Cognitive–behavioural therapy (CBT) is fundamentally a collaborative, empirical process of shared discovery (Reference SalkovskisSalkovskis 2002) in which client and therapist together derive a hypothesis, the ‘formulation’ (Reference PersonsPersons 1989), about the aetiology and maintenance of the client's problem. This formulation encompasses the unique predicament and response of the client in their particular present and past life contexts. This hypothesis is continuously refined in therapy as the client tests its validity against their experience and uses it to select cognitive and behavioural interventions. Instead of ‘giving solutions’, the therapist's emphasis is on guided discovery using Socratic dialogue (Reference Padesky and GreenbergerPadesky 1995) and systematic use of case-specific and standardised ratings to promote self-help and problem-solving. Failure to appreciate that therapy is explicitly based on a shared formulation, rather than being a collection of ‘bolt-on’ techniques or a manual-based approach, has resulted in a disparate range of interventions, often purely behavioural or prescriptive, being used as ‘CBT for children’ (Reference StallardStallard 2002). There is now widespread appreciation of the need to define CBT for children, young people and families and, in particular, to ensure that interventions are formulation-based through a collaborative reflection on not only individual but also systemic and developmental factors (an opinion confirmed at the inaugural meeting of the Child and Adolescent Special Interest Branch of the British Association for Behavioural and Cognitive Psychotherapies (BABCP) in 2001).
By ‘children and young people’ I generally mean individuals up to the age of 18. For conciseness in this article I will adopt the terminology of the UN Convention on the Rights of the Child, and refer to them simply as children.
The evidence base
A growing body of evidence supports the use of CBT to treat a wide range of child and adolescent mental health problems: depression (Reference Harrington, Whittaker and ShoebridgeHarrington 1998; Reference Lewinsohn and ClarkeLewinsohn 1999; Reference March, Silva and PetryckiMarch 2004), generalised anxiety (Reference Toren, Wolmer and RosentalToren 2000; Reference Barrett, Duffy and DaddsBarrett 2001), conduct disorder (Reference Henggeler, Sheidow and SprenkleHenggeler 2002; Reference White, McNally and Cartwright-HattonWhite 2003), interpersonal problems (Reference Spence, Donovan and GrahamSpence 1998), phobias (Reference Silverman, Kurtinees and GinsburgSilverman 1999), social phobia (Reference Spence, Donovan and Brechman-ToussaintSpence 2000), school refusal (Reference King, Tonge and HeyneKing 1998), sexual abuse (Reference Jones and RamchandaniJones 1999), pain management (Reference Sanders, Shepherd and CleghornSanders 1994), eating disorders (Reference Schmidt and GrahamSchmidt 1998), post-traumatic stress disorder (Reference Smith, Perrin, Yule and GrahamSmith 1998) and obsessive–compulsive disorder (Reference MarchMarch 1995; Reference Barrett, Farrell and DaddsBarrett 2005). There is also evidence in favour of using family cognitive–behavioural interventions on their own or to augment standard treatments for childhood behavioural and emotional disorders (Reference Northey, Wells and SilvermanNorthey 2003). More detailed process research is needed, however, to identify active components, individual or systemic, of CBT and indications for or against its use with specific disorders in younger populations. In adult work, limitations of CBT are becoming more well-defined (for example, it is appropriate only if problematic behavioural and cognitive responses are occurring frequently in the present), but it is less clear what the limitations of CBT may be in working with younger age groups or on a systemic basis. For reviews, see Reference StallardStallard (2002) and Reference Drinkwater and StewartDrinkwater & Stewart (2002).
A fuller evidence base is, of course, also emerging for use of longer-established psychotherapeutic approaches with children and families (Reference Fonagy, Target and CottrellFonagy 2002). It is a pity, but understandable given the scarce resources and competing agendas, that debate about which psychotherapies should be provided tends at times to become polarised, although clinical experience and reflective observation suggest many have a contribution to make. Undoubtedly, a more complete picture of the evidence base on which approaches are most appropriate for particular disorders and contexts will emerge with time. In the UK, CBT has been less available than other psychotherapeutic modalities in mental health provision for children. However, it should at the very least be readily available alongside other psychotherapies as part of comprehensive child and adolescent mental health services (CAMHS). The strong evidence base for use of CBT with children and families and the growing body of clinical experience of the strength of its use with these groups have enormous training implications (Reference DerisleyDerisley 2004). Few clinicians working with children have received core training in CBT; opportunities for CAMHS clinicians to gain clinically relevant core CBT training are extremely rare and any training opportunities are heavily oversubscribed (Reference Stallard, Udwin and GoddardStallard 2007).
Misperceptions about CBT
Much debate in psychotherapeutic circles (e.g. Reference MiltonMilton 2001) and also at the level of service provision planning both in child and adolescent and in adult mental health services seems to be founded on a number of common misperceptions about CBT. In 2002, Paul Gilbert of the BABCP issued a statement addressing the most common of these (available from the BABCP on request). In Table 1 I have summarised and interpreted this statement.
TABLE 1 Common misperceptions about CBT and the BABCP's responses to them a
| Misperception | Summary of the BABCP response |
|---|---|
| CBT is purely an individual therapy | It is also used with client dyads, families, and wider care networks and systems, and it offers a range of delivery options, for example supported self-help in stepped-care models |
| CBT takes no account of interpersonal or systemic issues | These must be considered and are operationalised in cognitive–behavioural terms in therapy |
| CBT can be a purely manual-directed approach that can be employed by clinicians without appropriate training in the modality or expert supervision | Specified levels of core skills, theoretical knowledge and appropriate support are still required (Reference Roth and PillingRoth 2008) |
| Any psychiatrist or psychologist is competent in the use of core cognitive–behavioural techniques | The standard training of psychiatrists and psychologists does not provide the required specific skills or knowledge |
| Supervision alone enables clinicians without core training to adequately deliver formal therapy | Clinicians without core training to deliver formal CBT may, however, support use of structured self-help or manualised materials where clear criteria for this are met and appropriate training and specific support are provided |
| CBT is a purely directive form of therapy | It is fundamentally collaborative |
| CBT is always a brief form of therapy | The duration and frequency of therapy follow from the formulation |
| Cognitive–behavioural therapists do not worry about, or work with, the therapeutic relationship or attend to people's feelings about their therapy or therapist or emotional responses in general | These are all operationalised and worked with in cognitive–behavioural terms in therapy |
| CBT does not address unconscious processes or take into account past experiences; in particular, it targets only symptom relief without reference to aetiology or maintenance | Formulation of causative, precipitating and maintaining factors encompassing past experience and explicit exploration of unconscious material are fundamental |
Incorporating systemic and developmental perspectives
A key difficulty in CBT with children and families has been the absence of a generic template for formulation and process that can incorporate wider interpersonal issues and systemic factors, a developmental perspective and insights more commonly associated with other psychotherapies, and in particular lead to a systemic process for working. Professionals in CAMHS have long appreciated the fundamental need to accommodate systemic, attachment and developmental factors into working with clients and have tended to work eclectically using perspectives from a range of different psychotherapies as clinically indicated. A systemic perspective is specifically required to look at major maintaining factors outside of the child that are in reciprocal interaction with surrounding individuals and are also often influenced by prevailing cultural narratives and the intentions of involved agencies or organisations.
Within the general cognitive–behavioural field, Reference Tarrier and CalamTarrier & Calam (2002) have similarly called for explicit incorporation of systems theory and epidemiological and social context into cognitive–behavioural case formulation not only with younger people but also in general use with adults. Generic adult cognitive–behavioural formulation templates have been developed and refined into specific formulation structures for specific psychopathologies, but they assume a state of developmental maturity and autonomy in terms of how the individual meets their needs. It is simply not appropriate to ‘extrapolate’ such adult models ‘downwards’ for children since they are in a process of developing cognitive and other dimensions of functioning, they exist in and are dependent on the context of their families/carers and physical and cultural environments, and they are learning to meet their needs within the context of their major attachment relationships. The BABCP's new standards of conduct for the practice of CBT state that therapists ‘should only practise in the areas in which [they] have appropriate education, training and experience’ (British Association for Behavioural and Cognitive Psychotherapies 2009). It is therefore not recommended, for example, that CBT therapists without core professional training and experience in working with systemic and developmental issues work alone with children and their families.
There is growing clinical experience indicating that systemic cognitive–behavioural formulation (Reference DummettDummett 2004, Reference Dummett2006; Reference DattilioDattilio 2005) can be used with children and their families to explore developmental, attachment, interpersonal, family and wider-system processes (e.g. care and support networks) using core cognitive–behavioural techniques. Although these approaches are yet to be formally evaluated, in clinical practice systemic cognitive–behavioural formulation provides a basis for understanding problems and tailoring a therapeutic package to address both individual and systemic factors relating to a particular child. Specifically, such formulation enables working not only with the child as an individual but also with the child and their parents/carers together, with families and with wider systems using core cognitive–behavioural techniques in the systemic context. Psychological phenomena more traditionally expressed through other psychotherapeutic approaches can be explicitly worked with within the systemic formulation by expressing them in cognitive–behavioural terms. Such phenomena include repression, projection, transference and the processes of experiencing, for example, the depressive or paranoid–schizoid positions. In day-to-day clinical practice, systemic cognitive–behavioural formulation can be used to tailor packages of therapy to suit a range of presentations, as required for generic use throughout CAMHS. This approach has also provided a useful integrative model for therapist training.
Concepts and processes fundamental to CBT
Cognitive–behavioural therapy aims to promote self-help by helping clients learn to find and evaluate their own solutions to both present and future problems (Box 1). Formulation is a dynamic process undertaken jointly by therapist and client that promotes a collaborative (rather than expert-led) therapeutic relationship with sharing of the responsibility for change (Box 2).
BOX 1 Core features of CBT
-
• Formulation-based, empirical
-
• Collaborative therapeutic relationship promoted through use of guided discovery by Socratic questioning style, with appropriate sharing of responsibility for change
-
• Structured and problem-focused, teaches problem-solving
-
• Integrates cognitive and behavioural strategies
-
• Assumes that cognitions (not simply events) determine outcomes
BOX 2 The cognitive–behavioural formulation
-
• A hypothesis or working model/representation of the major processes of cause and effect linking cognitions, thoughts, behaviours, moods and bodily symptoms in causing and maintaining problems
-
• Usually written, but can be visual (imagery) or verbal – whichever has most relevance and utility for the client
-
• Collaboratively derived on a case-by-case basis through a process of guided discovery
-
• Testable, so that the client/family can confirm that this is an accurate reflection of their difficulties
-
• A template from which to derive interventions and to predict consequences, positive and negative, of any change
-
• Helpful in refocusing therapy and for exploring difficulties in therapy
The template for a cognitive–behavioural formulation for an individual client is based on the Beckian cognitive model and the premise that in any problem situation associated with dysphoric mood there will be four functionally distinct components of response (affective, cognitive, physiological and behavioural) that can be explored with the client (Fig. 1). These four systems of response are interdependent (interacting also with the social and physical environment) through many mechanisms of cause and effect (Reference RachmanRachman 1978), including operant and classical conditioning, physiology, social learning and attachment processes.
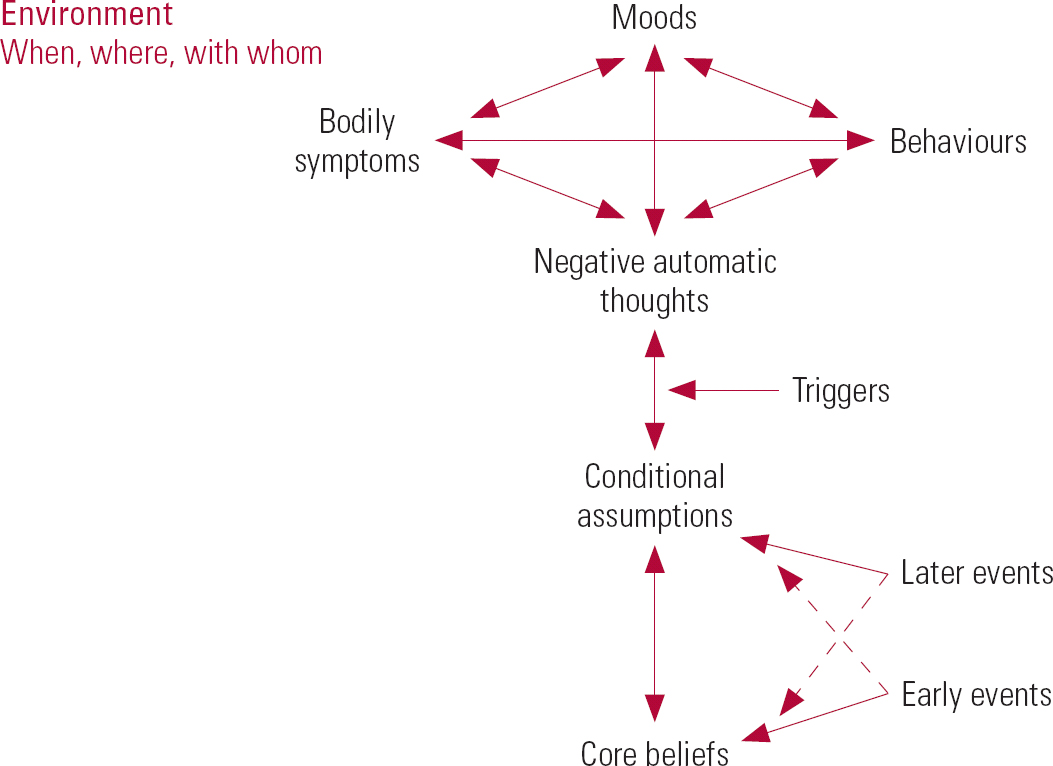
FIG 1 A template for an individual cognitive–behavioural formulation.
The Beckian cognitive model (Reference BeckBeck 1979) postulates three levels of cognition: relatively unconscious ‘core beliefs’, which derive from early life experiences, lead to more consciously held ‘conditional assumptions’ and ‘negative automatic thoughts’, the latter being active at the ‘four systems of response’ level. Core beliefs and conditional assumptions are built up and reinforced, largely through social learning, within the context of the attachment relationships and family and cultural contexts of early life. They are therefore strongly influenced by dominant family and cultural narratives.
Core beliefs
Core beliefs are fairly absolute statements about the self (e.g. ‘I am strong/weak/unlovable’), about the world (e.g. ‘it is a dangerous place’) and about others (e.g. ‘they are stronger than me/will reject me’) that constitute an internal working model of reality. Since core beliefs may be positive or negative evaluations of self, environment and others, they can serve both adaptive and maladaptive purpose, but reactions to negative core beliefs tend to be associated with problem situations.
Conditional assumptions
Conditional assumptions are expectations of the self or ‘rules to live by’. They have a defensive function in relation to negative core beliefs and have often had an adaptive function at an earlier stage of life (e.g. they have led to submissive or pacifying behaviours that have reduced persecutory attack in a hostile environment), but are less suited to present circumstances. Conditional assumptions take the form of either sympathetic or complementary (e.g. opposing but reinforcing) reactions to experience. They are expressed in ‘if …, then …’ terms, for example: ‘If I do everything perfectly, then I am worthwhile’ or ‘If I always keep other people happy, then I am lovable’. In day-to-day problem episodes, ‘trigger situations’ activate conditional assumptions, resulting in relatively conscious, here-and-now, situation-specific negative automatic thoughts that function at the four systems of response level. The thoughts are often distorted but are ‘automatically’ believed because they are mood congruent. They lead to the affective, physiological and behavioural components of problem response.
Vignette 1
A young person grew up with one parent who usually shouted when upset and one parent who (owing to underlying but unacknowledged mental health difficulties of their own) became rapidly overwhelmed by any upset in the family. She developed difficulties when, in adolescence, she was unable to advocate for her needs, particularly in peer relations. She discovered in therapy that she had unconsciously adopted the rule ‘never get anyone upset, even if it means I don't get what I need’. She was able to make changes to this once she had consciously considered the origin and present functionality of this rule for living.
Collaborative building up of cognitive–behavioural case formulation
The case formulation is started at the very beginning of therapy and is built up in stages and refined collaboratively by client and therapist as assessment and therapy progress. It is achieved by means of recent-event (also called four-systems) analysis, a fundamental technique in CBT that uses Socratic dialogue (below) to explore the client's affective, cognitive, physiological and behavioural reactions during problem episodes and also, as therapy progresses, their less conscious underlying core cognitions. In recent-event analysis, clients are encouraged to identify and separate their four-systems responses in recent ‘typical’ examples of the problem and to explore whether and how these responses are causally linked. This is a powerful tool for engaging with children, since it allows them to relive recent problems in session in a powerful fashion and to feel ‘heard’ by the therapist.
Vignette 2
A young person in care questioned following overdose initially gave blocking ‘Fine’ or ‘Don't know’ answers, since in her experience, ‘Adults usually don't really want to know what it's been like for me’. However, when asked to go through in detail the sequence of what she had been thinking and feeling about her situation at the time of the overdose, she felt more inclined to speak. She felt further encouraged as she and her interviewer shared an overt acknowledgment that her behaviour might be in some way understandable. She also reported that she was surprised that her interviewer ‘kept checking with me that they'd understood what I really meant rather than just assuming they knew’.
More important than simply giving the client a voice, recent-event analysis enables therapist and client to start to build together a formulation of the main links (usually circular) between the different components of the problem and any external (triggering or maintaining) factors. The formulation needs to be represented in a form that has most salience for the client. It is usually diagrammatic, but it may be narrative or expressed in symbols or imagery. The client's own language, images and experiences are used to represent elements of the formulation (Fig. 2). The degree of complexity reflects the shared understanding at the time and does not go beyond what is meaningful for the client (according to their developmental level and emotional state). Amplifying and maintaining cycles are collaboratively identified and predictions made about the possible consequences of change in any of the components.
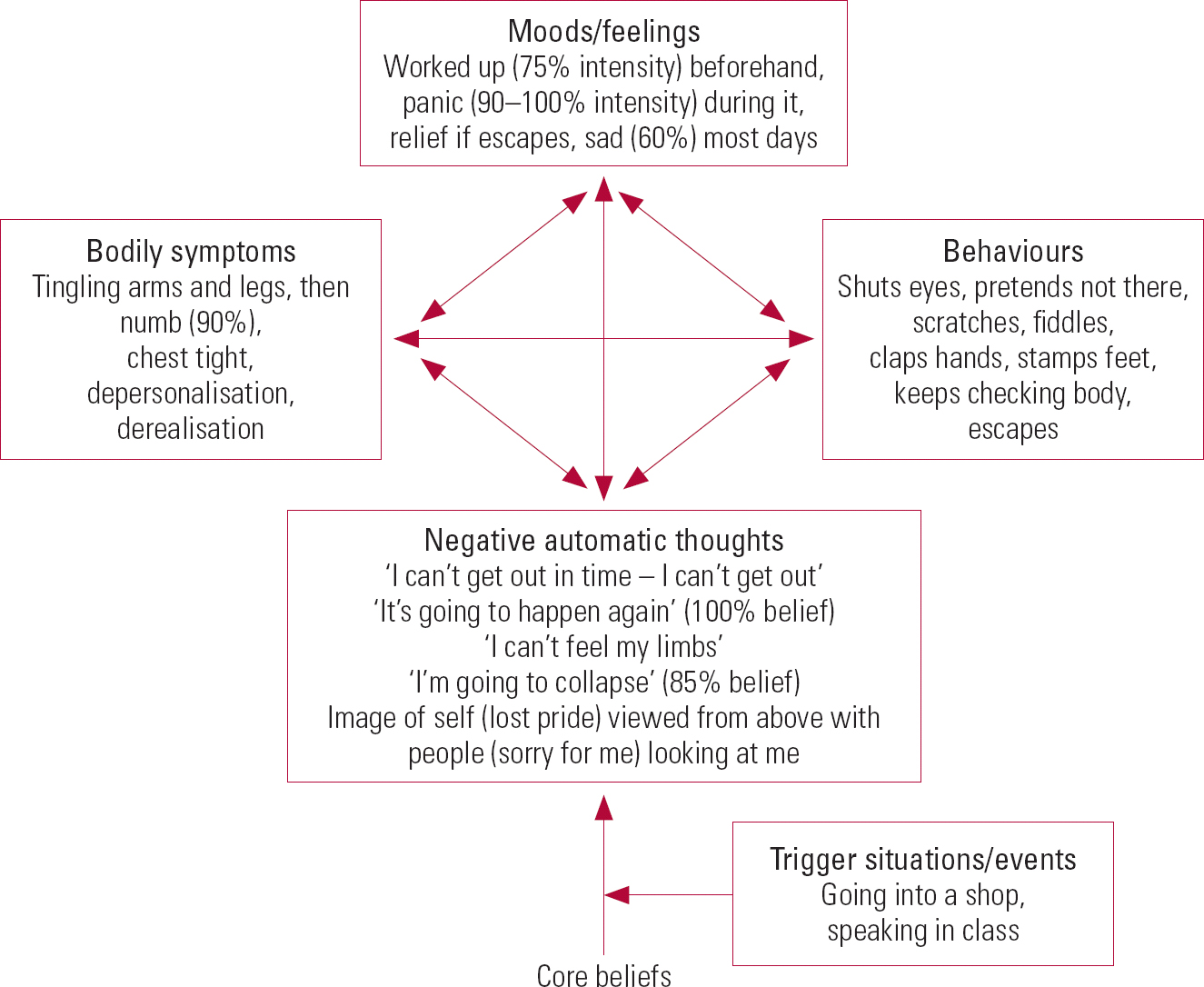
FIG 2 Sample recent event-analysis for a panic episode.
If an incomplete formulation does not yet account fully for a client's experiences (e.g. the persistence of a problem), this will be acknowledged collaboratively and further joint exploration embarked upon, as appropriate. With children, it is often evident at such times that a more systemic formulation (below) needs to be derived, perhaps necessitating incorporation of the experience of parents or members of the wider system. However, it may simply be that key cognitions or affects have been missed or undue emphasis has been given to those that, although present, are not intensely held but have been consistent with an overvalued therapist hypothesis, for example. Routine and regular use of case-based ratings of belief and affect intensity can greatly clarify which maintaining cycles predominate and regularly refocus collaborative attention. Specific links are made with past experience and these are integrated into the formulation. Helpful historical questions include ‘Can you remember the first time in your life this ever happened?’ and ‘Have there been other times in your life that have reminded you of this?’.
Therapy promotes skills of self-observation and monitoring and is effectively an invitation for the client, from within a supportive therapeutic relationship, to try out cognitive or behavioural change that empirically tests and further refines predictions from the formulation. Cognitive and behavioural interventions to address problems are selected collaboratively in accordance with the formulation. For example, the validity of cognitive deficits and distortions may be tested by encouraging the child to re-evaluate conclusions through guided self-discovery (below) that looks at the full breadth of their life experiences, rather than the narrow (mood-congruent) perspective taken at times of stress. Through this, the client is encouraged to create and evaluate more adaptive and functional explanations for themselves that reflect a ‘fuller picture’ of their experience. For example, ‘I'm useless’ might become ‘Although I often feel useless and that I can't do something I need to do, there are lots of times when I've done better than I predicted but not noticed!’
Vignette 3
A boy who repeatedly became overwhelmingly anxious before speaking in class developed a strategy of asking to be excused whenever he feared he might have to speak. (Removing himself from class had previously been condoned through a parent–school agreement for a known medical condition.) Although this defused his immediate anxiety, he came to think of himself as ‘completely useless’, because he could no longer imagine himself ever being able to speak in class, and also as ‘a dishonest person’, because of his deception. In therapy, an early piece of work on engaging him in behavioural change was to identify these self-beliefs and to compare them with wider evidence from his life (for example, the fact that he was usually uncomfortable about using dishonesty as a strategy and also that he was still able to talk assertively in other settings and had previously done so in class). From this wider evidence he was helped to construct an alternative belief that his strategy was not helpful, rather than that he was pervasively ‘useless or dishonest’.
Change can occur relatively rapidly at the level of negative automatic thoughts, but usually takes weeks or months at the deeper levels of conditional assumptions or core beliefs. Behavioural interventions include graded exposure to feared situations (or other anxiogenic stimuli) and identification and targeting of escape, avoidance and safety behaviours.
Socratic questioning
The Socratic questioning style (Box 3) is not by any means unique to CBT, but it is fundamental and indispensable in the practice of this intervention. As a therapist skill, Socratic questioning needs time, training and reflective practice to develop and is based on the observation that people change their thinking more readily if the rationale for change comes from their own insights, rather than from the therapist's (Reference Dattilio and PadeskyDattilio 1990). It establishes a collaborative therapeutic relationship and the process of guided discovery, in which curiosity is shared by therapist and client. It involves frequent summarising to reflect back what the client is reporting and to give opportunity for feedback on the accuracy of the therapist's understanding. Through self-reflection and evaluation, the client remains the acknowledged ‘expert’ in their own experiences and the therapist functions much more to assist memory retrieval, posing empirical questions to prompt self-discovery and self-suggestions for future interventions, rather than imposing hypotheses.
BOX 3 The basics of Socratic questioning
Questions are asked that:
-
• the client has the knowledge to answer
-
• draw attention to relevant information outside the client's present focus
-
• generally move between concrete/specific and more abstract/general
-
• apply new information to client's beliefs so client can: evaluate a previous conclusion construct a new idea
Systemic CBT formulation
In CBT with children, the formulation must encompass not only a four-systems perspective and the Beckian cognitive model, but also interpersonal and family factors, including attachment issues and systemic and cultural influences (Box 4). Furthermore, it must take into account developmental and biological factors and pragmatic factors such as the hierarchy of children's needs (primacy of physical and emotional security and nurturance, for example) that need to be satisfied before ‘higher-order’ therapeutic interventions are attempted. The formulation must be comprehensive but sufficiently succinct to be ‘user friendly’ and readily built up with the child or family from first principles.
Specific models incorporating systemic factors have been proposed for one or two specific presentations, for example eating disorders (Reference Fairburn, Shafran and CooperFairburn 1999), but not for more universal use with a wide range of presenting conditions. There were a number of early attempts at predominantly cognitively based family formulation models (Reference Schwebel and FineSchwebel 1992; Reference Smith and SchwebelSmith 1995; Reference DattilioDattilio 2005), but these did not explicitly incorporate all of the other (affective, physiological and behavioural) interacting components of response fundamental to cognitive–behavioural formulation. In clinical practice, clients (as individuals or families) often find great difficulty focusing on cognitive process (owing to the immediate dysphoria induced when bringing to mind distressing active thoughts) but are much more readily engaged in four-system exploration as an engaging way of reliving both positive and adverse individual and interpersonal experiences.
BOX 4 Additional criteria for formulation with children
-
• Incorporating interpersonal, family, attachment, systemic, cultural and developmental factors and intrinsic difficulties
-
• Being simple and understandable as a basis for communication between child, young person, family, therapist and other key persons or bodies, while still being comprehensive enough to include and make understandable all major processes of cause and effect that trigger and maintain difficulties
-
• Testable, so that the client/family can confirm that this is an accurate reflection of their difficulties
-
• A template from which to derive and select interventions and predict consequences, positive and negative, of any change (i.e. also predicts difficulties in treatment and likely timescales for change)
-
• Helpful in refocusing therapy and for exploring difficulties in therapy
Structure for systemic CBT formulation
Figure 3 shows a structure for systemic CBT formulation that can be used in clinical practice as a basis for collaborative exploration of a formulation with children and, when appropriate, families and wider systems such as support networks (Reference DummettDummett 2004, Reference Dummett2006). It should be noted that a structure such as the one shown here is never simply ‘presented’ to those involved: it is a template or potential framework for a systemic formulation that can be built up collaboratively with them, principally through four-systems analysis, to the level of complexity clinically indicated as assessment and therapy progress. As with an individual CBT formulation, therefore, it is necessary for ease of communication and understanding to keep the level of complexity of the formulation appropriate to the clinical situation. Key maintaining cycles are identified collaboratively in sessions through repeated Socratic recent-event analysis of both problematic and positive events and by ensuring that all key people involved in maintaining a problem are represented around the child by slowly building up the picture to include as many of the elements illustrated in Fig. 3 as is clinically appropriate. Clinical experience is required to ensure that priority is given to exploration of the elements of the formulation that are most significant in problem maintenance and to judge with the child when the experience and perspectives of other members of the system need to be sampled and incorporated, and also when such persons need to join the collaborative formulation process.
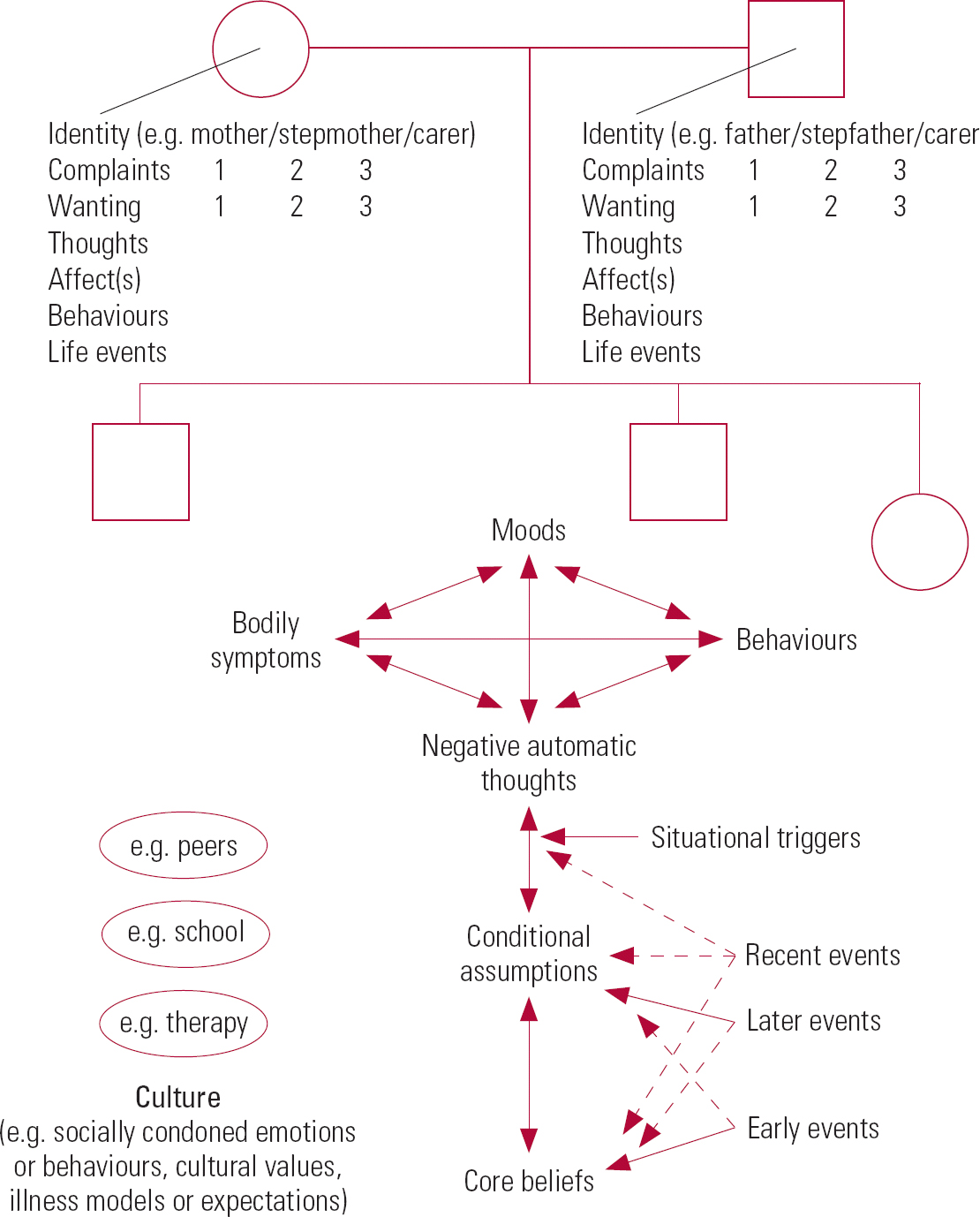
FIG 3 Systemic CBT formulation template for direct clinical use.
In the systemic case formulation, the child's individual formulation is central, together with a chronological list or time line (from bottom upwards, to allow linking with appropriate levels of cognition) of major life events from early on (age 0–5 years), later on (over 5 years), recently (since onset of symptoms or distress) and as present day-to-day situational triggers of acute difficulties. Surrounding this is a structure long valued in CAMHS practice – a genogram representing the key family relationships around the child. In addition, all other relationships involved in and possibly maintaining the child's problem(s) (for example, peers and other helping agencies, including the therapist(s)) are represented. Ideas of proximity are incorporated, since the child (and family in family working) will be asked to decide on the positioning of individuals in deriving this initial ‘sculpt’ of key relationships. The child's individual formulation is represented complete to the degree they have agreed in advance to share with the family (this may be very much simplified in the case of younger children). A key simplification is that only key (maintaining) components of the four systems of response (just key thoughts, emotions and behaviours) of other individuals are represented. Such key components are identified by repeating detailed recent-events analyses with the family on several occasions to see which elements occur and contribute most consistently and are reflected in the formulation as, for example, carer behaviours, thoughts and affects preceding, during and following problem episodes. Often, family influences need to be labelled in the formulation as carer core beliefs, commonly reflecting dominant family or cultural narratives and relating to their life experience. Major life events are therefore listed for the individuals most involved in maintaining the child's problem or most critical to the child for support, to hint at underlying influences on their cognitive processes.
Each key individual is asked early in therapy to give a prioritised problem list with their perception of severity for each item and to say which key changes or aims they wish for. These are included openly for each individual as a list of complaints and wants in the shared formulation (as shown in Fig. 3). They are also represented on the formulation as thoughts or as reflected in behaviours and emotional responses. This information has been found to be indispensable in making explicit to those involved differences in problem perception, desires and motivation for change, thereby helping family members to look at wider motivational issues and conflicts.
Cultural influences (e.g. culturally condoned emotions and behaviours, and cultural values, illness models and expectations) are listed in the formulation either in the surrounding environment or as cognitions of key individuals (if articulated as an account of their own thinking).
Use of systemic cognitive–behavioural formulation in practice
Components of a systemic formulation can be speculated on during treatment planning and supervision, on the understanding that this is hypothesising that will require subsequent testing against the client's experience and does not replace the collaborative process of formulation carried out with them. The template for systemic formulation offers a useful structure to represent often complex systems, allowing an at-a-glance overview highlighting major maintaining processes. This can be useful in supervision and focus case conceptualisation in therapist training.
The location and nature of major maintaining processes in the formulation will have implications for which interventions to prioritise and will also have prognostic importance: where symptom amplification is predominantly in the ‘here and now’ problem situation through positive feedback cycles between the four systems of response, change can occur relatively rapidly between weekly sessions. However, where key maintaining processes involve core beliefs, longer-term working will be required since change at these levels of cognition is much slower, often taking months or even years.
Where individual (intra-psychic) maintaining factors predominate, individual CBT will be the treatment of choice. However, in many CAMHS cases, maintaining and exacerbating processes are clearly predominantly interpersonal or even interagency, and systemic CBT will need to be offered in parallel with (or in preference to) individual therapy. Where parent or carer cognitions and consequent behaviours or affect are powerfully involved, the systemic intervention of choice is often to offer parallel parent/carer sessions to re-explore their cognitions, link them with past life experience and, through use of standard cognitive therapy techniques, consider their present functionality and accuracy.
Rating of belief levels (e.g. ‘I believed this 75% at the time’ on a 0–100% scale from ‘not believed at all’ to ‘absolutely believed with 100% certainty’) and affect-level ratings (e.g. 0–100% or 0–10, from ‘feeling not present’ to ‘the strongest I've ever felt it’) are very helpful in clarifying which processes are most active in problem situations.
Vignette 4
In a family four-systems analysis of recent difficult family times a teenager and her parents were individually asked to rate their emotional distress and belief levels for the thoughts that had most upset them during times they had identified as difficult.
What emerged was that the parental levels of distress had been consistently very high during times of difficulty. The parents' most intensely believed cognitions did include worry that their daughter was getting upset but far more consistent and intensely experienced than these worries were parental perceptions that their partner was misunderstanding their intentions or criticising their behaviour. In contrast, the teenager's distress in situations had been low, but she had a chronic irritation with her parents' arguing.
The rating of cognitions and affect enabled the parents to see which distressing thoughts (of the wide variety of cognitions active in the problem situation) had been most active in leading to their emotional responses in the situation. Instead of being linked to accurate perception of their daughter's emotional state, they were most intensely linked to relationship difficulties, which they subsequently chose to address in marital therapy.
A systemic perspective can be used when working on an individual basis, in carer–child or family sessions, or in wider meetings with involved agencies and support networks. Whichever form of working is used, however, it is always explicitly based on systemic cognitive–behavioural formulation and uses the Socratic questioning style and processes of empirical exploration such as recent-event analysis to encourage self-reflection and guided discovery.
As implied above, the principle of sufficiency is important: detailed work needs to be focused only on those areas necessary for positive change, although all areas of the potential template need at least to have been considered so that important processes are not missed. This requires therapist and supervisor skill and experience.
In building up a systemic formulation in an individual session with a child or in a family session, the area of the formulation most salient to the material being explored in the room should be built up to a degree of complexity and level of communication appropriate to the clinical setting. The formulation can be developed in a greatly simplified form, starting with a blank piece of paper or simple self-statement, with the child and/or family slowly building it up from reflections on their own experience. Ideally, it should be revisited and repeatedly re-derived through recent-event analysis for subsequent similar problem situations over time to clarify which processes usually predominate. For example, in individual session with a child who has come to understand ‘I shout because I'm afraid’, further exploration might be restricted to adding ‘Dad gets cross if I shout’. More insightful wider work around this basic formulation can then be explored with the wider family or, for older children, with the children themselves, to yield more complex systemic processes of cause and effect and inform an evolving systemic formulation.
A wider exploration with the family of Billy, who suffered panic attacks, might yield a much fuller picture (Fig. 4) than individual formulation (Fig. 2) alone. Interpersonal recent-event analysis using Socratic dialogue either with the whole family or just with central players is carried out to tease out and represent on the formulation not only the experience of all individuals involved in a recent problem situation, but also to explore with the whole family system how the family or wider system in its entirety is functioning. Thus, Socratic recent-event analysis of both problem and positive events can form the foundation of a collaborative systemic process wherein the family (and/or wider system agencies, as required) can explicitly explore systemic processes without undue emphasis on any individual and consider systemic possibilities for change.

FIG 4 Systemic case formulation for 13-year-old Billy, referred with panic symptoms.
In individual sessions, it is often helpful to encourage children to look outside themselves because they often come to therapy with a predominantly internal (e.g. self-blaming) focus. Looking at the history and interactional processes of their family and also at the helpfulness or otherwise of others' present reactions provides not only a broader understanding of difficulties but also an interactional understanding of what is necessary for change (for example, where they have expected too much of themselves when others need to change too).
Vignette 5
A boy had been labelled by himself and his family as ‘a liar’. There were indeed concrete examples of times when ‘things he had told his father’ had led to intense family distress. Faced with this partial picture of the family situation, he and his family had concluded that he was indeed ‘responsible for all upset at home’.
In individual sessions, he was encouraged to describe the wider family situation in four-systems terms, highlighting the behaviour, apparent feelings and (where known) thoughts not only of himself but of those around him. It was also suggested that he consider not only the helpfulness (or otherwise) of his own responses but of the responses of other family members too. This revealed that his father had moved out of the family home and that the older children and the mother now believed themselves to be a fully independent family unit. All the others had chosen to no longer communicate directly with the father, but the boy had chosen to still see him.
He recounted times he had ‘lied’ to his father and acknowledged that what was actually happening was that he was not daring to contradict distorted beliefs his father held about his mother. He identified active intense beliefs at these times that ‘Dad might have a breakdown if he's upset too much’ and that ‘Dad might fly off the handle if I upset him’. It was acknowledged that it would have been very difficult for him to have behaved differently faced with these circumstances.
After considering the contributions of other family members together with his own, he was asked to re-complete a ‘responsibility pie’ for upset in the family. He then rated his own contribution (originally seen as ‘nearly 100%’) as much smaller, ‘possibly smaller’ than that of other key players. He was subsequently better able to articulate this perspective to his family.
In family working, the co-construction of new meaning that occurs in shared recent-event analysis is emphasised. Family members are encouraged to consider initially their individual perspectives at times of difficulty but then, together with each other, to re-script more complete conclusions or narratives that reflect the fuller family experience. Family members need to feel sufficiently comfortable and ‘safe’ with sessions and with the relationships in the room to drop their habitual defences and reflect not only on the experiences and reactions of others but also on those of themselves, and at times to voice extreme personal reactions. For this reason positive events are usually considered first.
Vignette 6
When the members of a family were asked to consider together what they would choose to do on a family holiday, there was a natural discrepancy of opinion and wishes. After this was brought to their attention, they became less inclined to see differences of opinion that arose in difficult situations as a matter of concern. They had acquired greater ability to recognise differences of opinion as being a normal part of life, rather than signifying underlying malicious intent (‘She's just saying that to spite me’) or ‘proof that we're never able to agree’.
A non-judgemental stance is implicit in the Socratic questioning style employed and much normalising is carried out to reflect how people's responses are understandable given what they perceived at the time or had experienced previously. Family members are often invited to keep their reflections private if they wish, but acknowledgement is made of the need to share experience to allow them to hear each other and together create a new understanding of the ‘fuller picture’.
Vignette 7
The parents of a teenage boy who had a history of extreme refusal to attend school identified a particular Sunday night as having been ‘very difficult’. The boy and his parents were invited to carry out four-systems analyses of the episode, first as individuals and then as a family, sharing, if they felt comfortable, their thoughts, feelings and behaviours during and after the episode to see whether any new understanding emerged.
The parents reported that their son had come to them on the evening in question in an apparently distressed state. The mother reported having had an immediate surge of terror and fear (95% belief level) that he might self-harm. She had consequently avoided further conversation and ‘spent the evening on egg-shells to avoid any further distress’. The father reported an immediate feeling of frustration and impotence and the belief that he would be the person expected to ensure school attendance the next day and that his wife would blame him when he could not do so. He described ‘going into a rage’ and leaving the house. In contrast, their son (who had gone to school on the Monday morning without problem) initially failed to recall the incident at all, but then remembered that he had actually gone to ask his parents where to find something in the house and that he had in the end gone to find it unaided as they had seemed to be arguing about something.
As the family gradually shared their experiences, all in the room (including the therapist) were surprised to hear the expectations each had had of each other on that occasion. Both parents acknowledged surprise and perplexity but then relief to find that the beliefs about the evening that had coloured their emotional state for days had had no basis in fact. Further exploration revealed individual historical reasons underlying both parents' reactions on this and other occasions.
Many family narratives or ‘myths’ function at the conditional assumption or core belief level and thus the period needed for change can be predicted from the formulation as being of the order of months, rather than weeks. For this reason, family sessions are usually offered every 3 or 4 weeks over several months, much as with more traditional forms of family therapy. Although core beliefs are often shared, it can be difficult to locate within the family their primary focus: they may derive from one particular individual or be equally or predominantly derived from or maintained by external factors (peers, culture, religion or ethnic heritage). It is therefore important not to assume that all such beliefs are equally shared within the family. Family members should be given the opportunity to articulate their beliefs independently, in individual interview if necessary, since such beliefs can be strongly context-triggered, active when the person is with the family but much less active when with peers, for example.
As with many forms of therapy in use in CAMHS, it can be very helpful to incorporate positive strengths and abilities into the formulation to validate and positively reinforce adaptive coping styles and make explicit their function. Family sessions might include a therapist engaged in individual CBT with the child, who can act as an advocate for the child's perspective and redress any adult–child power imbalance in the sessions.
Consideration must be given to cultural factors and they may need to be worked with explicitly if they are active in problem maintenance, particularly as cultural beliefs are often held intensely but without awareness at the individual or family level. Similarly, therapists may be unaware of resources that are available within cultures in which they have not themselves lived.
Vignette 8
In a family that had recently arrived from abroad, a teenager presented with anxiety and extreme social withdrawal. He responded well to individual CBT focusing particularly on the use of safety behaviours and avoidance. However, one particular difficulty in the recovery period was the high level of anxiety his mother had whenever he dropped his safety behaviours and tried to habituate even to low levels of anxiety. The therapist explored with her (using an interpreter) her emotional reactions and thinking at these times. It was revealed that on coming to the UK she had been overwhelmed by discrepancies between cultural norms and narratives in the UK and those of her country of origin and this had led to a pervasive belief that her family could ‘never fit in and would always be outsiders’. This belief was particularly reinforced (‘proven to me’) when her son experienced social discomfort. In such situations, her culturally determined role as a woman and his mother was to try to help him feel better immediately, and she had little sense of her right to question or potential ability to change wider maintaining factors within the family (for example, culturally determined values such as gender roles). Consequently, she felt compelled to ‘rescue’ him from situations, effectively encouraging the use of safety behaviours and avoidance, even when he had initially resisted using them.
Systemic formulation and cognitive–behavioural working with outside agencies
A systemic formulation is a useful means of communication in working with outside agencies. In meetings with families and/or wider support networks a formulation can be built up through Socratic dialogue using a white board, for example. Key family and support individuals are usually identified first, and then participants carry out a four-systems exploration of interacting thoughts (particularly expectations, priorities and organisational discourses), behaviours and affect (e.g. discomfort triggered by organisational imperatives). The time line of life events provides a useful reference, particularly to proximity of loss for children in care.
Vignette 9
A 7-year-old in care and from a rejecting family of origin was faced with removal from a third residential placement, where he had made some progress over the year. This was explicitly reflected on in four-systems terms during interagency planning sessions in which participants shared observations on his behaviour and his expressed thoughts and feelings about himself, his carers and the future.
It was clear that with successive changes of placement his ability to perceive relationships as enduring and his sense of self-efficacy were reducing and his tendency to use extreme (aggressive or defiant) behaviour when feeling insecure about his future was increasing. Nonetheless, he had made encouraging behavioural change and expressed positive beliefs about his carer and himself in the current placement, but as in previous placements this was now less evident as his security there was threatened. Wider Socratic dialogue elicited key cognitions of agency workers managing his care and revealed the potency of interagency conflicts, organisational narratives and wider political imperatives in arousing discomfort in those making decisions about the child's care. Those present expressed relief in having these explicitly acknowledged, saying that they had been largely unconscious of many of these factors. They felt more enabled in their thinking now that these factors were ‘on the table’ to be weighed explicitly against other material in making any further decisions.
It may be that focused misperceptions or expectations held by one part of a child's support system cause particular problems but are amenable to rapid change.
Vignette 10
A school complained that a pupil with an autism-spectrum disorder was ‘obsessed’ with upsetting one of his peers. His mother could not understand why the school kept reporting aggression towards this child, as she had often specifically questioned her son and not found that he had any particular thoughts about the other child. Exploration of the school's experiences and staff perceptions revealed that they persistently saw him ‘targeting’ the other child in a regular group activity (assembly), in which his seating position was with the wall on one side and the other child as his immediate neighbour. Exploration with the boy, his mother and the staff involved revealed that he was confused and misreading social cues in this setting, particularly misunderstanding requests to stand as ‘time to go now’ and then getting frustrated with his neighbour for not moving. Because staff managing the activity were unaware of his primary difficulty in interpreting social cues in a group situation, his behaviour was being misperceived as focused aggression. This new understanding opened up a number of simple practical options to ease what had been an ‘incomprehensible’ problem.
Incorporating development, attachment and insights from other psychotherapies
Recent-event analysis and wider-system cognitive–behavioural formulation allow children and families to explore processes more commonly explored through other psychotherapeutic modalities by expressing in cognitive–behavioural terms the phenomena experienced. Repression of incongruous memories or images can be incorporated into the formulation as dysphoric elements at core belief level. The projective processes of object relations theory may be represented as cognitions at core belief level (e.g. ‘She always criticises me’) or negative automatic thoughts in the acute problem situation (e.g. ‘She is criticising me again’). Similarly, the experience of the paranoid–schizoid and depressive positions can be expressed in four-systems terms. Transference and countertransference processes may be located in the formulation as relationship-focused cognitions and consequent affect(s) and behaviour(s), and cultural influences may be represented in the formulation as articulated cognitions of key individuals. Figure 5 illustrates how sequences of interacting attachment-related behaviours and affects can be observed. Together with mediating cognitions, they can be expressed in four-systems terms and incorporated into the systemic formulation template.
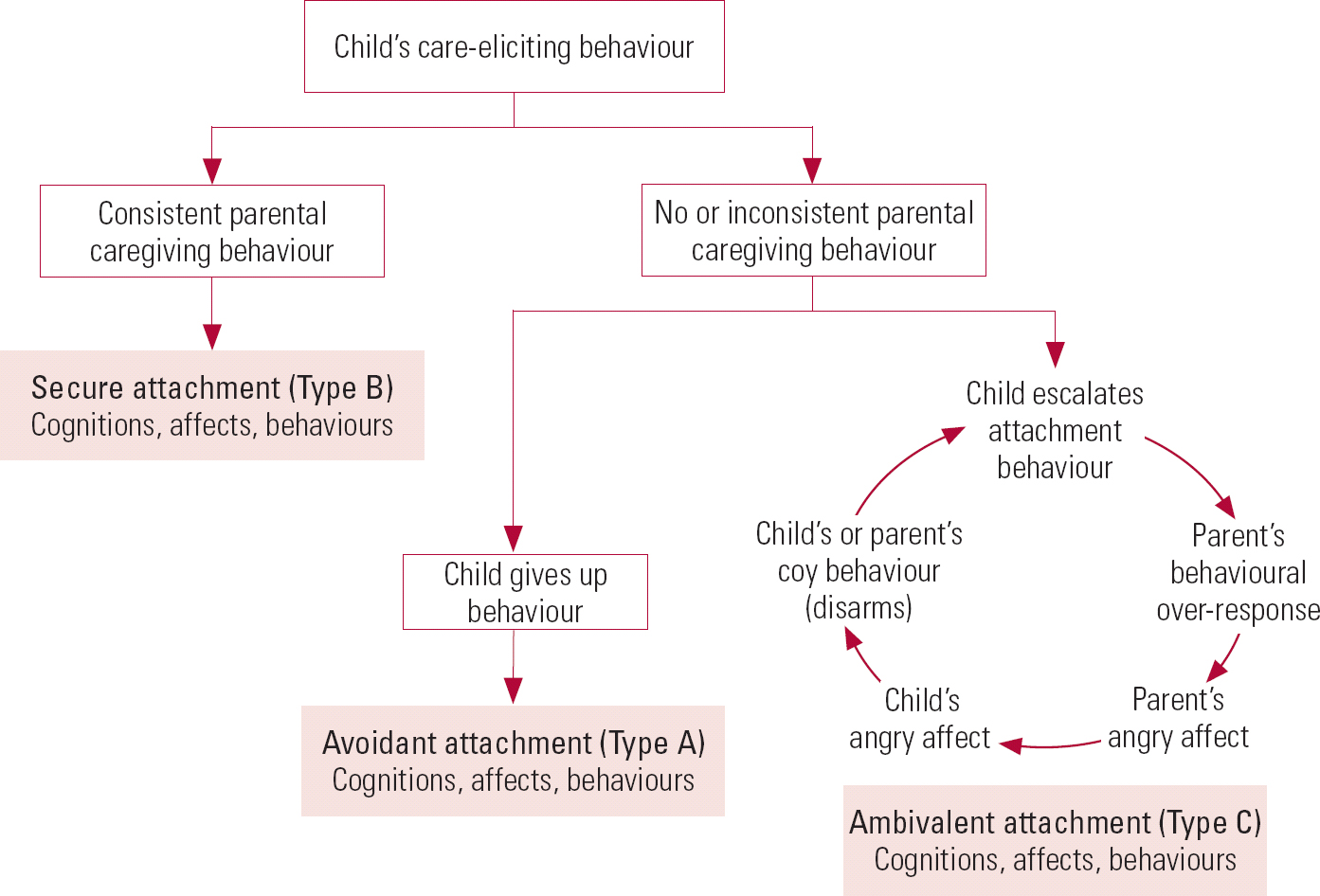
FIG 5 The major attachment patterns, expressed in four-systems terms.
Developmental and biological factors are accommodated and represented in the systemic template by starting with, on a case-by-case basis, the clinically observed ‘primary’ functional deficit in a system of response or cognitive level for the individual concerned. For example, with attention-deficit disorder, the primary deficit may be noted to be a cognitive deficit in pre-planning, in consequential thinking or in both, or to be impulsive behaviour or general lack of attention to social cues. By working through the formulation with the child and/or family, the consequences of this (poor self-esteem, peer rejection, etc.) can be identified, together with other, possibly maintaining or exacerbating, factors such as parental cognitions (over-anticipation of maladaptive behaviour) or behaviours (over-control). This can similarly be carried out for pervasive developmental disorders, specific intellectual and physical difficulties or simply to accommodate the child's present developmental level and to highlight the appropriateness or otherwise of the family's or school's expectations.
Vignette 11
The family of a boy with attention-deficit disorder could not initially see why he was ‘so angry with people all the time when we're doing everything to help him’. The therapist encouraged them to reflect on their own expectations of him and the ‘pros and cons’ of how people around him behave towards him. It became clear that people often ‘took control of him early in case he makes trouble’ when this was in fact unnecessary as he had had no intention of upsetting others and had simply been enjoying their company or even trying to help. The family realised from this that they were tending to over-anticipate malicious intent on his part. They could see how he was increasingly coming to believe ‘No one trusts me, everyone thinks I'm bad whatever I do and no one lets me do anything even when I can’. His emotional reactions were then entirely understandable to his family.
Examples of inaccurate or rigid cognitive responses (e.g. in some intellectual disabilities) or motor responses (e.g. in dyspraxia) are noted in the formulation under the appropriate system of response. Their effects in terms of other people's perceptions, expectations and behavioural responses can then be traced through the systemic formulation.
Summary
Formulation is the foundation of empirical therapy and is a core feature of CBT. Growing clinical experience reveals that formulation-based CBT working can be extended to systemic process working that incorporates developmental level, attachment processes and insights from other psychotherapies. The approach described in this article has been derived from empirical application of core cognitive–behavioural theory and processes to working on a systemic basis. It appears to offer a comprehensive systemic framework that can be used with individuals, carer–dependant dyads, families and when working with wider systems. It provides a structure that has been useful in supervision and therapist training. Although this approach is yet to be formally evaluated, in clinical practice there is growing experience that it opens up new ways of understanding and opportunities for change.
MCQs
-
1 Cognitive–behavioural therapy:
-
a is empirically based
-
b is directive
-
c is solely an individual therapy
-
d does not address the therapeutic relationship
-
e is a purely ‘here and now’ therapy.
-
-
2 The four systems of response are:
-
a cognitions, bodily symptoms, emotions and social context
-
b independent of each other and this is reflected in the formulation
-
c the same for every family member in a particular situation
-
d explored through recent-event analysis
-
e usually balanced so that no one or two elements predominate.
-
-
3 Treatment planning in CBT with a child or family should be based on:
-
a recent-event analysis only
-
b sharing with the family the full potential systemic formulation in all its complexity
-
c Socratic questioning, allowing the therapist to tell the family what they need to do
-
d guided discovery, allowing the therapist to tell the family where their thinking is distorted
-
e systemic formulation.
-
-
4 Effects of parents' cognitions cannot usually be adequately addressed through:
-
a individual therapy with a child
-
b parent–child sessions
-
c individual formulation without reference to the client's perceptions of others
-
d use of self-help materials
-
e professionals' meetings based on systemic formulation.
-
-
5 Service provision must recognise that:
-
a practice of CBT does not require ongoing expert supervision
-
b there is a significant core body of theoretical knowledge and skills training in CBT
-
c any psychiatrist's or psychologist's core professional training will have given them sufficient training to practise CBT
-
d any psychiatrist or psychologist can offer CBT supervision
-
e CBT cannot address long-standing or unconscious emotional conflicts.
-
MCQ answers

| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | t | a | f | a | f | a | f | a | f |
| b | f | b | f | b | f | b | f | b | t |
| c | f | c | f | c | f | c | t | c | f |
| d | f | d | t | d | f | d | f | d | f |
| e | f | e | f | e | t | e | f | e | f |
Acknowledgement
I thank Professor David Cottrell for his comments on an earlier draft of this article.









eLetters
No eLetters have been published for this article.