Median nerve compression occurs more commonly at the wrist, resulting in carpal tunnel syndrome (CTS). Anterior interosseous syndrome (AIS), pronator teres syndrome (PTS), and the entrapment at Struthers’ ligament are rare and uncommon syndromes with proximal median neuropathy (PMN). A very rare condition, mimicking PTS, exists, deriving from proximal median nerve compression occurring next to the entrance to the canalis brachialis, near the inferior border of pectoralis major muscle. Our report describes the clinical and electrodiagnostic findings in a patient who developed a PMN due to bilateral external compression of median nerve at the axilla against the superior edge of the back of a chair, while he was sitting in an obligate position to have a back tattoo (Figure 1A). The patient, a previously healthy 30-year-old man, complained of painful paresthesia and grip weakness of both hands, in particular the right one, developing just after rising from the chair. The burning paresthesia remained restricted to the thumb, index, and middle finger of both hands without radiating up to the forearm and was associated with weakness of the wrists and difficulty in flexing the three lateral fingers of both hands.
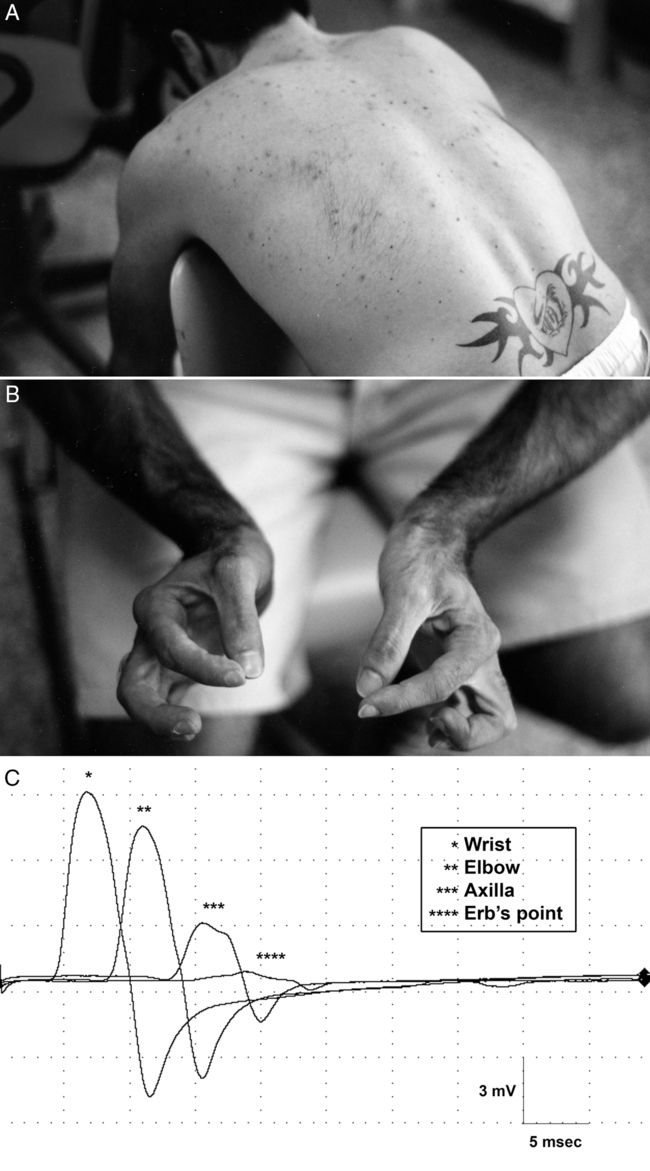
Figure 1: Obligate arms position with bilateral external axilla compression (A). Typical bilateral “pinch deformity” of the hands (B). Conduction block between Erb’s point and the axilla in right median nerve (C).
Symptoms remained unchanged with burning sensation, more noticeable at night, until the patient was seen in the Electromyography (EMG) Laboratory 4 weeks later.
Personal and familiar history was negative for inherited neuropathies or neurological diseases.
Clinical examination showed bilateral hand hypoesthesia in median nerve distribution, paresis of the hand and forearm median-innervated muscles with a typical bilateral pinch deformity (Figure 1B). Pain could not be provoked with forearm pronation. Physical evaluation revealed decreased strength in all the muscles innervated by the median nerve, with different degrees of impairment. Strength in forearm pronation was mildly reduced on the left side (4/5 Medical Research Council (MRC) scale) and moderately reduced on the right side (3/5 MRC scale). Weakness of flexor digitorum profundus (FDP) of the right index finger (3/5), right flexor pollicis longus (FPL) (2/5), pronator quadratus (PQ), and right abductor pollicis brevis (APB) (1/5) muscles was present. Left upper extremity strength was also slightly reduced: FDP 4/5, FPL 3/5, PQ, and APB 2/5. All other proximal and distal muscles showed normal strength. Deep tendon reflexes were present and bilaterally symmetrical; cranial nerve examination was normal and plantar responses were flexor.
EMG detected profuse denervation in all median-innervated muscles, including the pronator teres (PT) muscles. Fibrillations, positive sharp waves, and few polyphasic motor unit potentials (MUPs) were present in FDP, FPL, PQ, and APB of both sides, more at right. The other upper and lower limbs muscles were tested and showed normal EMG findings. In particular, the following muscles were bilaterally tested and were silent at rest, with normal MUPs on volition: trapezius, rhomboids, serratus anterior, supra- and infraspinatus, deltoid, biceps and triceps brachii, brachioradialis, flexor carpi ulnaris, extensor carpi radialis and ulnaris, extensor indicis proprius, first dorsal interosseous, abductor digiti minimi. In the lower limbs, the muscles bilaterally tested were vastus lateralis and medialis, biceps femoris, gastrocnemius, tibialis anterior and posterior, peroneus longus, soleus, extensor digitorum brevis and longus.
Motor conduction studies (MCS) and sensory conduction studies (SCS), including H reflexes and F waves, were performed to exclude inflammatory or inherited neuropathies, including hereditary neuropathy with liability to pressure palsies. MCS were examined segmentally to verify the presence of conduction blocks. SCS showed regular proximal velocities and amplitudes, while MCS revealed presence of a conduction block between Erb’s point and the axilla in both median nerves, more evident at right (Figure 1C). Data conductions from contemporaneous evaluation of responses to Erb’s point stimulation recorded from different muscles (deltoid, biceps and triceps brachii, and abductor digiti minimi) innervated by axillary, musculocutaneous, radial and ulnar nerves, were normal, without proximal conduction block. The distal sensory and motor conduction of radial, ulnar, and median nerves was performed. Tibial and common peroneal motor nerves and sural and peroneal sensory nerves were also examined.
Computed tomography (CT) scan of the chest and axilla was performed and revealed no abnormalities. The patient was treated for 1 month with oral corticosteroids (prednisone 50 mg/day for 10 days and 20-day tapering), obtaining improved muscle strength and a dramatic decrease in the hands’ burning paresthesia. Six weeks later, strength of median-innervated muscles had improved to almost normal; there was a slightly reduced light touch sensation over the tip of the right thumb, index, and middle finger and a mild residual weakness of the right FPL, PQ, and APB.
EMG of FDP, FPL, PQ, PT, and APB showed polyphasic MUPs; few fibrillation potentials persisted only in the right PT. The patient gradually and completely recovered his strength in 6 months but distal mild paresthesias persisted for 5 months. MCS and EMG at 8 months showed disappearance of conduction block between Erb’s point and the axilla in both median nerves and normal EMG findings with increased long-duration polyphasic MUPs in median-innervated muscles.
Neuropathies of the median nerve proximally to the forearm are unusual lesions. In a large series Reference Gross and Jones1 of 4838 EMG examinations, only 17 patients (0.35% of patients) showed PMNs, including AIS, PTS, and entrapment at the ligament of Struthers.
These unusual syndromes can be differentiated from CTS, thoracic outlet syndrome, brachial plexopathy, and cervical radiculopathy based on clinical presentation, needle EMG examination, and nerve conduction findings.
Most commonly reported PMNs etiologies include trauma, compression or overuse of PT, and humerus fracture. Reference Gross and Jones1–Reference Soubeyrand, Melhem, Protais, Artuso and Crézé5 When the median nerve is entrapped proximally to the wrist, precise anatomic localization of damage is difficult to verify and the conservative treatment is suggested. Reference Seki, Nakamura and Kono6 In PMNs, nerve conduction findings usually are not a sensitive indicator of damage, and conventional conduction techniques in the majority of PMNs patients document motor or sensory conduction block or slowing only in rare cases. Reference Gross and Jones1,Reference Buchthal, Rosenfalck and Trojaborg7,Reference Hartz, Linscheid, Gramse and Daube8
Moreover, needle examination does not allow to differentiate a median nerve lesion at the PT from a more proximal lesion. In our clinical case mimicking a PTS only conduction studies, confirming motor conduction blocks across the median nerve most proximal segment, could demonstrate and confirm PMN, attributable to a focal proximal demyelinative compressive nerve lesion.
Disclosures
The authors report no conflicts of interest.
Statement of authorship
GP designed and conceptualized the study; GP, DS, and PP drafted the manuscript for intellectual content and revised the manuscript for intellectual content.



