Hospital-based neurorehabilitation outpatient programs (HB-NROPs) are ambulatory programs serving individuals with neurologic conditions within a hospital setting. These programs reduce disability and enhance participatory outcomes in persons with common neurological diseases Reference Khan, Amatya, Galea, Gonzenbach and Kesselring1,Reference Rice, Janzen, McIntyre, Vermeer, Britt and Teasell2 ; approximately 13 individuals need to be treated to prevent avoidable deterioration in function in 1 individual. 3 These individuals often face complex problems best addressed by an interdisciplinary team approach characterized by the collaboration of different disciplines of the rehabilitation team. Reference Wade4 Although a coordinated rehabilitation team approach is recommended and leads to better outcomes, Reference Wade4,5 it is generally known that British Columbia (BC) HB-NROPs rarely maximize interdisciplinary practices and often do not include physicians. Therefore, the purpose of this survey was to evaluate access to BC HB-NROPs, explore how HB-NROPs implement interdisciplinary care, and highlight metrics currently being used to monitor the effectiveness of services.
This survey was conducted as a quality improvement project and did not fall within the scope of a Research Ethics Board review, and thus a waiver for ethics was obtained. The survey consisted of 17 questions focused on access to HB-NROPs, interdisciplinary care, and HB-NROP performance measures (Supplemental Material 1).
Participants were recruited via convenience sampling. Open-ended interviews were conducted with healthcare providers from various geographical regions of BC. Interviews were conducted through video or phone meetings and typically lasted 30–45 minutes each. All responses were recorded. Answers to the questions were then analyzed for recurring themes.
Fifteen of 16 providers agreed to participate by invitation by principal investigator PW. They were selected based on regions in BC that have specialists in Physical Medicine and Rehabilitation (PMR also known as physiatrists) in practice in neurorehabilitation. The distribution of providers surveyed included seven individuals from Greater Vancouver, four from BC Interior, and four from Vancouver Island. Twelve individuals were practicing physiatrists, one was a physiotherapist, one was an orthotist, and one was a rehabilitation program coordinator. Collectively, they represented nine HB-NROPs and one community physician spasticity clinic which offers spasticity and complex neurorehabilitation management in a nonhospital outpatient setting. This was included because of a lack of service provision such that there are no hospital-based outpatient clinics offering this type of care in the health region.
All participants reported admission criteria to BC HB-NROPs include functional and realistic goals and the need for at least one allied health discipline (physiotherapy, occupational therapy, and speech-language therapy). One Vancouver Island HB-NROP excluded individuals with peripheral neurological conditions and two HB-NROPs, one in Vancouver Island and one in Greater Vancouver, excluded referrals for clients from third-payer insurance companies such as automobile insurance and workers’ compensation. Third-payer insurance company referrals were excluded to ensure access for those who lack extended benefits, have lower income, or sustain the same injury by a different mechanism or place.
Wait times ranged between 1 or 2 weeks up to 3 months for the initiation of services depending on HB-NROP priority intervention criteria which prioritizes individuals’ need to access services based on acuity, goals, and risk of complications and functional decline. Individuals with acute conditions were seen sooner than individuals with chronic neurological conditions because individuals with chronic disabilities were not at imminent risk of further decline, hospitalization, or developing complications. Three respondents reported that three HB-NROPs were working on reducing the waitlist by re-evaluating their priority intervention criteria and triaging system.
Referral to a HB-NROP is separate from a referral to a physiatrist except for one HB-NROP in Greater Vancouver where a referral to the HB-NROP involved physiatry. To address this issue, one participant on Vancouver Island is working with program administrators to develop a single referral to both HB-NROP and physiatry to improve access to rehabilitation services. One respondent reported that one HB-NROP had occasional access to other medical specialties including neurology, neurosurgery, plastic surgery, and anesthesiology. With the exception of orthosis and prosthesis, all nonphysician services within publicly funded facilities are covered by BC provincial public health. All but one HB-NROPs included physical, occupational, and speech-language therapy (Table 1) for mobility, hand function, and dysarthria; other services were not readily available despite being common recommendations for outpatient follow-up. Reference Greenberg, Treger and Ring6 The limited coverage and inconsistency of nonphysician services offered at BC HB-NROPs were common concerns for participants. When asked about future initiatives, one physiatrist reported the development of a joint division of neuroscience comprised of PMR, neurosurgery, and neurology in BC Interior. Participants on Vancouver Island reported the development of a stand-alone rehabilitation hospital and expansion of an existing HB-NROP to include physiatrists, neurologists as well as allied health disciplines.
Table 1: Available services at HB-NROPs and community spasticity clinic by region

The community-based spasticity clinic had on-site services such as physiatrists, orthopedic surgery, and neurosurgery with access to neurologists and vascular surgeons. Table 1 outlines the nonphysician services available in the community-based spasticity clinic we surveyed. The clinic has on-site pharmacy, nursing, and orthotics and prosthetics services; however, nursing services were paid for by the clinic with pharmacy and orthotics and prosthetics paid for by clients privately. Physiotherapy and occupational therapy are not on-site, but the clinic is currently trialing the employment of therapists to make these services available. In the community, physiotherapy and many assistive devices including orthoses have limited coverage, and occupational and speech-language therapy are not publicly funded. This causes a barrier to collaborative care as clients could see a physician free of charge, but accessing nonphysician services was often expensive without extended medical benefits. For this reason, the number of community-based NROPs are few.
All participants collaborated using email, fax, phone, or in-person discussions. One physiatrist continues to join weekly team meetings and another physiatrist previously attended weekly team meetings but felt this to be a poor use of time because he seldom followed all patients admitted to the HB-NROP. Formal interdisciplinary joint sessions were reported by three participants, and all participants were willing to collaborate on an as needed basis via telecommunication and informal face-to-face interactions. Two physiatrists were satisfied with the collaborative care at their locations, however, were frustrated by the significant amount of uncompensated work required to maintain high levels of inter-professionalism. Participants affiliated with suburban hospitals and smaller HB-NROPs reported greater levels of collaboration compared to larger urban counterparts. One potential reason is that the physical layout of common workspaces can enable structured and spontaneous communication, information sharing, and impromptu decision-making. Reference Lyson, Ackerman and Lyles7 The second potential reason is that a flexible organizational structure can encourage interdependence and allow for a diffusion of responsibility by shifting the workplace culture away from the traditional hierarchy. Reference Lyson, Ackerman and Lyles7
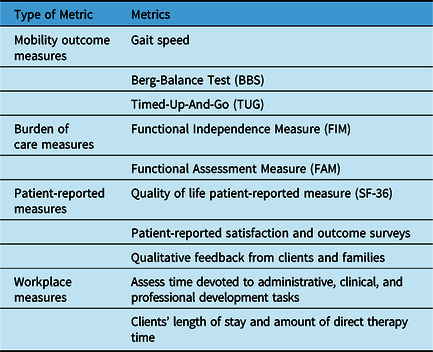
Participants from our survey encouraged the use of standardized outcome measures (Table 2) at the Activity and Participation levels of the International Classification of Functioning, Disability and Health as well as client-reported outcome measures including satisfaction surveys and qualitative feedback to justify the need for HB-NROP services and prevent budget cuts. We found no standardization of measures among BC HB-NROPs nor did participants comment on how the measures were being used in their respective HB-NROP. Evidence does support the use of impairment-based outcome measures such as the Functional Independence Measure and Timed-Up-and-Go to predict the amount of care required Reference Grrznger, Cotter, Hamilton and Fiedler8 and risk of falling, Reference Kyrdalen, Thingstad, Sandvik and Ormstad9 respectively. Other systems-level metrics are summarized by the Canadian Stroke Best Practices. 5
Table 2: Recommended metrics to monitor effectiveness of HB-NROPs
Limitations of our investigation include convenience sampling techniques to interview 15 healthcare providers in BC. Therefore, we had less representation from Interior BC and Vancouver Island compared to Greater Vancouver and no representation from Northern BC. Our assessment had three nonphysician participants. This biased our results to be more reflective of physiatrists’ perspectives and limits our ability to compare BC HB-NROPs in a standardized manner. Our project did not involve client participants when exploring access to outpatient rehabilitation services. Our findings are strictly provider-based perspectives.
Outpatient rehabilitation is a cost-effective method of reducing morbidity and mortality by focusing resources directly on rehabilitation therapy and reducing hospital and nursing costs of inpatient rehabilitation and acute care hospitals. Reference Tam, Mac, Isaranuwatchai and Bayley10 On average, 3 hours of outpatient therapy costs $177.65 CAD which is the equivalent of one-third of the cost of a rehabilitation bed day ($509 CAD) and one-quarter the cost of one alternate level of care day in acute care ($698 CAD). Reference Tam, Mac, Isaranuwatchai and Bayley10 Although an interdisciplinary approach for patients with neurological conditions can lead to better patient outcomes at no more cost to the healthcare system, Reference Wade4 BC HB-NROPs do not have a standardized interdisciplinary model of care nor assessment of outcome measures for patients with neurological conditions. There are differences in inclusion and exclusion criteria, medical and nonphysician services offered, and outcome measures utilized across regions of BC. Outside the hospital, administrative and financial barriers limit nonphysician clinicians from working within physician practices. To improve access to interdisciplinary outpatient rehabilitation care, future projects should evaluate the demand for outpatient rehabilitation services in BC by engaging conversations between frontline clinicians, the BC Provincial Rehabilitation Working Group and rehabilitation administers as well as acute care and ambulatory care directors. An economic benefits analysis of interdisciplinary outpatient neurological rehabilitation could be performed to advocate for improved access to rehabilitation services.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2022.37.
Declaration of Competing Interest
We have no competing interests to disclose.
Statement of Authorship
All authors contributed to the study design and implementastion. NC and AP collected the results, performed the analysis, and drafted the manuscript. All authors revised the manuscript ansd approved the final version.




