A 40-year-old man was referred for right eye vision loss. He was diagnosed with right herpes zoster ophthalmicus (HZO) manifest by a positive Hutchinson’s sign (skin lesions on the side and tip of the nose) 1 month prior to presentation and treated with oral valacyclovir 1 g TID for 10 days. Two weeks prior to presentation he developed a right hypertensive anterior uveitis (anterior chamber (AC) cells and elevated intraocular pressure of 32 mm Hg) and was treated with topical prednisolone acetate 1% QID and brimonidine–timolol eye drops BID to the right eye. Three days prior to presentation, he noticed significant blurring of his central vision. At presentation, visual acuity (VA) was counting fingers (CF) at 1 foot in the right eye and 20/20 in the left eye with a right relative afferent pupillary defect. Humphrey visual field testing demonstrated a dense central scotoma with a mean deviation of -16.69 dB and was normal in the left eye (Figure 1). AC was quiet and his optic nerves and retina appeared normal. A right retrobulbar optic neuropathy was diagnosed and magnetic resonance imaging of the orbits and brain was performed, which revealed enhancement of the right optic nerve (Figure 2). Given his history of HZO in close temporal relationship to the optic neuropathy, right herpes zoster optic neuropathy (HZON) was the likely etiology. This was confirmed with an AC paracentesis that detected Varicella Zoster Virus (VZV) by real time polymerase chain reaction (PCR). A lumbar puncture was performed and demonstrated 23 nucleated white cells (97% lymphocytes), a mildly elevated protein (0.58 g/L) and normal glucose. VZV was not detected by PCR in the cerebrospinal fluid (CSF).

Figure 1: Humphrey 24–2 SITA-Fast visual fields at presentation (left panel) demonstrating a dense central scotoma. The central scotoma improved with intravenous acyclovir 10 mg/kg every 8 h as seen 4 d (middle panel) and 16 d (right panel) after treatment initiation.
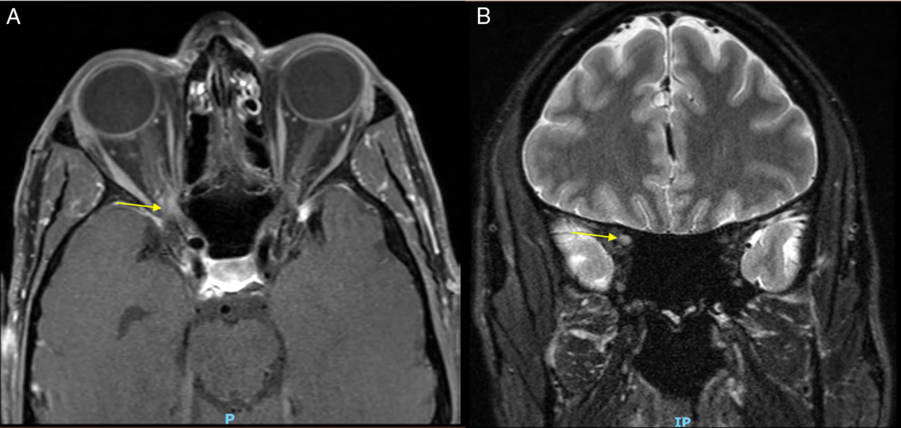
Figure 2: Axial T1-post gadolinium magnetic resonance imaging (MRI) of the orbits demonstrating right optic nerve enhancement (A; arrow). Coronal T2 MRI images demonstrating increased T2 signal in the intracanalicular optic nerve (B; arrow).
He was promptly treated with intravenous acyclovir 10 mg/kg q8h for 7 d followed by valacyclovir 1 g TID. Three days after initiating this treatment, he developed recurrent anterior uveitis with 1+ cells and was re-started on topical prednisolone acetate 1% QID. After 7 d of intravenous treatment, his VA was 20/80 and the central scotoma was much less dense (mean deviation -5.14 dB). Two weeks after initiating intravenous acyclovir, his VA returned to 20/20 and his visual field was normal. He continued to have a chronic anterior uveitis and required topical prednisolone eye drops 6 months after presentation. His VA at 6-month follow-up was 20/20 in both eyes with a normal visual field.
HZON can be a devastating complication of HZO and complete recovery of vision is rare as only modest visual recovery is expected in about 50% of patients. Reference Kedar, Jayagopal and Berger1 In our review of literature, we retrieved 32 cases of HZON with a final visual outcome of 20/20 reported in 3 cases. Reference Freitas-Neto, Cerón, Pacheco, Pereira, Ávila and Foster2–Reference Singh, Karmacharya, Rizyal and Rijal4 The presenting visual acuity was 20/200 in two cases and 20/120 in one case. Reference Freitas-Neto, Cerón, Pacheco, Pereira, Ávila and Foster2–Reference Singh, Karmacharya, Rizyal and Rijal4 Since our patient started with CF vision, he represents the largest recovery to normal vision reported in literature. In the three cases that returned to 20/20, treatment included oral or intravenous corticosteroids in all cases. Reference Freitas-Neto, Cerón, Pacheco, Pereira, Ávila and Foster2–Reference Singh, Karmacharya, Rizyal and Rijal4 However, the use of corticosteroids in the treatment of HZON remains controversial as there are no randomized controlled trials or prospective studies to support its use. Opponents of corticosteroid use in HZON argue that there is a risk of VZV retinitis with evidence stemming from case reports of patients with optic neuropathies who were treated with corticosteroids when the diagnosis of herpetic disease was not yet established. Reference Nakamoto, Dorotheo, Biousse, Tang, Schiffman and Newman5,Reference Friedlander, Rahhal, Ericson, Arrevalo, Hughes and Levi6 It remains unknown whether these patients would have developed herpetic retinitis with co-administration of systemic antivirals. In our review of the literature, 62% (20/32) of HZON cases were treated with systemic corticosteroids with improvement observed in 65% (13/20) of these cases. In comparison, our literature review revealed that only 12.5% of HZON cases (4/32) were treated with antivirals but without systemic corticosteroids. In these four cases, the patients’ VA improved from hand motion to 20/50, 20/40 to 20/25, 20/80 to 20/50, and hand motion to 20/60, after 4, 2, 2, and 6 weeks of antiviral therapy, respectively. Our case argues that complete recovery of vision can be achieved without systemic corticosteroid use and emphasizes the importance of controlled studies to assess the efficacy of steroid co-administration with antivirals in HZON.
It is unclear whether there is a benefit to intravenous compared to oral antiviral medications in treating HZON and whether this played a role in our patient’s recovery. Oral valacyclovir has advantages to oral acyclovir with a higher bioavailability and safety profile. Reference Aizman, Johnson and Elner7 Many studies indicate that a maximum dose of oral valacyclovir (2 g QID) is comparable to intravenous acyclovir 10 mg/kg q8h in terms of area under the curve, but lower in terms of peak concentration. Reference Aizman, Johnson and Elner7,Reference Beutner8 However, our review of literature demonstrated that no HZON case was treated with a dose as high as oral valacyclovir 2 g QID, with the highest dose being 1 g TID in five cases. Reference Freitas-Neto, Cerón, Pacheco, Pereira, Ávila and Foster2 The higher dose equivalent achieved with intravenous acyclovir may have been important in our patient’s recovery. Some have advocated for oral valacyclovir over intravenous acyclovir because of a better safety profile due to lower peak concentration and good central nervous system penetration. Reference Beutner8 Intravenous acyclovir 15 mg/kg q8h is recommended for immunocompromised individuals or those in which lower doses are not effective. Reference Aizman, Johnson and Elner7 Intravenous delivery has some advantages since drug delivery is performed under supervised settings and patient compliance is essentially guaranteed. However, this requires hospital admission or dedicated infusion clinics which accrues additional healthcare resources and costs. Our review of the literature demonstrated that 8 of 32 HZON cases were treated with intravenous antivirals whereas 16 cases received only oral antivirals. Further studies are required to assess whether there is any advantage to oral or intravenous delivery.
Confirmatory testing in HZON is important since the temporal relationship to HZO is suggestive but not definitive for HZON diagnosis. Patients may develop other optic neuropathies in close relationship to HZO such as non-arteritic anterior ischemic optic neuropathy, which can be precipitated by an intraocular pressure spike seen with the hypertensive uveitis caused by VZV. Our case suggests that AC paracentesis can be helpful for confirming VZV etiology in retrobulbar HZON when there is no visible associated intraocular inflammation. Our patient had a positive VZV PCR as a result of incomplete treatment of the anterior uveitis and this flared later in the course of his disease. The case also suggests that the AC was a higher yield location compared to CSF even with the retrobulbar location, which is contiguous with the CSF space in the orbit. We therefore suggest that AC paracentesis be considered in equivocal cases of HZON.
Conflicts of Interest
All authors have no conflicts of interest and disclosure to declare.
Statement of Authorship
Conception and design (PHY; AR; JAM), data extraction (PHY; AR; JAM), manuscript preparation (PHY), final approval (JAM). All authors have seen and approved the final version of the manuscript for publication.




