A healthy 66-year-old male was admitted to our emergency room (ER) with fever and severe bilateral visual loss (VL). The day before accessing the ER, the patient had undergone an apparently uncomplicated intramuscular paravertebral cervical injection of 20 ml of an oxygen-ozone mixture (ozone concentration of 20 µg/ml) and lidocaine 2%. It was the penultimate administration of a five-injection cycle of oxygen-ozone therapy (OOT) for the treatment of cervical herniated disc symptoms. About five minutes after the procedure, severe frontal headache, confusion, nausea, and vomiting occurred. Progressive bilateral blindness, memory impairment, and restlessness occurred about half an hour later.
Once in ER, one hour after the onset of VL, the patient presented with fever up to 38.5 °C. There was no evidence of significant hemodynamic changes. Blood tests showed neutrophilic leukocytosis (WBC count: up to 19630/mmc with 84.6% neutrophils), C reactive protein 19.1 mg/l, and value of procalcitonin in the normal range. Blood cultures were performed. The ophthalmological evaluation was negative; the neurologic examination showed global amnesia, temporal disorientation, and bilateral cortical blindness, with sparing of the pupillary light reflex.
A chest X-ray was negative for consolidations or interstitial involvement; the head computed tomography (CT) angiography was negative for major vessel occlusion or ischemia, while magnetic resonance imaging (MRI) showed diffusion-weighted imaging (DWI) and fluid attenuated inversion recovery (FLAIR) hyperintense lesions in the right cerebellar hemisphere and in the vermis and further alterations in the occipital parietal cortex bilaterally (Figure 1A and B) with normointense ADC maps (Figure 1C and D) suggestive of posterior vasogenic edema.
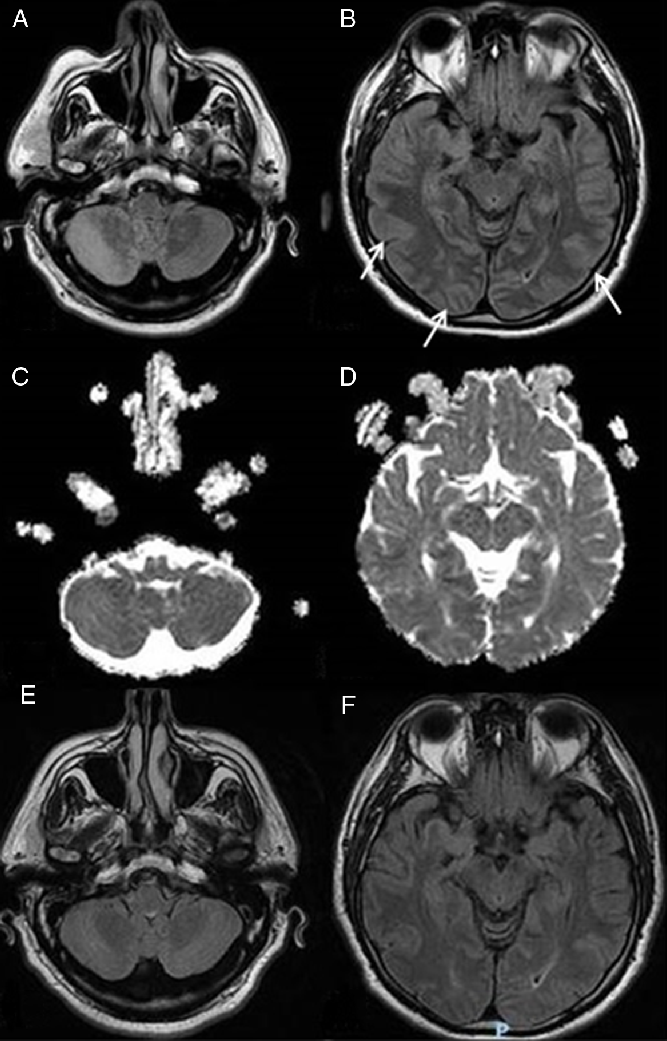
Figure 1: MRI findings at the acute onset and at the follow-up. (A and B) FLAIR MRI scans showing lesions of the right cerebellar hemisphere and of the cerebellar vermis and in the parieto-occipital lobes at the acute onset (arrows pointing at the parieto-occipital lesions). (C and D) Normointense ADC maps at the acute onset. (E and F) FLAIR MRI sequences showing a complete resolution of the lesions at the follow-up MRI.
Cerebrospinal fluid (CSF) examination showed hyperproteinorrachia (351 mg/dl) and 11 cells/mmc with normal glucose; microbiological samples were negative for Cryptococcus antigen and molecular and direct exam for bacteria. Empiric therapy with vancomycin, ceftriaxone, and acyclovir was administered.
At the admission to the department of infectious diseases, 24 h later, the patient was stuporous but easily awakened in response to verbal stimuli, well oriented to place but not in time. Bilateral visual impairment was still present, though an initial recovery of left lateral visual field was reported. Fever ceased on the second day of hospitalization. The antibiotic therapy was continued because of the suspicion of a procedure-related sepsis and maintained for a 14-days cycle; antivirals were continued because of the possibility of an overlapping encephalitis. A full recovery of the visual acuity (20/20 in both eyes) and an improvement of the neurological examination occurred on the 9th day. A transthoracic echocardiogram showed no vegetations, blood cultures performed in the ER were sterile, polymerase chain reaction (PCR) for genome of neurotropic viruses from a CSF sample was negative and a clinical ophthalmic evaluation showed no abnormalities. A second brain MRI evaluation performed 14 days later showed a complete resolution of the initial alterations (Figure 1E and F). A neurologic evaluation showed normal visual-spatial perceptive functions. The patient was discharged with the indication of a further outpatient neurologic evaluation that confirmed the complete clinical remission.
This article describes a case of headache, encephalopathy, nausea, vomiting, cortical blindness, memory impairment, and restlessness a few minutes after an intramuscular injection of OOT with complete recovery in 9 days. The brain MRI findings at the clinical onset were consistent with vasogenic edema in the parieto-occipital area that completely receded at the following MRI examination 15 days later. The clinical and radiological findings are suggestive for a posterior reversible encephalopathy syndrome (PRES).Reference Hinchey, Chaves and Appignani1
Other possible causes are less likely. Ischemic stroke can be excluded by the neuroimaging findings (absence of vessel occlusion at the CT angiography scans and complete regression of the alterations at the follow-up brain MRI). Infective encephalitis has been excluded by the laboratory outcomes (normal microbiological CSF analysis), clinical course, and neuroimaging findings.
Ozone has been associated with increased nitrogen monoxide (NO) secretion by endothelium,Reference Sánchez-González, Moro and Castillo-Henkel2 and NO may lead to an alteration of the brain-blood-barrier (BBB) leading to a vasogenic edemaReference Thiel and Audus3 thus leading to the PRES here described.
To date two similar cases during OOT exist in literature, and they both have been diagnosed as vertebrobasilar ischemia but we advance a new possible diagnosis for both of them.
Corea et al.Reference Corea, Amici, Murgia and Tambasco4 described a case of frontal headache, inferior facial nerve palsy, global amnesia, encephalopathy, and bilateral cortical blindness during an intradiscal ozone injection for sciatica. A few days later, the patient experienced generalized tonic-clonic seizures followed by a progressive clinical recovery in 10 days. The MRI showed hyperintense lesions in the T2-weighted and DWI scans of the occipital cortex bilaterally and in the left thalamus. No MRI follow-up was made. The MRI angiography was normal. This case has been diagnosed as a vertebrobasilar ischemia, but the clinical course and the MRI findings are also suggestive for PRES.
Vaiano et al.Reference Vaiano, Valente and De Benedetti5 described a case of severe frontal headache, vomiting, and nausea followed by cortical blindness and encephalopathy. The brain MRI showed multiple hyperintense areas in DWI and FLAIR scans with partial hypointensity in ADC map in the occipito-parietal cortex bilaterally. The patient clinically improved in the following days with complete remission after 9 days. A brain MRI control performed 4 months later showed a partial remission of the T2 hyperintense lesions. This case has been diagnosed as a vertebrobasilar ischemia, and PRES was ruled out for the absence of history of hypertension. The clinical presentation and the MRI findings, however, are suggestive for PRES complicated with partial cerebral ischemia.
In conclusion, ozone therapy for cervical/lumbar disc herniation is a procedure that is considered generally risk-free or as low as 0.1% and has low adverse effects at concentrations used for the therapeutic application (10–40 µg/ml). Our case, together to other mentioned cases, suggests that we need further studies to prove the real safety of this medical treatment and its effect to the BBB.
Statement of Authorship
VN and CP contributed in the acquisition of clinical information and drafting of the manuscript, FAL and GDM contributed in the critical revision of the manuscript, GR and GG contributed in the drafting of the manuscript, and MT contributed in approving the final version of the manuscript.
Conflict of Interest
None of the authors have potential conflicts of interest to be disclosed.



