Acute ischemic stroke (AIS) is a medical emergency with devastating effects. Recent trials have endorsed that endovascular thrombectomy (EVT) has significantly revolutionized the treatment of acute stroke.Reference Goyal, Demchuk and Menon1,Reference Goyal, Menon and van Zwam2 EVT is a resource-intensive procedure and the outcome of EVT should be monitored on a continuous basis. While monitoring EVT data, it is important to identify and remove bottlenecks leading to expedited EVT processes as well as improved patient outcomes.Reference Goyal, Jadhav and Wilson3
Optimizing Patient Treatment In Major Ischemic Stroke with EVT (OPTIMISE) is an ongoing Canadian registry of patients who have undergone EVT, which serves as a quality assurance platform for understanding outcomes post EVT.Reference Stotts, Poppe and Swartz4 As part of this registry, a comparative national statistical feedback on the stroke processes of care is provided to the participating centers. The parameters included in the registry are basic demographics, stroke process metrics, and outcome metrics. One outcome metric is the modified Rankin Scale (mRS) at discharge and at 90 days from the time of treatment.Reference Banks and Marotta5 A score of ≤2 on mRS is considered a good outcome. Manitoba’s only comprehensive stroke center offering EVT is in Winnipeg, Manitoba at the Health Sciences Centre (HSC). We are part of the registry and this study was approved by our institutional ethics board. Importantly, baseline EVT process and outcome data were not collected prior to our initiative. For this study, we compared the outcome (in mRS) at our center to that from the ESCAPE trial (Figure 1).Reference Goyal, Demchuk and Menon1
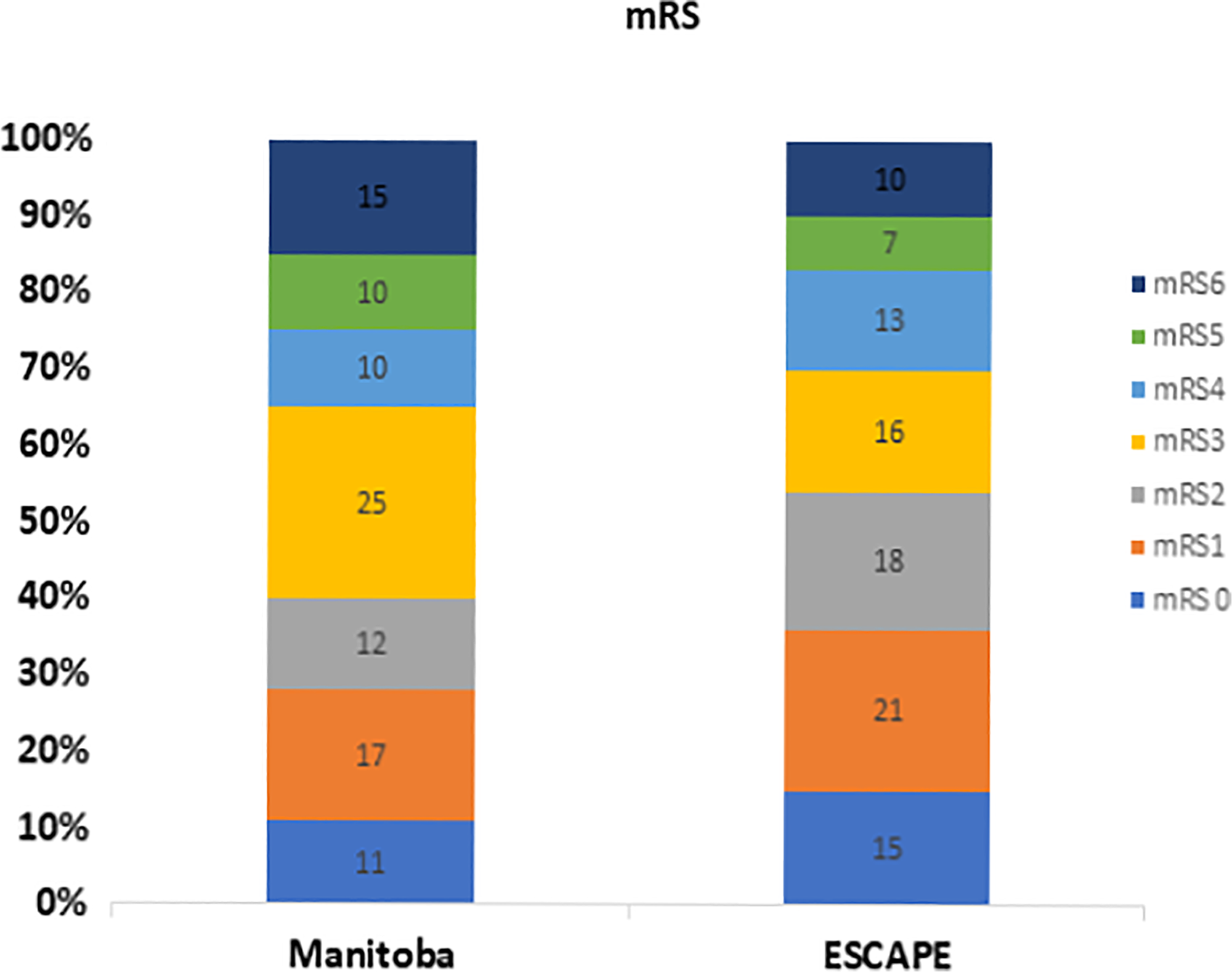
Figure 1: The bar diagram with 90-day mRs of patients with AIS who received EVT at HSC Winnipeg as compared to that from the ESCAPE trial.
In June 2020, a review of 232 consecutive patients who had undergone EVT for AIS between January 1, 2015 and December 31, 2019 was undertaken at our center using a cohort study design. Data were collected using the OPTIMISE clinical record form. All 90-day mRS was obtained by telephone visit. Our stroke process metrics are comparable to the national average. Our median door to recanalization time was 96 min (target is 90 min) with 85% achieving a good recanalization (TICI 2b/3). Significantly less (p < 0.01) patients in Manitoba (68 of 173 (39.3%)) as compared to 54% in ESCAPE trial achieved an mRS ≤ 2 at 90 days (Figure 1). Mortality was seen in 26 out of 173 (15%) of patients in our center compared to 10% patients in the ESCAPE trial (p = 0.17) (Figure 1). The national average was similar to what has been seen in the ESCAPE trial and meta-analysis.Reference Goyal, Demchuk and Menon1,Reference Goyal, Menon and van Zwam2 The median hospital stay was 4 days for patients who underwent EVT in our center. Due to bed occupancy issues and the fact that no acute stroke unit exists, these patients had to be discharged early to other hospitals.
Our study highlights striking results in patients undergoing EVT at HSC. Good outcome was achieved in a significantly lower percentage of patients in Manitoba compared to previous clinical trials.Reference Goyal, Demchuk and Menon1,Reference Goyal, Menon and van Zwam2 Other centers in Canada have shown outcomes from EVT similar to that of clinical trials.Reference Virani, Hu and Christian6 The mortality in patients undergoing EVT was similar to that of other clinical trials.Reference Goyal, Demchuk and Menon1
Though it is imperative to acknowledge that this study does not provide definitive results, it is possible to form judicious interpretations based upon it. It is also crucial to consider there are many factors that cannot appropriately be measured or accounted for when conducting a study of this sort, but the results that have been collected allow analytical conclusions to be drawn. In order to formulate a feasible explanation for this discrepancy in the two outcomes, one must look at the stroke process time intervals and the differing approaches to treatment as well as the different interventions being offered at various facilities. The differences in the baseline patient characteristics should also be considered. Our stroke process metrics are comparable to Canadian benchmarks. Thus, a plausible reason for a significantly poorer patient outcome could be due to a much shorter hospital stay (median of 4 days) after EVT, due to the lack of a stroke unit. Every province in Canada, with the exception being Manitoba, has a stroke unit, which ensures that every patient who suffers a stroke acquires outstanding care by a facility that is highly specialized in the field. Receiving the highest quality of care possible, which can be provided through the utilization of a stroke care unit, maximizes the likelihood of good patient outcomes.
Studies have shown that one of the most effective interventions for stroke patients has been the implementation of a stroke unit in hospitals.Reference Langhorne and Ramachandra7,8 A stroke unit is an organized facility that is primarily dedicated to care for patients who have suffered a stroke. It is a specialized and geographically defined unit, with staff who have expertise in stroke care. This intervention has successfully shown to save lives and decrease dependency after stroke, independent of patient age, sex, initial stroke severity, or stroke type, and was most obvious in units based in a discrete stroke ward.Reference Langhorne and Ramachandra7,8 Our study helps to better comprehend the significant impact of stroke unit care on patient outcomes.
Our study has limitations similar to other small population-based studies. We could not obtain mRS at 90 days in approximately 1/4th (59 of 232) patients treated with EVT. However, most of these patients were treated in the earlier time period. Our study focused on the in-hospital care of acute stroke patients. We did not have information on the demographics and comorbidities in our patients to compare. We did not compare the location of clot, operator’s EVT experience, and serious complication rate. Although these parameters could potentially explain our poor outcome, a treatment with number needed to treat of around 2 should be offered to eligible patients with AIS. Multiple randomized trials were expected to neutralize any confounding introduced by individual operator and center variables, although extrapolation of trial results to any center should be done with caution. The additional benefit of an acute stoke unit has been well established. Our study highlights the need of continuous and ongoing monitoring of results for EVT, which is a very effective but resource intense treatment. Our study also highlights the need to assess the outcomes from intravenous thrombolytics for acute stroke in our center. This has not been assessed yet.
Although Manitoba is the last province in Canada to build a stroke unit,Reference Billeck9 it is well on its way in acquiring this important intervention in acute stroke care for the province. The construction for this stroke unit began in December of 2019 and is said to be fully functional by late 2022. This new 28 bed unit will be constructed at the HSC, Manitoba’s flagship hospital. Not only will this stroke unit drastically reduce treatment costs, but it will also remarkably reduce the probability of death and disability in patients and will, therefore, aid the province with attaining improved patient outcomes. Thus, the implementation of a provincial stroke unit is expected to narrow the gap between Manitoba’s below average patient outcomes and national patient outcomes. Since it is expected that stroke patient outcomes will improve after the stroke unit is functional, our study will serve as an important baseline study to which future studies should be compared to. The execution of an acute stroke unit could seemingly yield great results and could benefit the province of Manitoba tremendously.
Acknowledgements
The authors would like to acknowledge the Department of Internal Medicine, University of Manitoba and CaStor (Canadian Stroke Trials for Optimizing Results) grants for covering part of the study activities.
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Authorship
RT: wrote the first draft of the manuscript; SA: data collection, reviewed the manuscript; AT: treated patients and followed them, reviewed the manuscript; EG: treated patients and followed them, reviewed the manuscript; JM: treated patients and followed them, reviewed the manuscript; JS: conceptualization, data collection, analysis, manuscript preparation, and review.



