Orbital myositis, a subgroup of idiopathic orbital inflammatory syndromes (IOIS), is a rare inflammatory disorder that primarily involves extraocular eye muscles.Reference Montagnese, Wenninger and Schoser 1 Patients typically present with subacute onset of unilateral orbital or periorbital pain, restricted eye movements, proptosis, and conjunctival hyperemia.Reference Pakdaman, Sepahdari and Elkhamary 2 We describe here two patients diagnosed with orbital myositis and one with an orbital isolated form of granulomatosis with polyangiitis (GPA/Wegener’s) who have different clinical presentations and neuroradiological features in order to draw attention to this underrecognized condition.
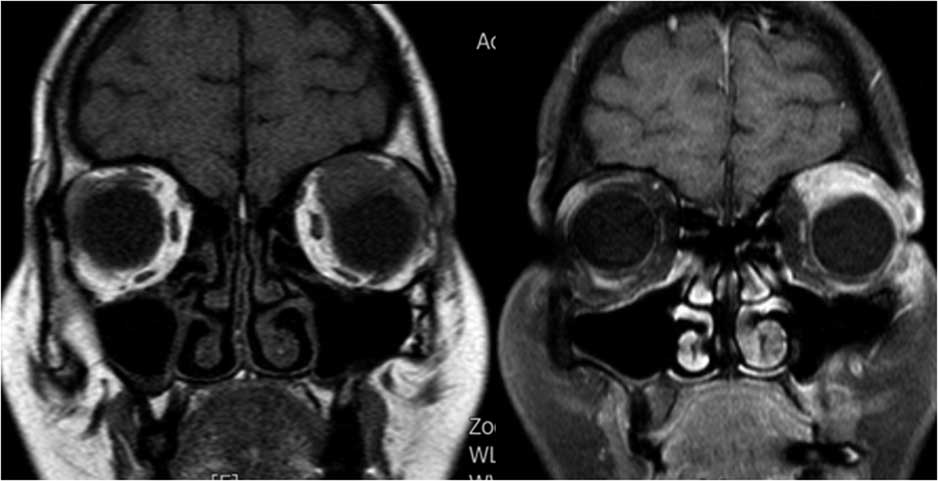
Case 1: A 42-year-old female presented with a 2-week history of left-eye ptosis and a moderate orbital pain. Clinical examination showed a marked ptosis on the left eye (Figure 1a). Visual acuity was normal, and there was no other ocular movement abnormality except for slightly limited elevation of the left side. Levator excursion was mildly reduced on the left side compared to the right. Laboratory tests revealed only a slightly elevated C-reactive protein (CRP) and sedimentation rate, but other investigations, including complete blood count (CBC), thyroid function test (TFT), antithyroid antibodies, anti-nuclear antibody (ANA), anti-neutrophil cytoplasmic autoantibody (ANCA), viral serology, IgG4 levels, and anti-acetylcholine receptor (AChR) antibodies were all normal. Orbital magnetic resonance imaging (MRI) showed enlargement and contrast enhancement of the left superior rectus and left levator palpebrae superioris (Figure 1b). Cerebrospinal fluid (CSF) examination was unrevealing. Brain MRI, intracranial MR angiography, and chest CT revealed no abnormalities. Treatment with intravenous methylprednisolone (1 g/day for 3 days) was initiated and followed by oral prednisolone (1 mg/kg/day). Symptoms gradually resolved, and a clear improvement occurred over the following 3 weeks (Figure 1c). Repeated MRI scan performed 2 months after the first MRI revealed marked improvement of the levator palpebrae swelling (Figure 1d). Steroids were slowly reduced and stopped over the following 3 months. The patient remained symptom-free at follow-up.

Figure 1a Isolated left total ptosis.
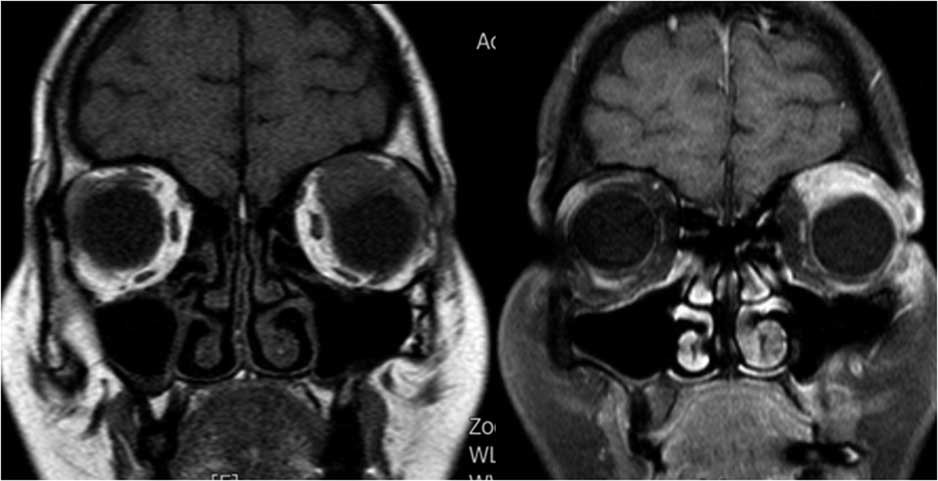
Figure 1b Coronal MRI scan of orbits shows enlargement and contrast enhancement of the left superior rectus and left levator palpebrae superioris.

Figure 1c Ptosis resolved after steroid treatment.
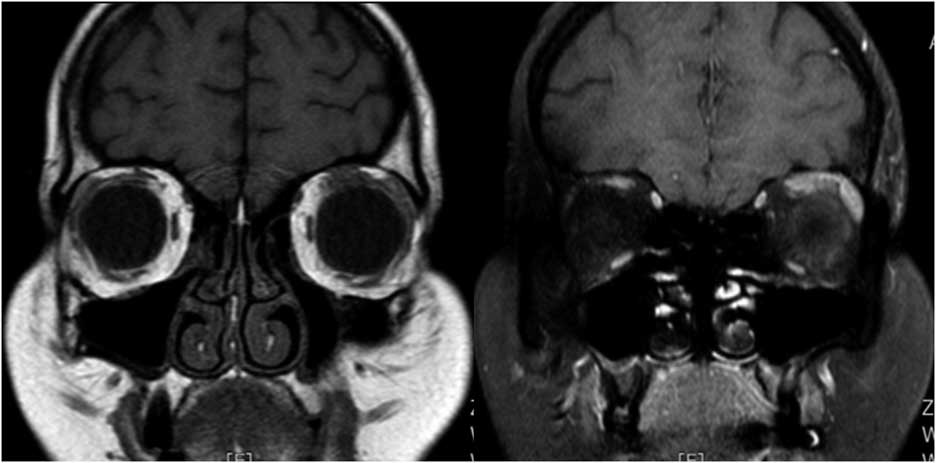
Figure 1d Repeat MRI after 2 months revealed marked improvement of the levator palpebrae swelling.
Case 2: A 33-year-old male presented with right conjunctival redness and retrobulbar pain exacerbated by eye movements that had lasted for a month. In the following weeks, he developed diplopia and right-eye ptosis. Neurologic examination demonstrated right-side ptosis and proptosis. In primary gaze, he had right exotropia. Right extraocular movements were totally restricted in elevation, depression, and adduction, and he had mild limitation of abduction (Figure 2a). Pupils reacted normally to light with mild right-eye mydriasis. Orbital MRI showed edema and enhancement of the right lateral rectus muscle partly involving surrounding fat (Figure 2b). CSF examination did not show any abnormalities. Subsequent investigations did not show any abnormalities in CBC, TFT, antithyroid antibodies, ANA, ANCA, IgG4 levels, and viral serology. Brain MRI, intracranial MR angiography, and chest CT were also normal. He received intravenous methylprednisolone (500 mg/day for 5 days) followed by oral prednisolone (1 mg/kg/day), and his symptoms improved slowly over 2 months, and he gained recovery in ocular motility within 5 months, except for diplopia in extreme lateral gaze. After treatment, his MRI showed resolution of edema and enhancement in the right lateral rectus 2 months later (Figure 2c).
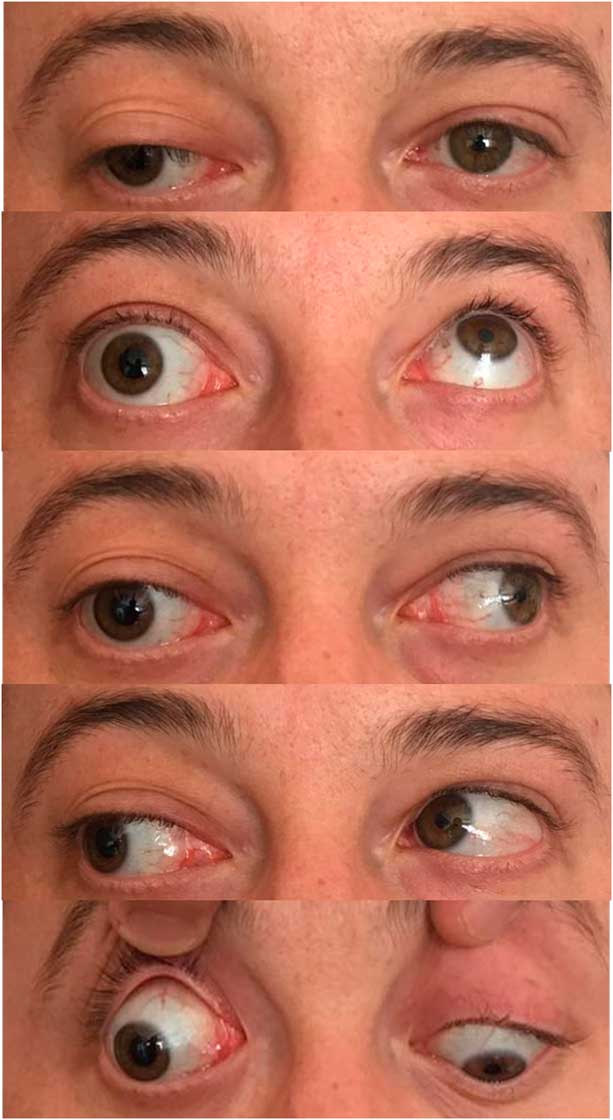
Figure 2a The upper image shows the eyes at primary position. There is right proptosis and periorbital edema. Patient had marked limitation of the right eye in elevation, depression, and adduction, and moderate limitation in abduction.
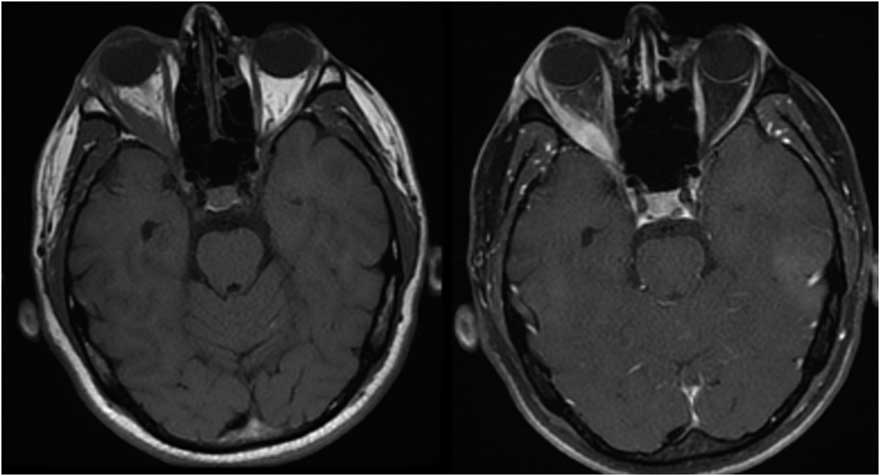
Figure 2b Axial MRI scan demonstrating right lateral rectus thickening and contrast enhancement.
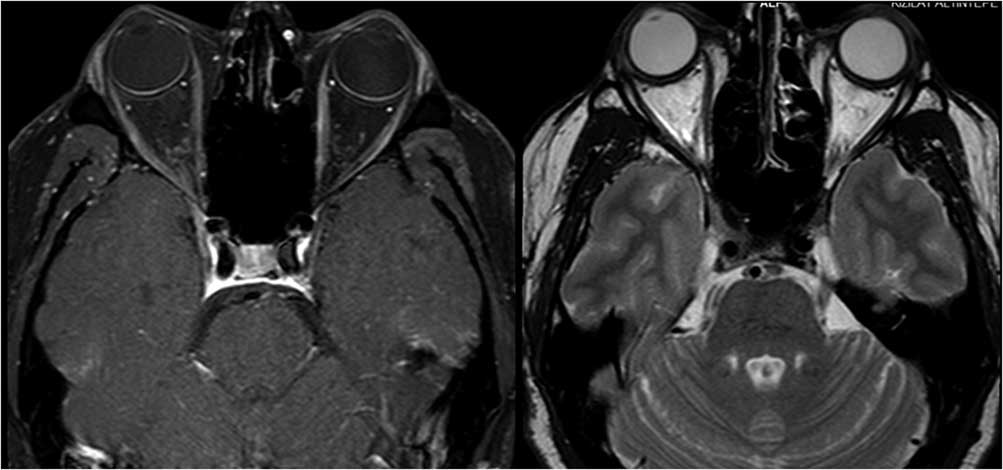
Figure 2c Repeat MRI 2 months later shows resolution of edema and enhancement in the right lateral rectus.
Case 3: A 74-year-old male was admitted with a 1.5-year history of blurred vision and progressive bulging of both eyes. The symptoms started after nasolacrimal duct intubation surgery to treat lacrimal drainage obstruction. He had a past medical history of vision loss in his left eye due to trauma 10 years previous, as well as erosion and perforation of the nasal septum 2 years before. Neurological examination showed bilateral proptosis that was more prominent on his right eye, and his extraocular movements were limited bilaterally in all directions (Figure 3a). MRI of the orbit identified bilateral hyperintensities, enlargement, and contrast enhancement in extraocular muscles. Brain MRI findings included linear dural thickening and enhancement on the anterior frontal and temporal lobes, inflammation and enhancement on the maxillary, frontal, and sphenoid sinuses, and a nasal septum defect (Figure 3b). Investigations revealed a mild increase in CRP and sedimentation rate, slightly low T3 and T4 levels, and normal thyroid-stimulating hormone, CBC, antithyroid antibodies, viral serology, IgG4 levels, ANA, and anti-AChR antibodies. The anti-proteinase ANCA (anti-PR3 ANCA) level was 72.3 U/ml (>20 U/ml), and p-ANCA was found to be positive. Therefore, a diagnosis of orbital inflammation due to GPA was established. Chest CT revealed calcific lung nodules and bilateral apical pleuroparenchymal fibrotic density changes. Histopathological investigation of nasal biopsy revealed chronic inflammation. He was treated with high-dose IV methylprednisolone (1 mg/day for 5 days) followed by 60 mg/day oral prednisolone. He responded with a prompt reduction of proptosis and lid edema and a slight improvement in ocular movement over the 6-month period. Treatment continued with prednisolone tapering and azathioprine.
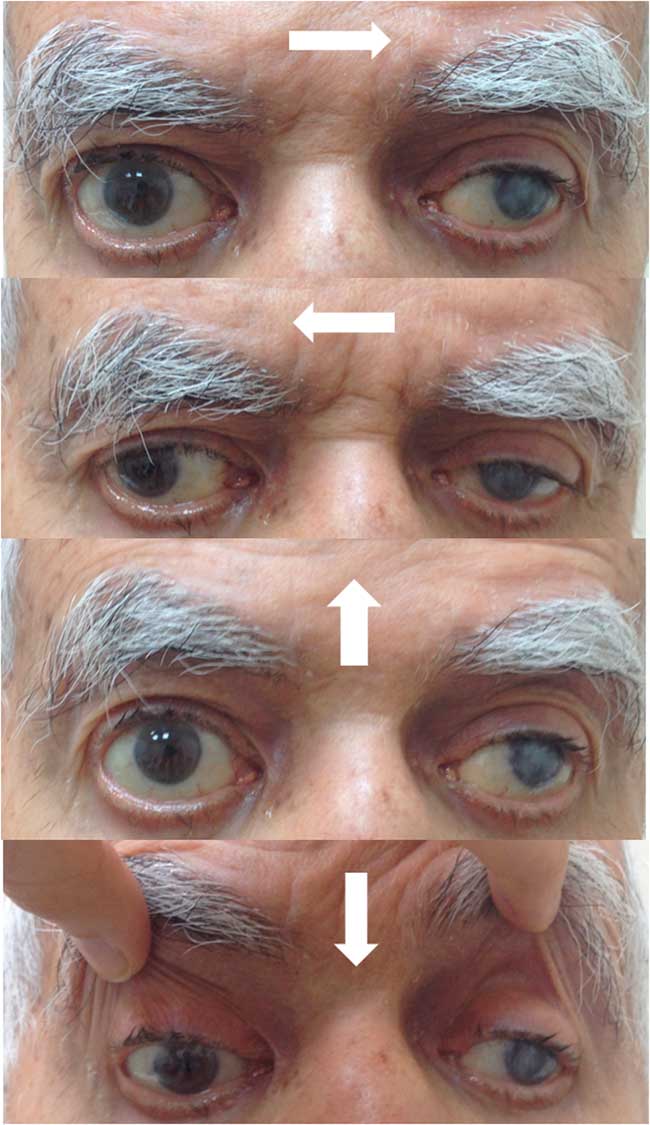
Figure 3a Patient has bilateral proptosis and bilateral restriction of extraocular eye movements in all directions.
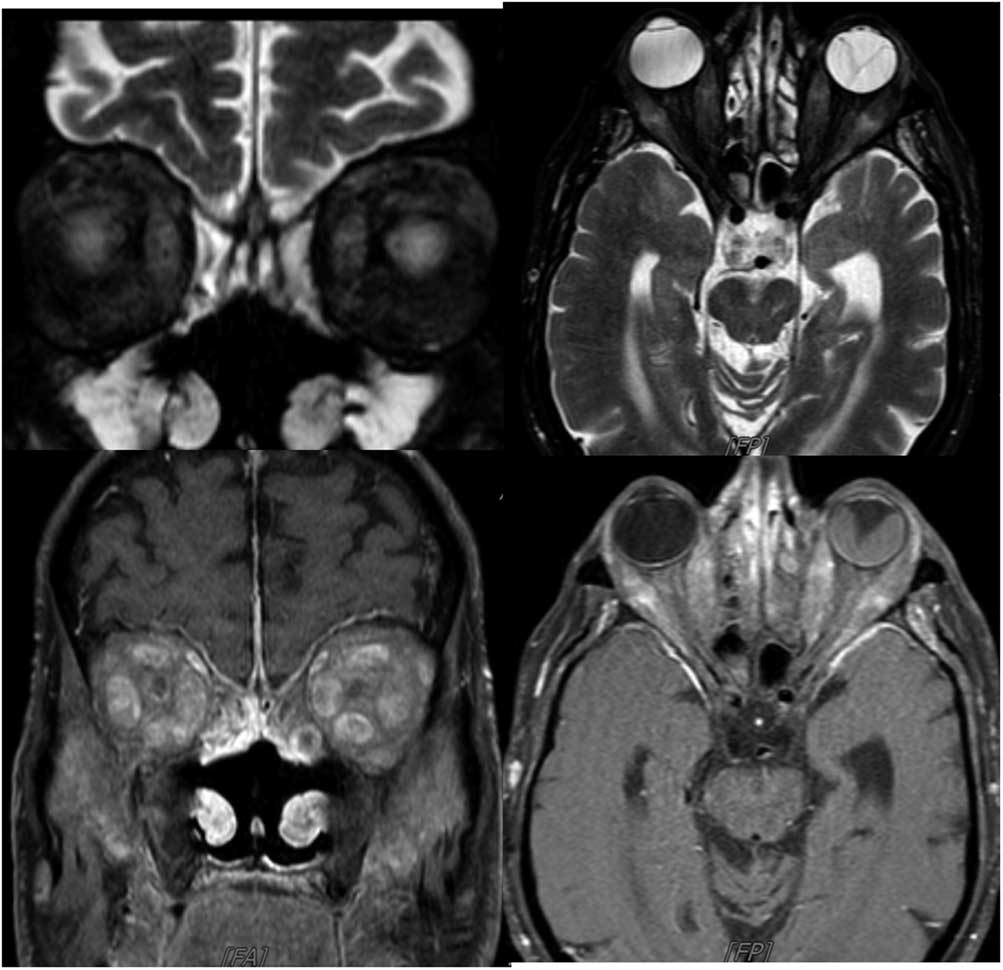
Figure 3b Axial and coronal MRI showing bilateral hyperintensities, enlargement, and contrast enhancement in extraocular muscles, linear dural thickening, and enhancement on the anterior frontal and temporal lobes, enhancement on the maxillary, frontal, and sphenoid sinuses and nasal septum defect. Right bulbus oculi was normal, whereas left bulbus oculi revealed retinal detachment.
Our three patients showed that orbital myositis has a large and underrecognized spectrum. The horizontal recti are reported as the most frequently involved muscles, followed by the superior and inferior recti.Reference Schoser 3 , Reference Önder, Bilgin, Köşkderelioğlu and Gedizlioğlu 4 Unilateral single-muscle involvement is the most frequently known presentation, but multiple or bilateral involvement can also be seen.Reference Spindle, Tang and Davies 5 However, rare presentations such as our first case are of semiological interest: marked ptosis secondary to inflammation in the levator palpebral muscle.Reference Almekhlafi and Fletcher 6
Diagnosis is usually established based on clinical presentation, neuroradiological findings, and exclusion of other causes in conjunction with laboratory results bringing additional clues for specific etiologies, such as in case 3. Contrast-enhanced orbital MRI is the most sensitive diagnostic imaging modality. The classical picture of orbital myositis includes a unilateral thickening of one or two extraocular muscles involving surrounding fat, tendon, and myotendinous junction. Contrast-enhanced T1-weighted images and T2-weighted images with fat suppression that make inflammatory lesions more visible within the orbit should be obtained.Reference Pakdaman, Sepahdari and Elkhamary 2 Histological confirmation with orbital biopsy is recommended in steroid-resistant cases to exclude the presence of neoplastic tissue or lymphoproliferative processes or if the imaging suggests the presence of an orbital tumor.Reference Montagnese, Wenninger and Schoser 1
As in our third case, bilateral orbital involvement may be the first or only clinical presentation in patients with systemic or limited forms of GPA.Reference Muller and Lin 7 , Reference Santiago and Fay 8 GPA is a systemic necrotizing vasculitis of the small to medium-size vessels, generally involving lungs and kidneys and often affecting the orbit and ocular structures.Reference Muller and Lin 7 , Reference Santiago and Fay 8 High levels of anti-neutrophil cytoplasmic antibody serology for cytoplasmic ANCA reactive against proteinase 3, as well as perinuclear ANCA reactive against myeloperoxidase, are highly useful in GPA diagnosis.Reference Muller and Lin 7 , Reference Santiago and Fay 8
We conclude that IOIS, and particularly orbital myositis, may involve different structures in the orbit. A consensus guideline for diagnosis and management of orbital myositis will be very useful to increase awareness and implement proper investigation and treatment strategies.
Acknowledgments
This study was presented in preliminary form as a poster at the Third Congress of the European Academy of Neurology in Amsterdam (2017).
Disclosures
Leyla Baysal Kirac, Arman Cakar, Yagmur Turkoglu, Hazal-Ceren Ak, Doga Coskun, Sibel Ustun-Ozek, Serap Uçler-Yaman, and Betul Baykan hereby declare that they have no conflicts of interest to disclose.
Statement of Authorship
Baysal Kirac: concept, design, writing of paper.
Cakar, Turkoglu, Ak, Coskun, Ustun-Ozek: collecting data, analysis of data.
Uçler-Yaman: supervision of development of work, help in data interpretation and manuscript evaluation.
Baykan: revised manuscript critically for important intellectual content.