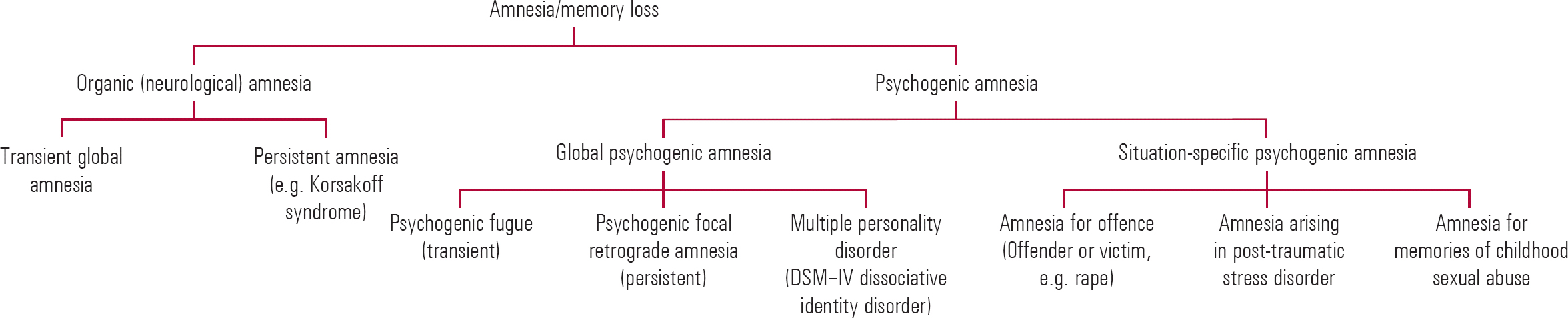
Amnesia (Fig. 1) has been defined as ‘an abnormal mental state in which memory and learning are affected out of all proportion to other cognitive functions in an otherwise alert and responsive patient’ (Reference Victor, Adams and CollinsVictor 1971). Memory impairment can affect the learning of new material (anterograde amnesia), owing to impairments in the encoding, storage or retrieval stages. It can also affect the recall of previously acquired memories (retrograde amnesia), which might involve personal experiences (episodic memory), general information (semantic memory) or perceptuomotor skills (procedural memory). Psychological factors can cause both anterograde and retrograde memory loss (or a combination of the two).
Types of psychogenic amnesia
Psychologically based amnesia includes the persistent anterograde memory impairment present in mental disorders such as depression, which in an extreme form can lead to depressive pseudodementia. Alternatively, it can cause transient or discrete episodes of retrograde and/or anterograde memory loss, which we refer to here as ‘psychogenic’ amnesia (i.e. loss not due to identifiable brain disease).
Why ‘psychogenic’?
A number of terms have been used to describe medically unexplained amnesia, including ‘hysterical’, ‘psychogenic’, ‘dissociative’ and ‘functional’. Each requires the exclusion of an underlying neurological cause and the identification of a precipitating stress that has resulted in amnesia. Unfortunately, the presence of amnesia may make it difficult to identify the stress until either informants have come forward or the amnesia itself has resolved.
Both DSM–IV (American Psychiatric Association, 2000) and ICD–10 (World Health Organization, 1992) favour the term ‘dissociative’ amnesia. Some have argued strongly for ‘functional’ amnesia as a description more acceptable to patients (Reference Stone, Carson and SharpeStone 2005). Others prefer ‘medically unexplained amnesia’. We favour ‘psychogenic’ amnesia, because it points to underlying psychological processes without assuming that any particular psychological mechanism is involved (a difficulty with ‘dissociative’ amnesia). Also, it does not specify whether the memory loss is produced (partly or entirely) consciously (‘factitious’ or ‘exaggerated’ amnesia) or purely unconsciously (‘hysterical’ amnesia). The term ‘functional’ amnesia has the problem that the amnesia could in many respects be considered dysfunctional. However, regardless of the term used, the question remains, at what point, in cases of doubt, should the clinician assume that a psychological stressor or a marker of neuropathology or brain pathology is the primary cause of the symptoms? A subsidiary to this is, does the amnesia have both psychological and neurological contributions to its aetiology?
Types of global psychogenic amnesia
Psychogenic fugue
This is a syndrome of sudden onset, involving loss of all autobiographical memories, including personal identity. It is usually associated with a period of wandering, for which there is a gap in continuous memories on recovery. Fugue states usually last a matter of hours or days. There is anecdotal evidence that they are more common in wartime, particularly in soldiers about to return to the front. Psychogenic fugue is classified in DSM–IV as dissociative fugue.
Case 1 Psychogenic fugue
A 40-year-old woman ‘came round’ on the London Underground. She had approached a staff member, telling them that she had no recollection of who she was or what she was doing. The only clues to her identity were a bag with a few clothes and a letter that turned out to be addressed to someone else. Staff contacted the police, who took her to an accident and emergency department. After being medically cleared she was admitted to a psychiatric unit. Initially, she appeared depressed but this resolved with no medication. In an effort to trace her identity a picture was shown on national television, with no responses. An amytal interview was tried, again with no success. She was eventually discharged from hospital and the retrograde memory loss persisted. One year later, relatives in the USA sent a missing person poster to the UK police and she was traced. It emerged that, following a marital crisis in the context of an unstable marriage, she had disappeared from her home and taken a flight to the UK. She had a history of depression.
After obtaining a clear history from the family a second amytal interview was attempted and she did recover most of her retrograde memory function (Reference Kopelman, Christensen and ParfittKopelman 1994).
Three main factors may predispose to psychogenic fugue:
-
• precipitating stress such as emotional, relationship, marital or financial problems
-
• depressed mood, sometimes with suicidal thoughts
-
• a history of a transient organic amnesia: some studies report that more than half of affected individuals have experienced severe head injury (Reference Berrington, Liddell and FouldsBerrington 1956).
Psychogenic focal retrograde amnesia
This is a persistent state in which the individual loses all retrograde memories. The amnesia is described as ‘focal’ because anterograde memory is relatively or completely spared. There is considerable controversy concerning whether a brain lesion in isolation can ever cause this dissociation between anterograde and retrograde amnesia (Reference KopelmanKopelman, 2002a). Often, spouses or close family members are not initially recognised and later the patient claims to have relearned who they are. Clinically, there may be two aetiological routes to the appearance of this syndrome. The first is following a typical fugue with wandering and loss of personal identity, when disproportionate retrograde amnesia persists. The other is after a minor brain insult such as mild concussion in a predisposed person. These cases are often difficult to manage, both because of the coexistence of minor organic, psychological factors and the possibility of financial compensation for injuries, and because the underlying stressors are often not obvious on initial inquiry. In both types of aetiology abnormal illness behaviour may arise and be reinforced by the gains derived from the emotional and practical support of family, friends, helping professions and the welfare system.
Case 2 Psychogenic focal retrograde amnesia
‘I put things in boxes, I choose to put them in the back of my mind. I've always done that’. These are the words, during treatment, of a 62-year-old man who collapsed at work with a transient right-sided weakness and a complete loss of autobiographical memory. On admission, he was disoriented in time and place as well as person, and there was a mild loss of power in the right arm and leg with an equivocally up-going right plantar response. A computed tomography (CT) scan was normal but a magnetic resonance imaging (MRI) brain scan showed evidence of a few pinpoint regions of altered signal bilaterally, consistent with a history of previously diagnosed hyperlipidaemia and diabetes. However, the physicians attending this man felt confident that his memory loss was entirely disproportionate to his neurological signs, which rapidly resolved. The patient did not recognise his wife, and he could not remember the names and ages of his children. He claimed to have relearned this (personal semantic) knowledge about his life and that ‘each day I remember more of the day before’. On formal tests, he showed severe and extensive autobiographical memory loss, with intact anterograde memory. When first seen, he and his family were angry at any suggestion that there might be a psychological component to his memory loss. However, during the succeeding weeks, his wife provided information about his difficult childhood and subsequent emotional problems. The initial onset had occurred after the patient had been confronted about ‘moonlighting’ in two employments and his dismissal from both. After being seen on a regular basis for several weeks, he was more willing to accept a psychological contribution to his amnesia and, following an amytal interview, virtually all of his memories were recovered.
(This patient is now out of contact. A previous brief report was published (Reference KopelmanKopelman 2000) with his permission. Identifying details have been changed.)
Multiple personality disorder (DSM–IV dissociative identity disorder)
A key symptom in this disorder is some degree of between-personality amnesia. How much access each personality has to the others' memories is variable (for a review see Reference Kihlstrom, Schacter and CermakKihlstrom 2000). A recent study (Reference Huntjens, Peters and WoertmanHuntjens 2006) showed evidence that items claimed not to have been remembered in one personality did influence the choice made later in a recognition task after a personality switch. In contrast to ‘simulators’, who tended to choose implausible alternative answers, the choice made was often a ‘near miss’ or plausible alternative to the correct answer. This led the study's authors to conclude that there is no evidence of a memory retrieval problem but instead that individuals with dissociative identity disorder hold incorrect beliefs about their memory functioning. How much this disorder is the result of iatrogenic influences on patients already vulnerable to psychogenic memory disorders is still a matter of debate (Reference MerskeyMerskey, 1995).
Differentiation of transient psychogenic and organic amnesia
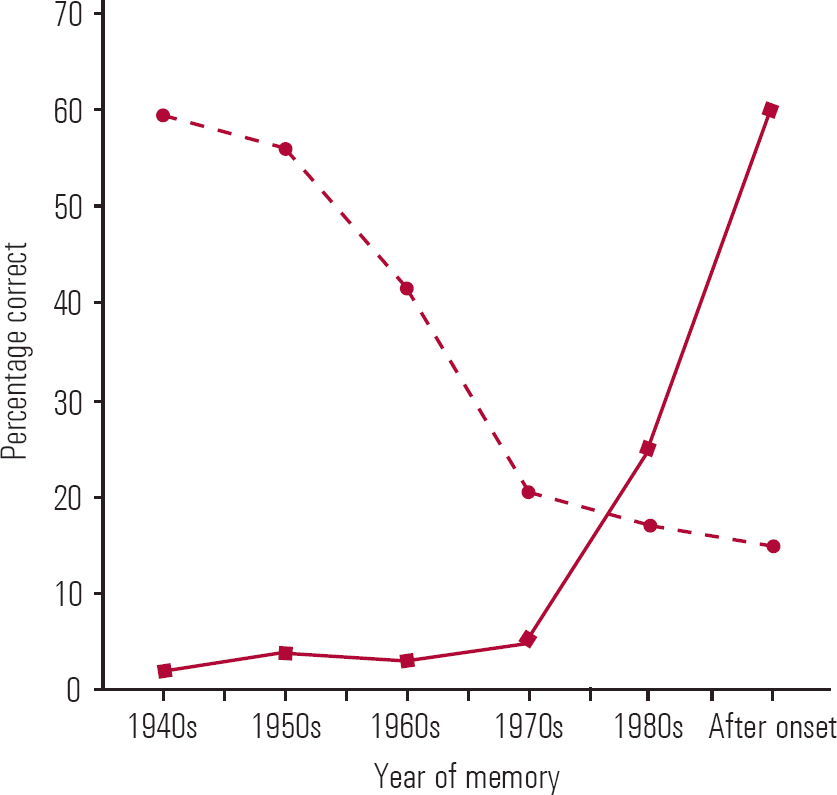
The differential diagnosis of psychogenic fugue is described in Box 1 (Reference Kopelman, Baddeley, Kopelman and WilsonKopelman 2002b). The features common to, and differentiating between, transient organic and psychogenic amnesias are shown in Table 1. The retrograde memory impairment in a transient neurological amnesia such as transient global amnesia, or in a persistent one such as dementia or Korsakoff syndrome, usually follows Ribot's law: recently learned material is more affected than earlier memories. This leads to a characteristic ‘temporal gradient’ when retrograde memory test performance is plotted against time. The memory impairment in psychogenic amnesia, in contrast, characteristically shows a reversed gradient, with earlier memories preferentially affected (see Fig. 2).
BOX 1 Differential diagnosis of psychogenic fugue
-
• Alcoholic ‘blackout’
-
• Transient global amnesia
-
• Transient epileptic amnesia
-
• Epileptic fugue (rare)
-
• Post-traumatic amnesia following head injury
-
• Simulation/malingering
Transient global amnesia
Transient global amnesia is a syndrome of sudden-onset anterograde and variable retrograde amnesia, with repetitive questioning not associated with other neurological deficits. It usually lasts for a matter of minutes to hours, with complete recovery.
Its aetiology is poorly understood. One theory is that an upsurge in venous pressure, which could explain the association with emotional or physical stress, causes hypoxoischaemia in the hippocampus, an area of key importance for memory. There is an association with migraine in 25% of cases (Reference Hodges and WarlowHodges 1990). Hyperintensities in the hippocampus have been demonstrated on diffusion weighted imaging (Reference Sander and SanderSander 2005). Reference Hodges and WarlowHodges & Warlow (1990) found an epileptic basis for a small proportion of cases (7% of 153) and the term ‘transient epileptic amnesia’ was coined (Reference Kapur and MarkowitschKapur 1990). Here the attacks tend to be briefer and more recurrent than in transient global amnesia, they are associated with other seizure types and they usually respond well to anticonvulsants.
Assessment of psychogenic amnesia
Box 2 shows the salient features to be elicited in the history, mental state and physical examinations, and the investigations to be performed when assessing a likely psychogenic amnesia. Neuropsychological testing should be carried out whenever possible.
BOX 2 The assessment of likely global psychogenic amnesia
History
-
• Precipitant of amnesia
-
• Head injury? Stress?
-
• What memories are affected?
-
• Retrograde only, or anterograde also?
-
• Complete, or ‘islets’ of preserved memory?
-
• Is it confined to autobiographical incidents?
-
• Is knowledge of facts about oneself or facts in general (semantic memory) affected?
-
• Personal identity?
-
• Close family, spouse's identity?
-
• Repetitive questioning?
-
• How does it feel to the patient? Indifference?
-
• An insistence that ‘recovered’ memories have been relearned?
-
• Psychiatric history
-
• Somatisation, depression, other isolated and ‘unexplained’ physical symptoms?
-
• Medical history
-
• Previous transient neurological amnesia?
-
• Seizures?
-
• Alcohol/substance intake?
Mental state examination
-
• La belle indifference?
-
• Other hysterical symptoms or symptoms of somatising?
-
• Depression?
Physical examination
-
• Particular emphasis on the cardiovascular and neurological systems
Neuropsychological tests
-
• Anterograde memory may be relatively normal, with disproportionate retrograde amnesia
-
• Tests of retrograde memory (e.g. the Autobiographical Memory Interview) show a ‘reversed gradient’
-
• Tests of simulation can be performed: malingerers will perform worse than by chance alone
Investigations
-
• Complete dementia blood screen
-
• MRI
-
• EEG if relevant
Essential collateral history
-
• GP and hospital records
-
• Witness/family accounts
-
• Undisclosed stressors from family
Management of global psychogenic amnesia
The patient and family should be engaged sympathetically, avoiding confrontation. The patient often has coexisting depression and this should be treated. The disadvantages of the amnesia should be gently drawn to attention and the advantages minimised, and the patient should be encouraged to resume normal activities, including employment.
Interview under sedation
It has long been noted, anecdotally, that an interview under intravenous sedation (abreaction) can help recover memories in psychogenic amnesia (Reference HermanHerman, 1938). This is a controversial technique and its use in the UK is in decline (Reference Patrick and HowellsPatrick 1990). There are concerns about the suggestibility of individuals during sedation and the reliability of memories obtained (Reference Rogers, Wettstein and RogersRogers 1988). Adding to the controversy, the technique has been used to ‘recover’ memories of childhood sexual abuse, leading several international bodies to caution against its use in this particular situation (Reference Brandon, Boakes and GlaserBrandon 1997). Although problems remain, we would distinguish this use (hunting for specific, long distant abuse memories) from the use of amytal in the treatment of acute-onset non-neurological loss of recent (and remote) memories.
There are no randomised placebo-controlled trials of interview under sedation in psychogenic amnesia (Reference KavirajanKavirajan, 1999). Reference Lambert and ReesLambert & Rees (1940) compared barbiturates, hypnosis and supportive treatment in a group of 247 servicemen with hysteria, 56 of whom had amnesia. The groups were non-randomly chosen and the barbiturate group contained patients who had not recovered spontaneously or by interview without sedation. The authors noted that, although there was no difference in remission rates between the groups (82%, 75% and 88% respectively) in a post hoc analysis, interview under sedation was found to be ‘by far the quickest and the easiest method’ of recovering memory. Despite the absence of high-quality evidence demonstrating its efficacy and the controversy regarding its use, interview under sedation can still have a place in the management of psychogenic amnesia if it is used cautiously and without any attempt at making suggestions.
Conducting an amytal interview
As much collateral history from the family and other informants should be elicited as possible before proceeding and the interview must not be rushed into. It is best to arrange an in-patient admission for the interview, so that any psychological issues arising can be discussed with staff. Clinical impression suggests that sodium amytal is the most effective drug for this purpose; we have found that lorazepam has too slow an onset and midazolam is more difficult to titrate. Amytal can be more accurately titrated to gain greater control of the degree of sedation. It must be noted that amytal is unlicensed for this purpose and it is advisable to obtain written informed consent before the procedure. A protocol is available (Reference Perry and JacobsPerry 1982). The risk of respiratory arrest and the lack of a pharmacological antagonist are considerations and a crash trolley and oxygen should be readily available. Significant cardiopulmonary disease would be a contraindication. For guidelines on the safe use of ‘conscious sedation’ see American Society of Anesthesiologists Task Force (2002). Complications are rare; at a time when such interviews were more commonplace, a study reported 1 respiratory arrest in 500 amytal interviews, and this because the amytal was administered too quickly (Reference Hart, Ebaugh and MorganHart 1945).
The principle of interview under sedation is to reach a level of intoxication in which the patient is deeply relaxed but not asleep. This can be judged by getting the patient to count backwards from 50 until numbers are mixed up or skipped. At this point conversation about neutral topics can turn towards the amnesic gap, using clues gained from the history. Questions are as open as possible and leading questions should not be used (Reference Rogers, Wettstein and RogersRogers 1988). This level of sedation is maintained by slowly injecting more amytal until no further progress is made or the maximum dose reached. Information revealed is talked over again while the patient is recovering, to ensure that the memories are retained in awareness.
Prognosis
If the amnesia is long-standing and the family is enmeshed in a system that maintains the symptoms then it is difficult to change. The longer the amnesia has persisted, the less likely is complete recovery.
Memory complaints or a psychogenic amnesia may form part of a wider picture of somatisation disorder. If this is the case, efforts should be made to limit the number of investigations and doctors involved, and some form of regular psychological treatment should be instigated.
Situation-specific amnesia
Amnesia for offences
Offenders as well as victims of crimes commonly claim amnesia regarding the offence and psychiatrists can be called upon to comment on this. Cross-sectional studies have found that in 25–45% of homicides, 8% of other violent crimes and a small percentage of non-violent crimes, offenders claim amnesia for the offence (Reference KopelmanKopelman, 2002a).
Differentiation from underlying neurological conditions such as an epileptic automatism, post-ictal confusional state, head injury, hypoglycaemia, sleepwalking or rapid eye movement (REM) sleep disorder is important (for references see Reference KopelmanKopelman 2002a). Amnesia for an offence can also occur in alcohol intoxication, substance misuse and acute psychosis but purely psychological amnesia occurs most commonly in crimes of passion. In one series, 40% of offenders claiming amnesia on arrest for murder still had amnesia for the offence 3 years after conviction. They were less likely to deny the offence than a similarly convicted comparison group, thus providing some evidence that malingering was not the sole cause of their memory loss (Reference Pyszora, Barker and KopelmanPyszora 2003).
Post-traumatic stress disorder
The relationship between trauma and memory is complex, with some memories apparently enhanced and others forgotten. This forgetting is sometimes interpreted in terms of ‘peri-traumatic dissociation’, which is one of the diagnostic criteria for acute stress disorder in DSM–IV. However, it may also be the case that, when something extraordinary happens, we ask ourselves to recall far more detail than we would normally expect, and experience the shortfall as ‘gaps’ in memory (Reference KopelmanKopelman 2002a). The presence of head injury can complicate the clinical picture. With regard to the memory disturbance seen, amnesia predominates in head injury, and intrusive memories predominate in post-traumatic stress disorder (PTSD), where memory lapses are less common. The two could be seen to lie at the opposite extremes of a continuum.
One particular theoretical model proposes a dual-component memory system to explain memory of personally experienced traumatic events (Reference Brewin, Dalgleish and JosephBrewin 1996). On the one hand are verbally accessible memories (autobiographical memories) that have received some conscious processing and have been transferred to the long-term store. These memories can be retrieved either automatically or deliberately. On the other are the situational accessible memories responsible for trauma-related flashbacks and nightmares. These memories have undergone little conscious processing and involve the autonomic and motor responses at the time of the trauma. Because these memories are not encoded verbally they are difficult to communicate to others and to control, often being triggered by trauma-related cues.
Anterograde memory dysfunction has been demonstrated in people with PTSD and there are claims that they have a loss of hippocampal volume on MRI (Bremner 1999), which has been attributed to effects of glucocorticoids (Reference MarkowitschMarkowitsch 1996).
Childhood sexual abuse
Amnesia for childhood sexual abuse has been an issue of debate and can have important medico-legal implications. Doubts over the veracity of memories of such abuse that come to light during psychotherapy are expressed in the proposition of ‘false memory syndrome’.Footnote † However, even studies by protagonists of false memory syndrome (Reference Loftus, Polonsky and FulliloveLoftus 1994) show that some forgetting of abuse does occur.
As with PTSD, mechanisms have been proposed whereby such forgetting and subsequent (possibly erroneous) retrieval might occur (Reference SchacterSchacter 1996), particularly in relation to certain cues or triggers (Reference Andrews, Brewin and OcheraAndrews 2000).
Other common psychiatric disorders causing memory complaints
Cognitive symptoms are increasingly seen as part of the schizophrenic syndrome. A meta-analysis concluded that significant deficits were found in verbal recall (Reference Aleman, Hijman and De HaanAleman 1999). Performance on delayed recall tests by people with schizophrenia was one whole standard deviation below that of people without. Both post-mortem and structural MRI studies have shown people with schizophrenia to have smaller medial temporal lobes compared with controls (Reference Shenton, Dickey and FruminShenton 2001).
Depression is associated with both subjective complaints of forgetting and measurable deficits on anterograde memory tests (Reference Dalgleish, Cox, Kopelman, Baddeley and WilsonDalgleish 2002). In its extreme form, the picture may be of a pseudodementia, especially in the elderly. These deficits are at least partly corrected by treatment. Again, it is interesting that one meta-analysis concluded that there is evidence of reduced hippocampal volume in depression (Reference Campbell, Marriott and NahmiasCampbell 2004). Bipolar disorder, especially in older patients with multiple episodes, has been reported to be associated with measurable impairments on neuropsychological tests of memory, even when patients are in remission (Reference Savitz, Solms and RamesarSavitz 2005).
Another way of looking at these data is to suggest that psychopathology has a non-specific effect on memory. What is not clear is how much the cognitive deficits are directly related to the pathophysiology of each condition, how much is an epiphenomenon of the psychological condition, and whether and to what extent they are secondary to confounders such as medication or substance misuse. Well-designed prospective studies would clarify these issues.
What are the brain mechanisms of psychogenic amnesia?
There is evidence from ‘lesion’ studies that memories of emotional or traumatic events are processed differently from ‘ordinary memories’. In particular, emotional memories, especially those involving fear, may use amygdaloid circuits, whereas ‘normal’ learning involves other brain regions (Reference Fine and BlairFine 2000). The amygdala is a brain area richly connected to the emotional circuitry of the brain and the autonomic nervous system.
Lesions in the medial temporal and the diencephalic areas of the brain cause an amnesic syndrome with anterograde amnesia and also a variable degree of retrograde amnesia. Frontal areas are believed to be more involved in the effortful retrieval of autobiographical memories (Reference KopelmanKopelman 2002a). A few years ago, one of us (M.D.K) proposed a model of how brain systems and psychosocial factors interact to produce a global psychogenic amnesia (as in fugue or focal retrograde amnesia) (Reference KopelmanKopelman, 2002a). It hypothesises that stress affects a frontal/executive retrieval system, especially if there has been a past learning experience of an organic amnesia or the person is severely depressed. Stress sometimes has a direct effect on the medial temporal–diencephalic system, but if this remains unaffected new learning can continue, so that only the retrieval of past autobiographical information is impaired. Severe stress can also affect retrieval from the ‘personal semantic belief system’, resulting in the transient loss of personal identity. In situation-specific amnesia, it has been suggested that some aspects of forgetting are due to a narrowing of consciousness, with attention focused on central perceptual details.
Functional neuroimaging is offering insights into the brain mechanisms involved in psychogenic amnesia. Several functional MRI (fMRI) studies have been carried out in psychogenic amnesia. Although there do appear to be abnormalities in areas important for memory, the location and even the direction of the activation or deactivation has differed from study to study, making interpretation difficult (references can be supplied on request). Reference Anderson, Ochsner and KuhlAnderson and colleagues (2004) reported evidence that executive mechanisms can be recruited to prevent unwanted memories from entering awareness, and that repeated use of this strategy inhibits the subsequent recall of the suppressed memories. This research group went on to use event-related fMRI to investigate the neural substrates of these phenomena. They found that during the suppression of unwanted memories, poorer recall correlated with activation of the lateral prefrontal cortex and deactivation of the medial temporal lobe. Further research using event-related fMRI during autobiographical memory retrieval paradigms in patients with psychogenic amnesia will clarify the brain mechanisms associated with memory suppression.
Conclusions
We hope that this article has given the clinician knowledge of the range of presentations of psychogenic amnesia and a practical framework on which to base an assessment. This should allow differentiation between neurologically based amnesias and comorbid psychiatric conditions. Management may involve an amytal interview, but this should not be rushed into: first, a full understanding of the patient's underlying issues should be sought and any depression treated.
Psychogenic amnesia may result from the effects of stress on the frontal memory retrieval systems and inhibitory mechanisms, rather than from an effect on the medial temporal lobes or diencephalic structures, which are the usual sites of pathology in neurologically based amnesias. Functional neuroimaging is now allowing the investigation of the interaction of these structures during normal retrieval and suppression in memory tasks, and may eventually provide insights into the brain mechanisms underlying psychogenic amnesia.
MCQs
-
1 Psychogenic fugue:
-
a usually lasts a few months
-
b is increasing in incidence
-
c is commonly preceded by head injury
-
d is associated with repetitive questioning
-
e is rarely associated with a loss of personal identity.
-
-
2 Psychogenic focal retrograde amnesia:
-
a is never associated with head injury
-
b has a classic temporal gradient
-
c is associated with severe anterograde amnesia
-
d often causes repetitive questioning
-
e persists longer than fugue in the majority of cases.
-
-
3 The management of psychogenic amnesia:
-
a should always involve an amytal interview
-
b should involve the family
-
c should involve an element of confrontation
-
d will be made easier if the patient is encouraged to apply for social support benefits
-
e is more likely to result in a good outcome the longer the amnesia persists.
-
-
4 Transient global amnesia:
-
a shows a pattern of retrograde memory loss very similar to that of psychogenic amnesia
-
b is often associated with stressful antecedents
-
c is characteristically associated with abnormal EEG
-
d is associated with a loss of personal identity
-
e usually responds to anticonvulsants.
-
-
5 Amnesia for an offence:
-
a is commonly reported in shoplifting
-
b is caused by malingering in almost all cases
-
c is rare in homicide
-
d can result from an automatism
-
e persists in only a tiny minority once the trial is over.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | f | a | f | a | f | a | f | a | f |
| b | f | b | f | b | t | b | t | b | f |
| c | t | c | f | c | f | c | f | c | f |
| d | f | d | f | d | f | d | f | d | t |
| e | f | e | t | e | f | e | f | e | f |
TABLE 1 Differentiating transient organic and psychogenic amnesias
| Characteristic | Transient organic amnesia | Transient psychogenic amnesia |
|---|---|---|
| Is preceded by precipitating stress/significant life-event | Possible | Usually |
| Normal results in standard investigations (routine EEG, CT, MRI) | Possible | Usually |
| Loss of personal identity | Never in transient global amnesia | Always in fugue |
| Repetitive questioning | Common in transient global amnesia/transient epileptic amnesia | Seldom in fugue/psychogenic amnesia where there may be la belle indifference |
| Other symptoms/signs | Sensorimotor symptoms in transient epileptic amnesia | Wandering in fugue |
| Time–memory performance curve | ‘Temporal gradient’ of retrograde amnesia in transient global amnesia/transient epileptic amnesia | ‘Reversed gradient’ in psychogenic amnesia |
| Anterograde memory | Impaired | Often spared |
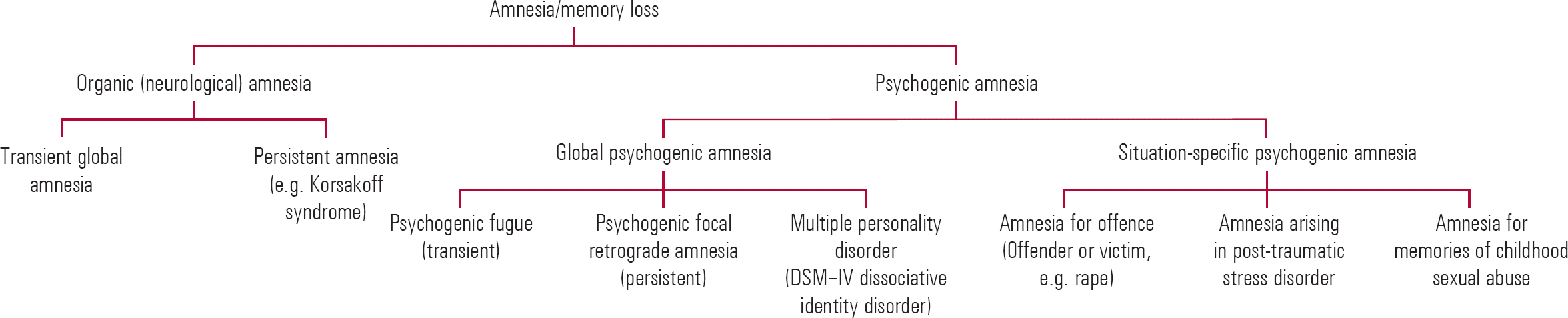
FIG 1 A partial classification of amnesia.
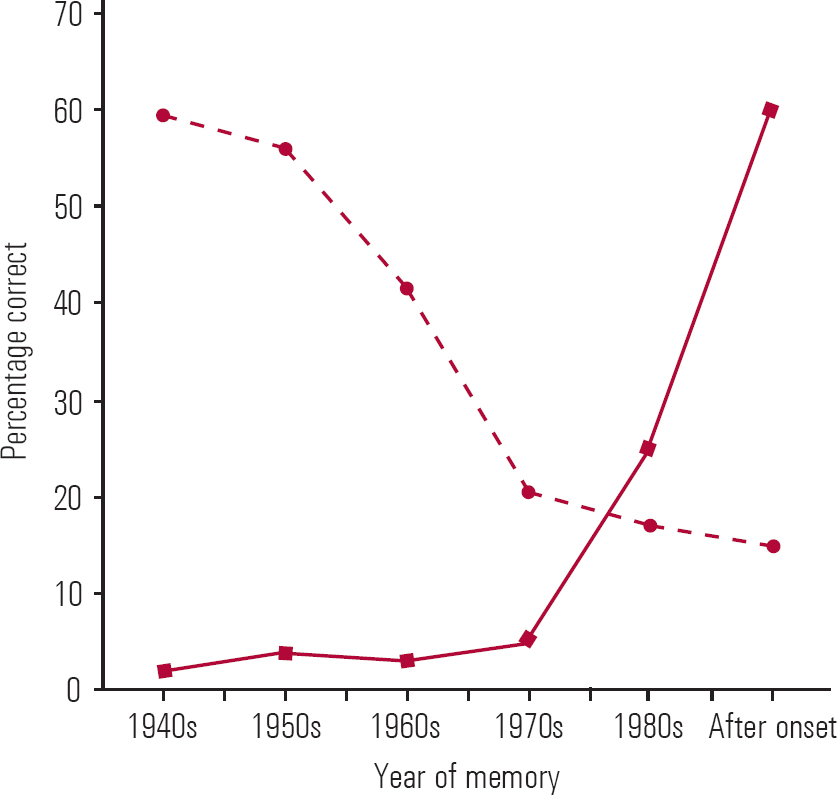
FIG 2 Example of retrograde memory performance plotted against age of memory for a psychogenic amnesia (![]() ) and a neurological amnesia such as transient global amnesia (
) and a neurological amnesia such as transient global amnesia (![]() ). Note the characteristic ‘reversed’ temporal gradient for psychogenic amnesia (see Reference Kritchevsky, Zouzounis and SquireKritchevsky 1997).
). Note the characteristic ‘reversed’ temporal gradient for psychogenic amnesia (see Reference Kritchevsky, Zouzounis and SquireKritchevsky 1997).



eLetters
No eLetters have been published for this article.