Introduction
Up to 80% of all Emergency Department (ED) visits involve pain as a component of the presenting complaint.Reference Cordell, Keene and Giles 1 - Reference Tanabe and Buschmann 3 Numerous studies indicate that inadequate pain management during medical care can have many detrimental short and long-term effects,Reference Megel, Houser and Gleaves 4 - Reference Weisman, Bernstein and Schechter 7 and the World Health Organization has advocated for optimal pain treatment for all.Reference MacLean, Obispo and Young 8
Children’s pain in the ED remains poorly managed despite an increase in pain research over the past decade.Reference Belleville and Seupaul 9 - Reference Todd, Ducharme and Choiniere 12 A recent multicenter study found only 60% of patients in pain receive any analgesia in the ED.Reference Todd, Ducharme and Choiniere 12 Time to initial analgesia across a number of studies varies from 74-116 minutes, suggesting that there is significant room for improvement.Reference Todd, Ducharme and Choiniere 12 - Reference Petrack, Christopher and Kriwinsky 15
A limited number of American studies have assessed resident knowledge and pain management practices in non-ED settings. Anesthesia residents have been found to have a significantly better knowledge base regarding pediatric pain management when compared to pediatric or orthopedic residents.Reference Saroyan, Schechter and Tresgallo 16 The only study evaluating emergency medicine (EM) residents compared them to pediatric residents, and found that 99% of EM residents provided analgesia prior to performing a lumbar puncture, compared to 43% of pediatric residents. While this suggests EM residents may be better at pain management for this procedure, the overall adequacy of analgesia for presenting complaints involving pain was not assessed.Reference Breakey, Pirie and Goldman 17
A survey of various medical schools across Canada found that some two-thirds of programs could not identify any specified curriculum time for pain education. In contrast, a study published in 2009 found that 100% of veterinary faculties had a pain education curriculum.Reference Watt-Watson, McGillion and Hunter 18 Researchers have long recognized that lack of pain management education is associated with a lack of knowledge in practicing health care professionals.Reference Maclaren and Cohen 19 Understanding the EM residents’ perspective of pediatric pain management has the potential to help tailor education programs for these learners. The objectives of this study were to describe the following amongst EM residents: (a) the extent and type of training received in pediatric pain management; (b) the approach to common painful pediatric presentations; (c) the level of comfort in assessing and treating pediatric pain; (d) the perceived facilitators and barriers to optimally managing pediatric pain; and (e) the attitudes towards education and management of pediatric pain in the ED.
Materials and Methods
Study design and participants
A descriptive, cross-sectional survey of emergency medicine residents at three Canadian universities was undertaken during the 2012-2013 academic year: McGill University, The University of Alberta, and The University of Calgary. The study population was comprised of Royal College of Physicians and Surgeons of Canada Emergency Medicine residents (FRCP-EM) and clinical fellows (CF), College of Family Physicians of Canada Emergency Medicine residents (CCFP-EM) and CFs, and Pediatric Emergency Medicine (PEM) residents and CFs.
Survey tool
A survey instrument was created after literature review and with the guidance of an expert panel, in keeping with previously established methods.Reference Burns, Duffett and Kho 20 The five main themes of the instrument were: (a) demographic characteristics; (b) knowledge and education regarding pain assessment and treatment; (c) perceptions of pediatric pain management; (d) current practices; and (e) perceived barriers and facilitators. Questions were multiple choice or short-answer; open-ended questions were thematically coded by two of the team members (HA, SA). The expert panel consisted of experts in medical education, pediatric pain management, and emergency medicine (both faculty and trainees). The survey required less than 15 minutes for completion.
Survey distribution methodology
The electronic implementation of the survey was coordinated by the Clinical Research Informatics Core (CRIC, University of Alberta). Checkbox.com was used to create and distribute the survey. Consent to participation in the study was implicit in completion of the survey. An advance email notification was sent, followed by an information letter and the survey link 7 days later. Non-responders were sent a reminder email 21 days after the initial notification and the study was closed to further responses at 42 days after the initial notification.
Data Analysis
Standard descriptive statistics (means, medians, standard deviations, and ranges) were generated for continuous variables, and frequency distributions were generated as categorical variables. The 95% confidence intervals were calculated as appropriate. In all assessments of level of comfort, the variable in question was collapsed to a dichotomous (comfortable/uncomfortable) response. Comparisons between groups (e.g., junior versus senior residents) were assessed using Fisher’s exact test. Comparisons among three or more groups were assessed using either the Fisher-Freeman-Halton test for categorical groups (e.g., training program) or the Cochrane-Armitage trend test for ordinal groups (e.g., level of pediatric experience). McNemar’s test was used to assess differences in physicians’ level of comfort treating one year olds and nine year olds. A p-value less than 0.05 was considered statistically significant.
Results
Demographic characteristics
Of 122 residents surveyed (80 FRCP-EM, 26 CCFP-EM, and 16 PEM) 56 were enrolled (46%). The mean age of the participants was 29.5 years and they had a median of 12 weeks of experience in a pediatric ED (range 3-104 weeks). Demographic information on study participants is provided in Table 1. Seventy-one percent (40/56) of participants did not have children, and 15% (8/54) had personally used prescription pain medications within the last six months.
Table 1 Demographic characteristics of participants (n=56)

PGY=post-graduate year
Pediatric pain assessment
Forty-five percent (25/55) of participants reported that they did not receive any training in pediatric pain assessment. Of the 33% (18/55) who did, 33% (6/18) received both formal and informal training, and 28% (5/18) received only informal training. Twenty-two percent of participants (12/55) reported they were unsure if they had received any training on pediatric pain management. Sixty-one percent (11/18) of educational sessions reported on pediatric pain assessment were taught by emergency physicians, 17% (3/18) by residents, and 17% (3/18) by other physicians (including anesthesiologists and intensivists).
The most common assessment tools that residents reported they had been taught about were the Faces Pain Scale (FPS) (29%, 16/56), the Visual Analog Scale (VAS) (25%, 14/56), the Numerical Rating Scale (NRS) (14%, 8/56), and the Face, Legs, Activity, Cry, Consolability scale (FLACC) (7%, 4/56). In contrast, 13% (7/56) reported that they used the VAS, 7% (4/56) the FPS, 7% (4/56) the NRS, 5% (3/56) the FLACC. Eleven percent (6/56) stated that they did not use any tool to assess pediatric pain. (See Figure 1, which summarizes the findings regarding participants’ reported level of comfort assessing pediatric pain.)
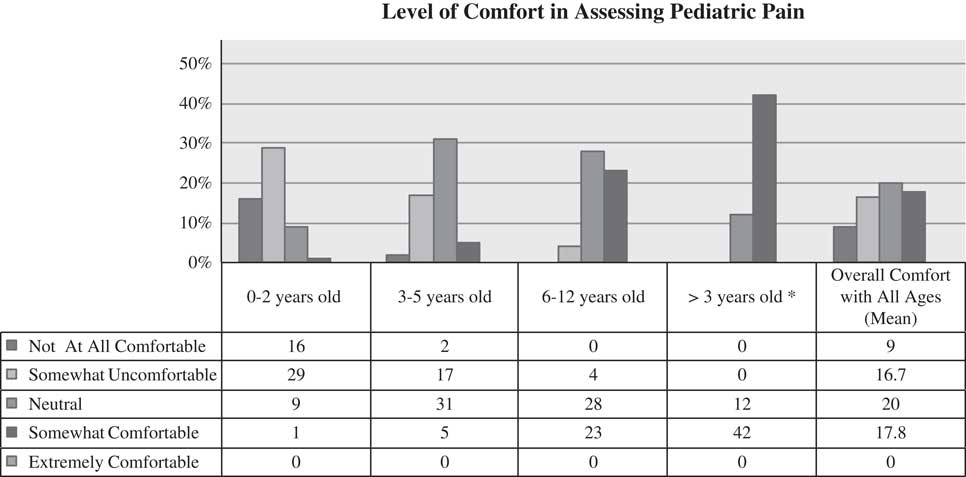
Figure 1 Participant level of comfort in assessing pediatric pain (n=55)
All years of residents reported that they were uncomfortable with the assessment of pain in 0-2 year olds (p=0.07); for patients aged 2-12 years; level of comfort with pain assessment increased with years of training (p=0.02). Table 2 provides information on participant level of comfort with assessment of children’s pain, categorized by weeks of pediatric ED experience. There was no statistically significant difference in level of comfort in assessing pediatric pain for any age group across different training programs.
Table 2 Participant level of comfort with assessment of children’s pain, categorized by weeks of pediatric ED experienceFootnote *
* Results represent the number of respondents that were “comfortable” or “very comfortable.”
Eighty-three percent (45/54) of respondents reported they were “extremely” or “somewhat” uncomfortable with the assessment of pain in a disabled, non-verbal child; 85% (47/55) had not received any training on how to assess pain in this population. Eleven percent (6/55) of respondents were unsure if they had had any training on this subject.
Treatment of pediatric pain
Sixty-nine percent (38/55) of respondents reported having received post-graduate training on how to treat pediatric pain, 18% (10/55) did not recall receiving any such training and 13% (7/55) reported they were unsure. Thirty-five percent of respondents (13/37) indicated that their training was formal, 27% (10/37) informal, and 38% (14/37) reported that they received both. The teachers providing this training were emergency physicians (89%, 33/37), residents (38%, 14/37), other physicians (14%, 5/37), and nurses (3%, 1/37).
Fifty-eight percent (32/55) of respondents reported having received teaching on non-pharmacologic interventions for the management of pediatric pain, 13% (7/55) had not and 29% (16/55) were unsure. Most respondents reported using various distraction techniques (n=42); some reported using glucose/sucrose (n=18), the help of parents or caregivers (n=16), and child life specialists (n=7).
Figure 2 illustrates participants’ reported comfort level with the use of various pain medications for a one and nine year old child. When treating pain for a nine year old, there was no statistical difference in level of comfort of junior residents (year 1-2) compared to senior residents (year 3-6) regarding the use of oral oxycodone (p=0.70), oral morphine (p=0.27), IV morphine (p=0.12), oral codeine (p=0.57), intranasal fentanyl (p=1.00), distraction techniques (p=0.72), or regional nerve blocks (p=0.18). All residents reported they were more comfortable using opioid pain medications for a nine year old, as compared to a one year old (oral oxycodone p<0.001, oral morphine p<0.001, IV morphine p=0.004). Table 3 describes the top two medications of choice for mild (2/10), moderate (5/10) and severe (7/10) pain scenarios.
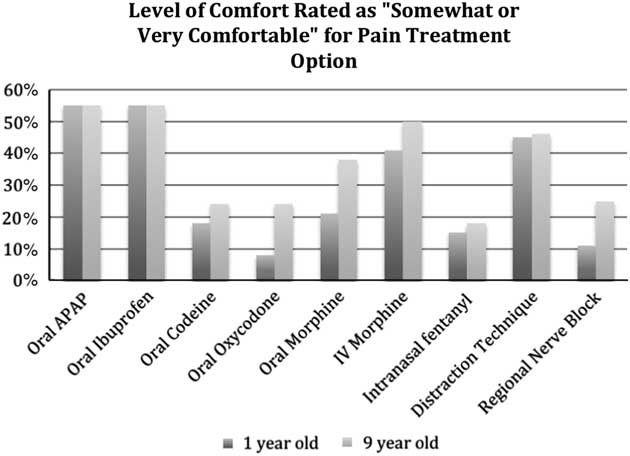
Figure 2 Participant level of comfort for pain treatment option (n=55)
Table 3 Top medication choices for pain relief for a 7-year-old child, based on severity of pain (n=55)

IV=intravenous, PO=per os, SC=subcutaneous, NSAID=non-steroidal anti-inflammatory
* n=54
Participants reported that they would wait a median of 30 minutes (range 15-120 minutes) after the administration of one dose of oral ibuprofen before reassessing the patient’s level of pain. After the administration of one dose of intravenous fentanyl, residents reported that they would wait a median of 5 minutes (range of 1-60 minutes).
When asked how analgesic medications affected parent/caregiver satisfaction, 49/54 (83%) of participants felt that it significantly improved satisfaction, 8/54 (15%) felt it somewhat improved satisfaction, and 1/54 (2%) felt it somewhat worsened satisfaction. When participants were asked how important it was for patients to be pain free when discharged from the ED, the mean level of importance on a scale of 0 to 100 was 76; when asked how important it was for patients’ pain scores to be less than 3/10 when discharged from the ED, the mean level of importance was 88.
Barriers to managing children’s pain
Table 4 outlines the barriers reported by participants to assessing pain in a pediatric patient. The most commonly cited barrier was self-reported lack of comfort in the participant’s ability to assess degree of pain (especially in young infants or those with developmental disabilities).
Table 4 Barriers reported by participants to assessing and treating pediatric pain (n=55)
Multiple responses were permitted.
Pediatric pain management teaching
When participants were asked how important they felt it was to receive education about pediatric pain management, 98% (54/55) felt it was “extremely important” or “somewhat important.” The methods reported as best to teach pediatric pain management included role modeling (61%, 34/56), lecture format (57%, 32/56), simulation (32%, 18/56), or web-based learning (29%, 16/56).
Discussion
To our knowledge, this study is the first to survey the knowledge and attitudes of EM residents caring for children with pain. Our findings indicate that EM residents have limited overall exposure to children and minimal formal training in pediatric pain management. Specific deficiencies we identified include the care of very young children and children with developmental disabilities. Residents do, however, report a desire to be proficient in the care of children in pain.
Residents participating in our study reported limited training in the assessment of pediatric pain, with a large percentage of unable to recall receiving any training. The first step to appropriate pain management is the assessment of pain, and our findings suggest residents receive insufficient training in this skill. Pain assessment tools are well studied, and several have been validated for use in children as young as 3 years of age; however, a gold standard amongst these has yet to be identified.Reference Tomlinson, von Baeyer and Stinson 21 The large array of tools available, and the lack of consensus regarding the best choice, may contribute to their inconsistent and infrequent use. The authors of a recent systematic review suggested that a single pain assessment tool be used within an institution, as the change in score is a more important variable than the absolute number.Reference Tomlinson, von Baeyer and Stinson 21
Residents participating in our study reported feeling very uncomfortable when attempting to assess pain in the age group of 0-2 years. This trend was reversed once the child was 13 years or older, likely because the assessment of this group is very similar to that in adults. There has been limited research on pain assessment in very young children; however, preliminary studies suggest that the FLACC observational tool can be successfully used in children aged 6-42 months, and accurately identifies pain and distress.Reference Babl, Crellin and Cheng 22 Resident educational interventions should be specifically directed at the assessment of pain in this patient population.
One of the most striking and novel findings in our study was that residents reported lack of comfort in the assessment of pain in a child with a developmental disability, specifically one that rendered them non-verbal. The majority of residents reported feeling uncomfortable in such a scenario, and indicated they had not received any training on how to assess pain in such patients. Previous research has suggested that children with cognitive impairment experience pain frequently, and those with the fewest abilities experience the most pain.Reference Clancy, McGrath and Oddson 23 , Reference Breau, Camfield and McGrath 24 To address this, the Pediatric Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (Ped-IMMPACT) group has called for “specific planning and co-ordination” for communicating with non-verbal and/or cognitively impaired children. 25 , Reference Malviya, Voepel-Lewis and Burke 26 The revised FLACC observational tool has been studied and found to be reliable and valid in children with cognitive impairment in some settings, and while challenging to apply in the ED, may provide a starting point for development of a tool in this environment. This underscores the importance of directing educational initiatives for residents on the assessment of pain in non-verbal, developmentally disabled children.
We found a marked difference in the reported level of comfort for pharmacological treatment of the pain of a non-verbal one-year-old infant compared to a verbal child of nine years of age. This unease with pharmacologic agents in very young children likely contributes to the under-treatment of pain that has been previously reported in this population.Reference Alexander and Manno 27 Several explanations have been suggested for this, including physician lack of comfort with medication dosing, the belief that children don’t feel pain like adults and/or will not remember it, fear of adverse effects, inability of young children to verbalize their needs, potential for opioid dependency, risk of over-sedation, and lack of clear guidelines.Reference Alexander and Manno 27 , Reference Lewis, Lasater and Brooks 28 Residents should be comfortable using a variety of opioid medications across the spectrum of pediatric age groups; this would encourage use of stronger pain medications when clinically indicated and reduce the risk of under-treating pain in non-verbal children.
Residents appropriately choose potent opioids for severe pain, a combination of moderate-potency opioids and NSAIDs for moderate pain, and either acetaminophen or NSAIDs for mild pain. Current best evidence suggests ibuprofen and acetaminophen are the appropriate first-line oral analgesic agents for mild to moderate acute pain in children, and that an opioid such as morphine should be used for persisting pain, or pain of severe intensity. 29 - Reference Morris, Stulberg and Stevermer 31 Our results suggest that this evidence-based approach is followed by EM residents.
Although many residents participating in our study reported using and being taught about non-pharmacologic techniques to reduce pain, there were also many who were not taught this or did not recall being taught. Evidence exists for the efficacy of several non-pharmacologic modalities in the reduction of pediatric pain in the ED, including psychological therapies, complementary and alternative medicine, massage, and music.Reference Ali, Drendel and Kircher 30 , Reference Eccleston, Palermo and Williams 32 - Reference Hernandez-Reif, Field and Largie 34 Lack of resident use of these effective, non-pharmacologic techniques could be rectified through educational initiatives.
Residents assigned a high importance to patients being completely pain-free upon discharge; however, they assigned an even higher importance to pain being classified as at least mild (<3/10) prior to discharge. This is in agreement with the WHO recommendations that pain be at least mild prior to discharge from the ED. 29 This is also important for caregiver satisfaction with their health care experience, as parents of children who experience frequent pain at home report higher dissatisfaction with their child’s care.Reference Gill, Drendel and Weisman 35
Our results suggest that residents appear to recognize that pediatric pain management is an essential part of residency curriculum, and want it to be taught in various formats. Multiple approaches to teaching pain management have been previously reported for non-EM programs. These include online interactive modules, seminars and didactic teaching over a course of days or weeks, small group teaching, interactive conference series, inter-professional discussions, and use of standardized patients; application of these techniques has yielded mixed results.Reference Gehlhar, Tauschel and Lux 36 - Reference Puljak and Sapunar 39 One undergraduate medical education program in the US found that the integration of elements to strengthen emotional skills is an effective educational approach when teaching students about pain.Reference Murinson, Nenortas and Mayer 37 The investigators in this study reported that learners who used personal, reflective portfolios to build awareness of the affective dimensions of pain demonstrated attainment of foundation knowledge, robust engagement in tasks addressing emotional development, and high levels of learner satisfaction. One internal medicine program in the US used a combination of interactive sessions, didactic teaching, provision of pocket reference cards, and emailing of clinical vignettes in their training program.Reference Scott, Borate and Heitner 38 The investigators in this study administered pre- and post-intervention surveys and found that while knowledge and overall documentation of pain did not improve, use of pain scales and “opioid-phobia” did. It is interesting to note that the EM residents in our study ranked traditional teaching formats (specifically role-modeling and lectures) as preferable to simulation, suggesting that pain assessment and treatment may be better taught using more traditional teaching techniques.
Limitations
Our study gathered data through the use of a novel survey instrument, which has not been previously validated. We included three sites in our study, which may limit the generalizability of our results; however, the self-identified deficiencies were common regardless of EM training program, thus suggesting that they are likely generalizable to other Canadian programs. Our response rate and sample size was smaller than desired, despite an effort to have the study championed by local site leads. A higher response rate and resulting greater sample size may have led to more robust and reliable results, and additional statistical power for the training-program-based sub-group analyses. As with all surveys, recall bias may have taken place. Despite these limitations, we feel that this study provides important insights into an area of medical education that, to date, has been largely ignored.
Conclusion
Under-treatment of children’s pain is a ubiquitous problem in the ED. Our study identified three main areas of reported discomfort for EM residents: pediatric pain assessment, management of pain in very young children, and pain management in children with developmental disabilities. We hope that our results will facilitate medical educators at the three involved sites, as well elsewhere in Canada, in gaining further understanding into existing knowledge needs, as well as barriers and facilitators that will affect the implementation of effective EM resident education on acute pain management for children. However, given our small sample size, further inquiry may be prudent to confirm that similar findings exist in other settings. Post-graduate EM curricula should be adjusted to reflect the self-reported weaknesses in the area of children’s pain management that we identified.
Acknowledgements
We would like to thank the attending physicians and residents who pilot tested our study tool, and Mr. Ben Vandermeer of the Alberta Research Centre for Health Evidence program who provided statistical support for this study. We also thank Ms. Pam Marples and the Clinical Research Informatics Core team for their invaluable help with survey dissemination, and Ms. Melissa Gutland for her administrative support.
Competing interests: Dr. Huma Ali secured a McGill University Emergency Medicine Resident Research Grant to support this study. The authors have no financial or other conflicts of interest to disclose.








