India is undergoing rapid nutritional transition(Reference Wasir and Misra1, Reference Misra and Khurana2). Driven by aggressive advertising, low cost and easy availability, people are increasingly consuming high-saturated-fat snacks, refined carbohydrates and sweetened carbonated beverages. There is an increased inclination to replace traditional meals with energy-dense imbalanced foods(Reference Misra and Khurana2). Such dietary patterns with inadequate physical activity trigger the onset of fat deposition(Reference Gupta, Shah and Goel3) and lead to early metabolic derangements such as the metabolic syndrome and type 2 diabetes mellitus(Reference Wasir and Misra1, Reference Misra and Khurana2).
Nutrition and physical activity are major modifiable lifestyle factors related to the development of non-communicable diseases(Reference Woo, Leung and Ho4). Presently, the school system in India does not lay emphasis on health education or the practical application of health-related knowledge. It is often left to physicians to educate children and adults about healthy living. As many healthy (or unhealthy) life-long practices begin in adolescence, it is important to study the nutritional knowledge and behaviour in this age group(Reference Harvey-Berino, Hood and Rourke5). Also, the changes brought about by an educative intervention during these formative years are more likely to track into adulthood as healthy preferences. Moreover, children do not always choose what they eat; very often parents decide and prepare food for them. Clearly, parents, peers and teachers can play a crucial role in shaping each child's outlook towards health.
Previous studies that investigated health and nutrition-related knowledge of Asian Indian children were conducted one to two decades back and included small samples from a single city(Reference Vijayapushpam, Menon and Raghunatha Rao6–Reference Tragler8). Further, they did not assess children's knowledge about factors pertaining to physical activity and non-communicable diseases. Nutritional transition and the effect of westernisation have become apparent in developing countries only during the last 5 years(Reference Wasir and Misra1, Reference Misra and Khurana2). Therefore, it is crucial to evaluate various aspects of knowledge in the present era. Moreover, no previous study to our knowledge has explored the relationship between knowledge and practice about health, nutrition, physical activity and non-communicable diseases in Asian Indian adolescents.
In the present study, we aimed to assess the impact of a controlled educative intervention on health and nutrition-related knowledge and behaviour of urban Asian Indian children. If the effectiveness of this model could be established, it may give directions for future school-based health and nutritional intervention programmes.
Subjects and methods
Study design
The data were collected as part of a school-based intervention programme, the Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing (MARG; Hindi for ‘path’)(9) involving children (aged 8–18 years; n 40 196), parents (n 25 000) and teachers (n 1500) from three cities of North India (New Delhi, Agra and Jaipur) during the period from August 2006 to December 2008.
Sampling design
Initially, a list containing the names of all senior secondary government (or public) and non-government (or private) schools located in each city was prepared. From each city, five government schools and five private schools were randomly selected and enrolled for the study. The government schools were primarily run through financial aid provided by the central or state governments and catered to children of low and low-middle socio-economic status (SES). The private schools were managed by private management and catered mainly to children of upper-middle and high SES. This sampling design ensured proportional representativeness of the sample with respect to all SES. Nutritional education was imparted to all children, parents and teachers of these selected schools. From among the entire study population, cross-sectional sampling was used to collect a representative sample of subjects, to whom the study questionnaire was administered (Fig. 1). The present study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Board. Written informed consent was obtained from subjects aged 18 years or older and from the parents or guardians of subjects younger than age 18 years.
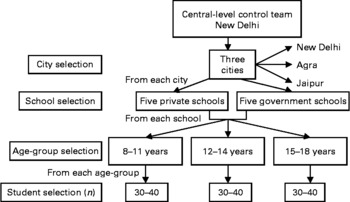
Fig. 1 Key steps in the subject selection process for the questionnaire survey. Parents were selected for the pre-intervention survey during parent–teacher meetings using the same process. Twenty to thirty teachers were randomly selected from each school for the pre-intervention survey.
Knowledge and behaviour assessment questionnaire
A detailed knowledge and behaviour assessment questionnaire was prepared at the National Foundation for Diabetes, Obesity, and Cholesterol Disorders (N-DOC), Diabetes Foundation (India). The questionnaire included the following themes: health, nutrition, diseases (obesity, diabetes, hypertension, CVD and dyslipidaemia), physical activity, and healthy cooking practices. Each theme included fifteen to forty-five questions (total 164 questions) and respondents were required to choose one of the three options, ‘yes’, ‘no’, or ‘I do not know/cannot say’, for each question. A score was given for each question; a correct answer was scored as +1, an incorrect answer as − 1 and ‘I do not know/cannot say’ as 0. The same questionnaire was used for children, parents and teachers. Before the main study, the questionnaire was pre-tested in one of the schools to identify any inadequacies or omissions. Results of this survey were used to modify the questionnaire. A few key questions included:
(1) Is exercise important for staying healthy?
(2) Is obesity ‘excessive fat in the body’?
(3) Are carbohydrates the main energy source in our diet?
(4) Is steaming of food a healthy cooking practice?
(5) Is diabetes ‘increase in blood sugar level’?
Pre-intervention knowledge and behaviour assessment
At baseline, a total of 3128 children, 2241 parents and 841 teachers completed the questionnaire. This information served as the baseline data for the study. The maximum scores in knowledge and behaviour sections for each age group were estimated. Scores of more than 75 % of the maximum were considered ‘good’; 50–75 % were considered ‘fair’ and scores lower than 50 % were considered ‘poor’(Reference Harvey-Berino, Hood and Rourke5).
Educational intervention
A health and nutrition-related educative intervention was carried out in all selected schools over a period of 6 months. Each team conducting the intervention consisted of physicians, well-qualified nutritionists and field workers. The teams in all three cities were trained extensively to ensure collection of reliable and valid data. The study was coordinated at the central level in New Delhi. Education was imparted to the entire study population and not only to the subjects selected for questionnaire surveys.
Separate age-appropriate education modules were developed for school children in the three age groups and for their parents and teachers. Each module included not only didactic lectures, but also several innovative activities. Junior school children (aged 8–11 years) were educated through creative tasks such as making posters, masks, cards and cartoons. Middle (aged 12–14 years) and senior school (15–18 years) children participated through school plays, debates, extempore, posters and cooking competitions. Several other activities such as healthy snack making, paragraph writing, healthy tiffin day, quizzes, health board setups, collage making, healthy recipe writing, and slogan and poem writing were also organised for school children, parents and teachers.
Lectures were conducted using easily comprehensible power-point presentations, which included pictorial graphics, cartoon characters and educative quotations. Each lecture was followed by interactive discussions, wherein the team members addressed all health and nutrition-related queries from the participants. Subsequently, reader-friendly, attractive and informative booklets (see online supplemental material) were distributed as take-home material for reinforcing and sustaining the information gained through lectures and group discussions (Fig. 2). The booklets also included detailed information about the causes and prevention of common non-communicable diseases such as obesity, diabetes, hypertension and CVD.
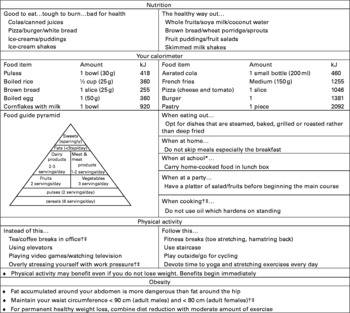
Fig. 2 Key statements from educative posters and booklets used in the study. * Specific for school children. † Specific for parents. ‡ Specific for teachers.
Educative activities and questionnaire surveys were pursued during the non-academic periods in the school curriculum. The research team ensured weekly interaction with school children, each interaction lasting between 45 min and 1 h. Parents were sensitised to healthy living practices during parent–teacher meetings, held at least once in 6 months. About one or two lectures were organised for all teachers of each school. The teachers also participated in student activities and helped in consolidating the messages further. For propagating information within the school environment, each participating school was provided with between one and three sets of seven informative and eye-catching posters that were displayed on the school boards to ensure maximum readership. A total of 125 activities and fifteen health camps were conducted in the three cities. Besides this, 480 students and eighty-nine teachers were trained as volunteers to spearhead the initiative in their respective schools.
Post-intervention knowledge and behaviour assessment
After 6 months of educational intervention in the three cities, students were again randomly selected, as described in Fig. 1. The same questionnaire, used in the baseline survey, was administered to these school children (n 2329) to assess improvement in their knowledge and behaviour scores. The same research team administered the post-intervention survey. School children were not pre-informed about the follow-up survey to avoid any bias. During this programme, the post-intervention survey was usually conducted around January. Due to academic pressure of examinations in January, fewer children consented to participate in the follow-up survey, resulting in a reduced sample size.
Statistical analysis
Data were managed on an Excel spreadsheet. All entries were double-checked for any possible keyboard error. The χ2 test was applied to analyse the variation in frequency of correct responses between children from government and private schools. Knowledge and behaviour assessment scores were computed as arithmetic mean and standard deviation. The questionnaire scores were normally distributed (by skewness/kurtosis tests for normality). Comparison was made between the pre- and post-intervention scores of children using the independent-samples t test. One-way ANOVA and Scheffé's post hoc test was done to compare the differences in scores of children, parents and teachers. Multiple linear regression analysis was applied, with knowledge and behaviour scores as dependent variables and age, sex and type of school as independent variables. P < 0·05 was considered statistically significant. STATA (version 9.0; StataCorp., College Station, TX, USA) was used for data analysis.
Results
Sample characteristics
Of the 3128 children selected for the pre-intervention survey, 47 % (n 1475) belonged to government schools and 52 % (n 1633) were males. In the post-intervention survey, 47 % (n 1101) were from government schools and 54 % (n 1258) were males.
Assessment of baseline knowledge and behaviour scores
The percentage of children in each age group who answered each question correctly at baseline and also after intervention is given in Table 1. In the baseline survey, private school children performed significantly better than those from government schools in most of the themes under study (P < 0·05). The maximum frequency of correct responses was observed in the 15–18 years age group and the least in those aged 8–11 years. Among government school children aged 8–11 years, only 40 % were aware that exercising regularly was important for being healthy. Subsequently, only 18 and 45 % children in this age group in government and private schools, respectively, chose outdoor games over indoor games. Only a small proportion of children in government schools gave correct answers about proteins (14–17 %), carbohydrates (25–27 %) and saturated fats (18–32 %). About half of the school children were not sure about the dietary sources of vitamins and fibre. Only one-third of the children knew correctly about the types of milk available for use. Though a majority of children (74–89 %) aged 12–18 years had an accurate idea about the pathogenesis of diabetes, the correct knowledge about CVD was limited to 21–43 % students in government schools and 32–54 % in private schools across all age groups.
Table 1 Proportion of children (%) who answered key knowledge and behaviour assessment questions correctly, before and after the ‘Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ (MARG) intervention
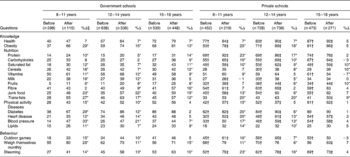
* Significantly different before and after MARG intervention (P < 0·05).
† Significantly different compared with government school, before intervention (P < 0·05).
‡ Significantly different compared with government school, after intervention (P < 0·05).
§ Percentage improvement.
In government schools, males had significantly higher baseline knowledge and behaviour scores than females (P < 0·05) (Table 2). No such difference was observed in private schools. The mean scores increased significantly with age in both types of schools (P < 0·05). On multiple linear regression in children, increasing age, being male and studying in private schools independently predicted higher baseline knowledge and behaviour scores (P < 0·001) (Table 3). Knowledge scores correlated significantly with behaviour scores in all children (r 0·687; P < 0·001; data not shown). Knowledge and behaviour scores increased linearly with age in children (trend analysis; P < 0·001).
Table 2 Knowledge and behaviour assessment scores before and after the ‘Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ (MARG) intervention in children
(Mean values and standard deviations)
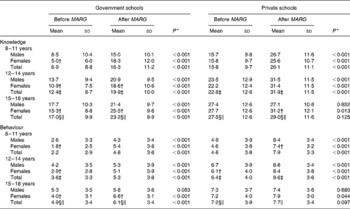
* Significantly different before and after MARG intervention (P < 0·05).
† Significantly different compared with males of this category (P < 0·05).
Scheffé's post hoc ANOVA was used to compare the total mean scores among the three age groups: ‡ 8–11 years v. 12–14 years, § 8–11 years v. 15–18 years, ∥ 12–14 years v. 15–18 years.
Table 3 Multiple linear regression for knowledge and behaviour scores in school children aged 8–18 years‡
(β Coefficients and 95 % confidence intervals)
MARG, The Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing.
* P < 0·001 (considered significant).
† P = 0·003.
‡ All models adjusted for age, sex and school type.
§ Reference: female.
∥ Reference: government schools.
Impact of MARG educational intervention
Following the intervention, knowledge and behaviour scores improved significantly in all children, irrespective of the type of school (P < 0·05), except in 15- to 18-year-old adolescents of private schools (Table 2). A significantly higher improvement was observed in 8- to 11-year-olds as compared with older children (12–18 years) (P < 0·05); and in government schools as compared with private schools (P < 0·05) (Fig. 3). Significantly higher scores were observed in private school children as compared with government school children, even after educational intervention (Table 1). Among 8- to 11-year-olds, more than 15 % improvement was noted in knowledge regarding obesity, trans-fatty acids, physical activity, diabetes and blood pressure. Following the intervention, more than 10 % additional students considered steaming of food a healthy cooking practice and preferred outdoor games over indoor games.
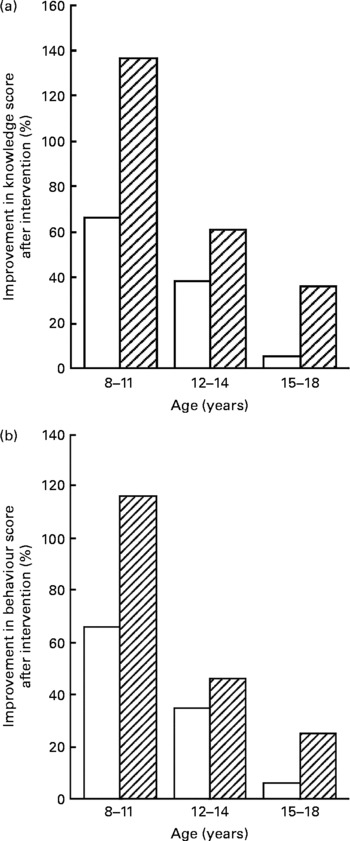
Fig. 3 Percentage improvement in knowledge (a) and behaviour (b) assessment scores of children from private schools (□) and government schools (![]() ) after the ‘Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ (MARG) intervention. A significantly higher improvement in both knowledge and behaviour scores was observed in 8- to 11-year-olds as compared with older children (12- to 18-year-olds) (P < 0·05), and in government schools as compared with private schools (P < 0·05).
) after the ‘Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ (MARG) intervention. A significantly higher improvement in both knowledge and behaviour scores was observed in 8- to 11-year-olds as compared with older children (12- to 18-year-olds) (P < 0·05), and in government schools as compared with private schools (P < 0·05).
After MARG intervention, there was no significant sex-based difference in knowledge and behaviour scores, thus indicating that the intervention caused much higher improvement in females as compared with males (Table 3).
Comparison of baseline scores in children, parents and teachers
With respect to knowledge and behaviour, private school parents and teachers scored better than their government school counterparts (P < 0·05) (Fig. 4). On comparing the scores among children, parents and teachers (using Scheffé's post hoc test), the following order was observed in scores in both types of school: teachers>parents>children aged 15–18 years>children aged 12–14 years>children aged 8–11 years (P < 0·05 for all).
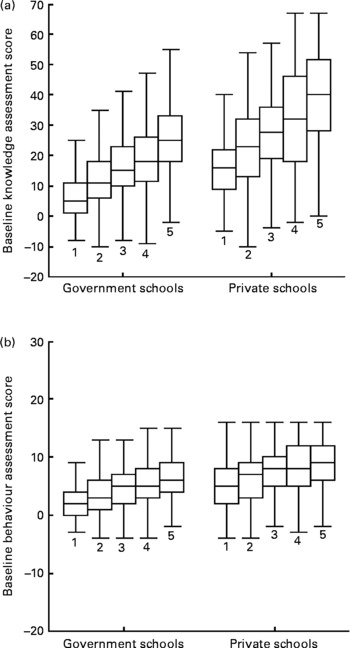
Fig. 4 Comparison of baseline knowledge (a) and behaviour (b) assessment scores in children, parents and teachers. 1, Children aged 8–11 years; 2, children aged 12–14 years; 3, children aged 15–18 years; 4, parents; 5, teachers. Mean values are indicated by the horizontal lines, 95 % confidence intervals by the boxes and ranges by the whiskers. Private school parents and teachers scored significantly better than their government school counterparts (P < 0·05), with respect to both knowledge and behaviour. On comparing the scores among children, parents and teachers (using Scheffe's post hoc test), the following order was observed in scores in both types of school: teachers>parents>children aged 15–18 years>children aged 12–14 years>children aged 8–11 years (P < 0·05).
Grading and accordance of baseline knowledge and behaviour scores
Knowledge and behaviour scores of children, parents and teachers were graded as poor, fair and good, as elaborated in the methodology section. In government school children aged 8–11 years, the knowledge and behaviour scores were rated as poor in 94 and 91 %, respectively (Table 4). In these schools, though a smaller percentage of parents (16 %) and teachers (24 %) had ‘fair’ knowledge, a higher percentage had ‘fair’ behaviour (parents 22 %; teachers 31 %). Among private school children aged 15–18 years, though knowledge score was good in 14 %, only 7 % practised healthy behaviour. A higher percentage of private school teachers had fair knowledge (35 % teachers v. 31 % parents) and behaviour (47 % teachers v. 37 % parents) as compared with the parents.
Table 4 Frequency (%) of baseline knowledge and behaviour scores among children, parents and teachers*
* Scores: good, score>75 % of maximum; fair, score 50–75 % of maximum; poor, score < 50 % of maximum.
Discussion
The present study highlights marked gaps in health and nutrition-related knowledge and behaviour of urban Asian Indian school children, specifically those aged 8–11 years. Significantly higher knowledge and behaviour scores were noted among private school students as compared with government school students. Encouraging results were observed in the post-intervention survey, with a significant improvement in scores of all children.
During adolescence, several developmental and social changes take place, which influence lifestyle and eating patterns. School children have considerable purchasing power(Reference Singh10) and, often, several food options to choose from. However, they do not have the natural ability to choose a nutritious diet. Therefore, it is essential to educate them about health and nutrition during their school days. As reported previously(Reference Nelson, Lytle and Pasch11), the present study showed low knowledge about health and nutrition in children, before educative intervention. Children were not aware of key topics such as energy, proteins, carbohydrates and saturated fats. Approximately 75 % government school children did not consider carbohydrates as the main energy source in the diet. They did not understand the concept of nutritive value and that a combination of cereals and pulses would increase the nutritive value of food. Such lack of knowledge about dietary components may explain the high intake of dietary fats(Reference Gupta, Shah and Goel3) and subsequently high prevalence of obesity(Reference Bhardwaj, Misra and Khurana12) in urban Asian Indian school children and adolescents.
Quite often, children and their parents are not aware of genuine information sources and risk their chances of making unhealthy choices(Reference Jones, Andrews and Tapsell13). Many pre-packaged foods that are marketed as ‘low-cost’ are poor in nutrition and frequently bear misleading labels about their nutritional value. A majority of children in the present study (54–72 %) were not aware that trans-fatty acids are hidden in many processed and packaged foods including chips (crisps) and French fries(Reference Ratnayake, Hollywood and O'Grady14). They are present even in commonly consumed Indian snacks such as samosa (triangular pastry shell with a filling of potatoes), kachori (refined wheat flour bread stuffed with spiced vegetables), pakore (slices of vegetables dipped in a batter of gram flour) and chole bhature (a combination of chick peas and breads made of refined wheat flour), as most of these snacks are deep fried in repeatedly heated hydrogenated oil(Reference Misra, Khurana and Isharwal15). However, only 25–55 % school children in the present study considered these snacks to be junk food. Further, many false nutritional beliefs in Asian Indian societies are transmitted through the generations. Several respondents (20–25 %) in the present study believed that the excess water in which vegetables have been cooked should be discarded and that consuming butter is associated with strong bones and good health (25–35 %). Previous studies have also suggested that a child's nutritional knowledge comes more often from home than from the school(Reference Arcan, Neumark-Sztainer and Hannan16). This emphasises the need to impart health education not only to children, but also to the community as a whole.
Schools have been identified as an important setting for health promotion activities(Reference Crockett, Petersen, Millstein, Nightingale and Petersen17, Reference Parcell, Keider, Basen-Engquist, Poland, Green and Rootman18). The introduction of the health and nutrition curriculum in schools has resulted in a significant improvement in knowledge, attitudes and behaviours of students(Reference Vijayapushpam, Menon and Raghunatha Rao6, Reference Tragler8, Reference Baranowski, Davis and Resnicow19, Reference Foster, Sherman and Borradaile20). In India, a dual system exists, in which the lower- and lower-middle-SES families send their children to government schools, while the upper-middle- and higher-SES families send their children to private schools. Established ideas of social status and hierarchy tend to influence this decision. According to the Annual Status of Education Report (ASER) 2008, the private school sector educates only 22·5 % students in India(21). Private schools are often less bureaucratic, have better amenities and offer an English medium curriculum. Since most of the health and nutrition information available through books, newspapers and the Internet is written in English, private school children may tend to learn these things on a more subconscious level(Reference Boehl22). Also, they get better access to several forms of informative mass media, due to an apparent economic edge. Prior research has documented an association between children's cognitive abilities and the SES of their parents as measured by education level, occupation and income(Reference Sigelman, Derenowski and Mullaney23, Reference Phillips, Hayden and Norris24). High-SES parents are better educated, have better occupational profiles and are more likely to transmit educational advantage to their children through cultural and economical means(Reference Sullivan25). Thus, the results from the present study, indicating higher scores among private school children and parents, were comparable with realistic situations.
School teachers can be a crucial link in providing health education, addressing misconceptions and improving understanding about a healthy lifestyle. In the present study, when an educative environment was provided to school children by our team members, they registered significant improvement in their knowledge and behaviour scores, indicating the effectiveness of teaching. Though the gains in scores of government school children were higher than those of private school children, the gap still remained. Further, our educative sessions facilitated frequent and individual interactions with students, which may not be a routine in most schools. The knowledge and behaviour scores of private school children aged 15–18 years did not change significantly, as they already had high scores during the baseline survey. This may also be explained by the assumption that older children are less receptive to newer information as compared with younger ones and, hence, educational initiatives should begin early during childhood. The large increase in correct responses to specific themes such as physical activity and healthy cooking practices may be explained by the students' higher interest in information that they may use in everyday life.
The present study revealed a sizeable gap between knowledge and behaviour of Asian Indians, as has been reported in other countries(Reference Girois, Kumanyika and Morabia26–Reference Mirmiran, Azadbakht and Azizi28). Though a considerable proportion of private school subjects had good knowledge of health and nutrition, only a few practised healthy behaviour. It is also pertinent to note that the prevalence of obesity in private schools has been noted to be much higher than in government schools in India(Reference Bhardwaj, Misra and Khurana12) despite their ranking better in knowledge. Clearly, the availability of high-energy junk foods and physical activity schedules are important factors in determining obesity in contrast to knowledge alone.
Limitations
The present study dealt with qualitative aspects of the dietary intake pattern of Asian Indian school children. It did not provide quantitative data on diet and nutrition, which have been described in our previous study(Reference Gupta, Shah and Goel3). Considering that analysis of the results of a knowledge, attitude and practice (KAP) questionnaire may be beneficial in health promotion programmes, there is no standard questionnaire on nutritional KAP for Asian Indian school children. Post-intervention assessment could not be carried out in parents and teachers.
Conclusion
The present study, the largest conducted in South Asia, indicates a significant impact of educative intervention on knowledge and behaviour of urban Asian Indian school children with regards to health, nutrition and non-communicable diseases. Clearly, it is important to start early and sustain health education efforts throughout a child's school experience. These efforts should appropriately include participation by parents as well as teachers in preschool, elementary, and secondary schools. Eventually, it is essential to create a festive atmosphere, emphasising that achieving and managing a healthy lifestyle can be fun. The information gathered here might help in the future design of a realistic primary prevention programme for diabetes and CVD in India, and other developing countries.
Acknowledgements
The study was supported by the World Diabetes Foundation, Denmark (WDF05-120)(9).
We acknowledge the cooperation of students and their parents; teachers and principals of the schools which participated in school surveys and the MARG programme. We thank Ms Meeta Lall and Dr Amit Noheria for their helpful comments and reviewing the manuscript.
The authors' contributions were as follows: P. Shah, A. M. and N. G. were responsible for the concept and design of the study; P. Shah, A. M., D. K. H., R. G., P. Seth, P. K. G., A. K., S. Bansal, A. K. G., A. A., A. J., N. H., P. K., P. T., I. M., R. B., S. G. and S. Bharadwaj were responsible for data collection; P. Shah, A. M., R. M. P. and R. S. were responsible for monitoring the study; P. Shah, A. M., N. G., K. G. and R. M. P. were responsible for data interpretation and analysis; P. Shah, A. M., N. G., K. G., D. K. H., R. G. and R. M. P. were responsible for manuscript writing. P. Shah, A. M. and N. G. contributed equally to the study.
No conflicts of interests were declared.
The supplemental material is available online only at http://journals.cambridge.org/action/displayJournal?jid = bjn










