discharge. In the next phase after checking normality, we analysed the results of the Student t-test for independent samples test or the Mann–Whitney U-test in order to better visualise the results. Results with p < 0.05 were regarded as statistically significant. Statistical analyses were performed using Statistica version 12 for Windows (produced by StatSoft Polska).
Results
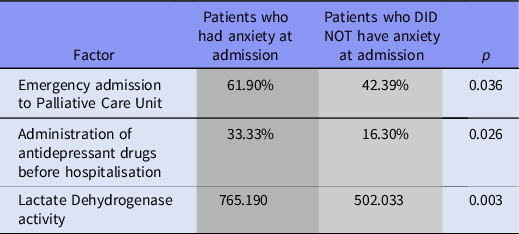
One-third (31.34%) of patients had anxiety at admission to hospital. These patients 2.2 times more were admitted in emergency to Palliative Care Unit (Tables 1 and 2). They 2.5 times more often administered antidepressant drugs before hospitalisation (Tables 1 and 2). They had also higher average activity of LDH 765.19 vs. 502.033 (Tables 1 and 2).
Table 1. Factors affecting the anxiety at admission, Student’s t-test
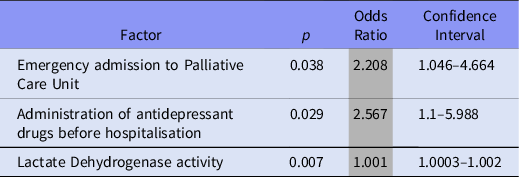
Table 2. Factors affecting the anxiety at admission, univariate logistic regression analysis results
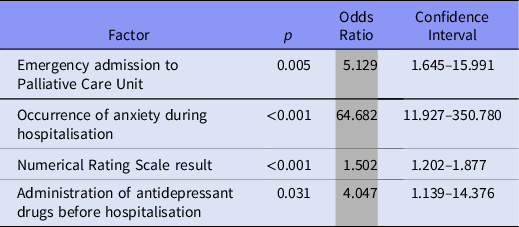
In case multivariate logistic regression analysis factors connected with anxiety at admission is emergency admission to Palliative Care Unit (OR = 5.129). Anxiety at admission enhanced 64.7 times chance for occurrence of anxiety measured during hospitalisation. Patients with anxiety at admission had 1.5 times higher Numerical Rating Scale result. According to this form of analysis, patients 4 times more often administered antidepressant drugs before hospitalisation. All results are presented in Table 3.
Table 3. Factors affecting the anxiety at admission, multivariate logistic regression analysis
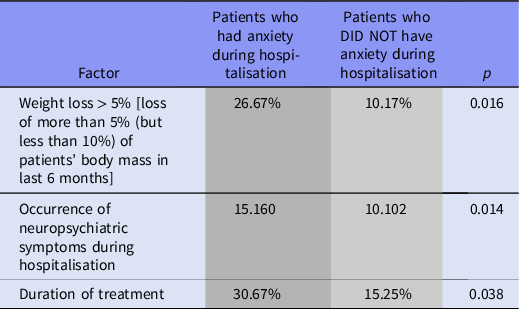
More than half of our patients (55.97%) had anxiety during hospitalisation. 26.67% of our patients with anxiety during hospitalisation had loss of weight more than 10% (but less than 30%) of their body mass in last 6 months (vs. 10.17% without anxiety and with weight loss > 10%). In patients with anxiety during hospitalisation coexist neuropsychiatric symptoms (p = 0.041, OR = 2.457, CI95% = 1.037–5.824). Patients with anxiety also had longer hospitalisation in Palliative Care Unit (p = 0.019, OR = 1.044, CI95% = 1.007–1.082). All results are presented in Tables 4 and 5.
Table 4. Factors affecting the anxiety during hospitalisation, univariate logistic regression analysis results
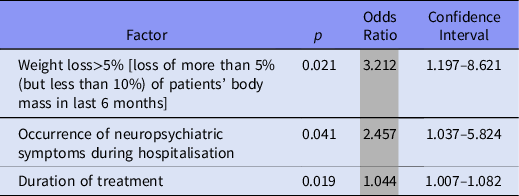
Table 5. Factors affecting the anxiety during hospitalisation, Student’s t-test from the results of univariate logistic regression analysis
More than quarter of our patients (26.12%) had anxiety at discharge. In this group of patients, we could find more often patients: who administered antidepressant drugs before hospitalisation (3 times more often), had anxiety at admission (3.3 times) and during hospitalisation (22.4 times more often, Tables 6 and 7). We could also find 4.55 times more often coexisting neuropsychiatric symptoms (Table 6).
Table 6. Factors affecting the anxiety at discharge, univariate logistic regression analysis results

Table 7. Factors affecting the anxiety at discharge, Student’s t-test from the results of univariate logistic regression analysis

According to multivariate logistic regression analysis, we know that patients with anxiety at discharge had lower glucose concentration, lower albumin concentration and more often coexist with them neuropsychiatric symptoms.
In case of 13.43% of patients, we observed neuropsychiatric symptoms at admission. Patients from this group were admitted 10.9 times more often in emergency. With each year of this age, there is 1.084 times greater chance for neuropsychiatric symptoms. In this group, patients had 2.36 times higher PS scale note and 8.61 times greater chance for electrolyte imbalances. Neuropsychiatric symptoms at admission increased chance for this type of symptoms during hospitalisation (50 times more) and at discharge ( 15.571 times more).
During multivariate logistic regression analysis, we found factors connected with neuropsychiatric symptoms at admission such as emergency admission Palliative Care Unit (24.18 times; p = 0.002; OR = 24.182; CI95% = 3.363–173.867) and higher PS scale note (4.1 times; p = 0.016; OR = 4.11; CI95% = 1.295–13.047).
Almost quarter of our patients (23.88%) had neuropsychiatric symptoms during hospitalisation. Those patients were admitted in emergency 2.517 times more often (than patients without those symptoms). In every year of life, we patient had 1.056 times greater chance for neuropsychiatric symptoms during hospitalisation. Patients with those symptoms also had higher PS scale note (OR = 1.858) and greater chance for anxiety during hospitalisation (OR = 2.457). Patients with neuropsychiatric symptoms during hospitalisation had 2.913 times greater chance for death.
In multivariate logistic regression analysis, we found factors which in complex model affect investigated variable, those are occurrence of neuropsychiatric symptoms at admission (OR = 60.825), occurrence of infection at admission (OR = 5.255) and higher risk of death (OR = 7.598).
More than 10% of our patients (11.94%) had neuropsychiatric symptoms at discharge. In every year of life, the patient had 1.077 times greater chance for those symptoms. Patients more often took antidepressant drugs before hospitalisation (OR = 3.394). Also, they had higher PS scale note (OR = 3.875), lower albumin concentration (OR = 0.864) and had more often catheter (OR = 3.333). In those patients coexist occurrence of anxiety at discharge (OR = 4.549) and occurrence of nausea and vomiting at discharge (OR = 3.126).
During multivariate logistic regression analysis, we found factors connected with neuropsychiatric symptoms at discharge such as occurrence of anxiety at discharge (5.29 times; p = 0.013; OR = 5.287; CI95% = 1.425–19.618), occurrence of dehydration (8.87 times; p = 0.009; OR = 8.864; CI95% = 1.715–45.806) and older patients’ age (1.131 times; p = 0.001; OR = 1.131; CI95% = 1.052–1.215).
Discussion
Patients treated with advanced cancer are at high risk of developing anxiety and neuropsychiatric symptoms. Prevention and appropriate treatment have a positive impact on the quality of life and can result in many benefits, including a reduction in the risk of death. The results of our research indicate factors that are associated with anxiety and neuropsychiatric symptoms. Their identification is important from a clinical point of view because it improves the quality and life expectancy of patients with terminal cancer. We took into account the occurrence of anxiety and neuropsychiatric symptoms in patients at admission, during hospitalisation and at discharge from the hospital.
The results of the study suggest a clear link between urgent admission of patients to hospital and anxiety. Sudden deterioration in health and symptoms requiring urgent intervention, such as uncontrolled pain or shortness of breath, affects mental deterioration. The level of pain experienced assessed on the SCM scale depends on the incidence of anxiety in patients (Niles & O’Donovan, Reference Niles and O’Donovan2019). The authors of another study point to a link between the occurrence of depression, anxiety disorders and emotional maladjustment and visceral sensitivity, which is associated with a stronger feeling of pain in the abdominal cavity (Zvolensky et al., Reference Zvolensky, Jardin, Farris, Kauffman, Bakhshaie, Garey, Manning, Rogers and Mayorga2018). Optimal analgesia and adaptation of pharmacotherapy to patient needs is very important in home and hospice treatment, and thus minimises the risk of emergency hospitalisation. This is very important because the severity of pain and anxiety is important determinants of quality of life (Hong & Tian, Reference Hong and Tian2014; Huang et al., Reference Huang, Du, Aihemaiti, Liu, Chen, Yu, Hu and Liu2019).
Patients with gastric cancer have the highest risk of depression in the group of patients with gastrointestinal cancer, reaching even 63.4% (Hong & Tian, Reference Hong and Tian2014). The use of antidepressants associated with depressive symptoms in the past results in a higher risk of anxiety during hospitalisation (Lee et al., Reference Lee, Oh, Lee, Lee, Pak, Choi and Jeon2018). Anxiety at admission is also associated with increased levels at the time of patient discharge. This indicates the susceptibility of individuals with psychiatric history to anxiety (Bouras et al., Reference Bouras, Markar, Burns, Huddy, Bottle, Athanasiou, Darzi and Hanna2017). Emotional resources and education are the components responsible for coping with stress, which affects mental health (Baudry et al., Reference Baudry, Anota, Mariette, Bonnetain, Renaud, Piessen and Christophe2019; Krok & Telka, Reference Krok and Telka2019).
Our study indicates a higher LDH level in patients with anxiety at admission, which is most likely related to more advanced cancer and its biological and psychological consequences in patients. High LDH is a bad prognostic factor.
Our observations show a correlation between the occurrence of weight loss above 10% and the occurrence of anxiety. Weight loss is a common problem in patients with gastric cancer, affecting up to half of the patients at the time of cancer diagnosis (Soleyman-Jahi et al., Reference Soleyman-Jahi, Abdirad, Fallah, Ghasemi, Sadeghi, Heidari, Mahmoodzadeh and Zendehdel2017) Muscle tissue catabolism and weight reduction have a negative impact on patient self-esteem and anxiety (Park et al., Reference Park, Yu, Park, Kwon and Yu2019) Reduced self-esteem increases the risk of depressive conditions (Park et al., Reference Park, Park, Lee, Kwon, Chung and Yu2018). A bad mental state reduces appetite and increases weight loss on the basis of a vicious circle.
Serum albumin level, which is a determinant of nutrition, affects mental state of patients (Jin et al., Reference Jin, Yong, Ren, Li and Yuan2018) and is a prognostic factor (Cao et al., Reference Cao, Jin, Wang and Bai2017).
There is also a clear correlation between the presence of neuropsychiatric symptoms and an increased risk of anxiety in both patients and their families.
Patients with anxiety during hospitalisation were hospitalised longer than patients without anxiety disorders.
In urgent patients, the risk of neuropsychiatric symptoms is significantly higher.
We have observed that the risk of neuropsychiatric symptoms increases with age (Kato et al., Reference Kato, Michida, Kusakabe, Sakai, Hibino, Kato, Tokuda, Kawai, Hamano, Chiba, Maeda, Yamamoto, Naito and Ito2016; Hwang et al., Reference Hwang, Lee, Son, Jung, Kim, Lee, Kong, Suh, Lee, Yang and Hahm2018; Honda et al., Reference Honda, Furukawa, Nishiwaki, Fujiya, Omori, Kaji, Makuuchi, Irino, Tanizawa, Bando, Kawamura and Terashima2018; Huang et al., Reference Huang, Du, Aihemaiti, Liu, Chen, Yu, Hu and Liu2019; Shim et al., Reference Shim, Noh, Lee, Hwang, Son, Jung, Kim, Kong, Suh, Lee, Yang and Hahm2019). This can be explained by the reduced adaptability of older people to new hospital conditions and the form of stress response.
We observed a clear correlation between reduced PS score (which is a measure of the patient’s ability to undertake daily activities and function independently) and anxiety. The study shows that depression and anxiety are strong predictors of poor physical health (Niles & O’Donovan, Reference Niles and O’Donovan2019). Another analysis indicates that low physical activity is a predictive factor of anxiety and depression (Hong & Tian, Reference Hong and Tian2014). This is an important indicator of quality of life and a prognostic factor.
In patients with neuropsychiatric symptoms, electrolyte levels should be determined as there is a clear association with dyselectrolytemia. There is a strong correlation between gastric cancer and SIADH syndrome, which may cause electrolyte disturbances (Hwang et al., Reference Hwang, Jeon, Jang, Bae, Lee, Cho, Chang and Park2014). Sodium and calcium are particularly important in the pathophysiology of these symptoms.
The presence of neuropsychiatric symptoms at admission is associated with a higher risk of their occurrence during hospitalisation and discharge from the hospital.
Anxiety during hospitalisation is a factor predisposing to neuropsychiatric symptoms. Antidepressants used in patients with depression and anxiety disorders may lead to hyponatremia, which is a risk factor for neuropsychiatric disorders.
Neuropsychiatric symptoms during hospitalisation increase the risk of death. Infection during hospitalisation clearly influences the risk of delirium, cognitive disorders and behaviour. The results of the study indicate a link between the presence of nausea and vomiting during discharge from the hospital and an increased risk of neuropsychiatric symptoms. Fluid loss may be associated with dehydration and electrolyte disorders, which are clearly related to the risk of neuropsychiatric disorders, as described above. Moreover, advanced gastric cancer may cause intracranial hypertension, which manifests itself as neuropsychiatric symptoms, nausea and vomiting (Pu et al., Reference Pu, Xu, Yin and Zhang2016).
Reduced serum albumin levels, similarly to anxiety, increase the risk of neuropsychiatric symptoms. The presence of a urological catheter in the bladder correlates with an increased risk of neuropsychiatric symptoms, which may result from impaired mobility and discomfort in intimate areas, or pain associated with blocking the outflow of urine, which is one of the indications for catheterisation.
The last correlation we have noticed in this study is the effect of dehydration on the risk of neuropsychiatric symptoms. Dehydration can be caused by reduced fluid supply, difficult fluid intake or fluid loss through vomiting and diarrhoea. Dehydration is one of the main causes of delirium. It also correlates with the risk of electrolyte disturbances, which, as discussed earlier, is a factor increasing the risk of neuropsychiatric symptoms. It is important to ensure adequate irrigation to minimise the risk of delirium.
In conclusion, our analysis has shown that the incidence of anxiety in patients with advanced gastric cancer is related to emergency admission, use of antidepressant drugs before hospitalisation, higher level of LDH, high scores of NRS, weight loss, longer duration of treatment and lower level of albumin concentration. Neuropsychiatric symptoms are associated with emergency admission, older age, higher level of PS scale, dyselectrolytemia, higher risk of death, anxiety, infection, nausea, vomiting, lower level of albumin, presence of catheter and dehydration.
It is important to know factors connected with neuropsychiatric symptoms and anxiety because thanks to that we could avoid those dangerous clinical symptoms. Nurses have more frequent contact with the patient than doctors and may notice neuropsychiatric symptoms more quickly. If the nurses have knowledge about the results of our research, they will be better at fulfilling their tasks and understanding this area of their work. If the nurses have knowledge about the results of our research, they would understand this area of their work and thanks to that they can faster react for changing situation for the better condition of patients.
Acknowledgements
We thank our colleagues from the Department of Palliative Medicine of Jagiellonian University Medical College in Cracow for the possibility to collect medical data of patients admitted to the Department of Palliative Medicine from the medical documentation made by medical staff.
Authors contributions
PB constructed an idea and hypothesis for research, planned methodology to reach the conclusion, collected data, performed the statistical analysis and wrote the paper. MB wrote the paper. MJ collected the data. DA wrote the paper and collected the data. IF-B organised and supervised the course of the project or the article and took the responsibility.
Financial support
Paweł Bryniarski was supported by the grant ‘Best of the best 2.0’ number MNISW/2017/97/DIR/NN2 of Ministry of Science and Higher Education of the Republic of Poland.
Conflict of interest
Authors declare no conflict of interests.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.










