Residents of long-term care (LTC) facilities often require and receive care in the emergency department (ED). Moving from LTC to the ED via emergency medical services (EMS), and back involves a series of “transitions in care” (Coleman & Berenson, Reference Coleman and Berenson2004). Suboptimal transitions in care between LTC and the ED lead to increased hospital length of stay, patient dissatisfaction, reductions in quality of care, and adverse events (Callahan et al., Reference Callahan, Arling, Tu, Rosenman, Counsell and Stump2012; Callinan & Brandt, Reference Callinan and Brandt2015; Carson, Gottheil, Gob, & Lawson, Reference Carson, Gottheil, Gob and Lawson2017; Coleman & Berenson, Reference Coleman and Berenson2004; Crilly, Chaboyer, & Wallis, Reference Crilly, Chaboyer and Wallis2006; Manias, Bucknall, Hutchinson, Botti, & Allen, Reference Manias, Bucknall, Hutchinson, Botti and Allen2017; McCloskey, Reference McCloskey2011; Scott, Reference Scott2010). Many promising studies and programs have focused on improving transitions by empowering seniors to manage their own care across settings (Enderlin et al., Reference Enderlin, McLeskey, Rooker, Steinhauser, D’Avolio and Gusewelle2013; Murray & Laditka, Reference Murray and Laditka2010; Parry Coleman, Smith, Frank, & Kramer, Reference Parry, Coleman, Smith, Frank and Kramer2003). Although we value this approach, we also see a need for strategies to improve transitions that do not put the onus wholly on the patient, particularly given the high rates of cognitive impairment among LTC residents. In previous work, we found that 53.5 per cent of LTC residents transferred to the ED have dementia (cognitive performance score [CPS] ⩽ 3), and that 27 per cent have moderate to severe dementia (CPS > 3) (Cummings et al., Reference Cummings, McLane, Reid, Tate, Cooper and Rowe2020). In that study, inconsistent documentation of such basic information as “reason for transfer to acute care” was found among care settings. The present study therefore focuses on efforts to improve consistent documentation of resident health and personal information among care settings.
Communication among care settings is particularly important for the emergency care of seniors, given their high rates of cognitive impairment. Without information on baseline mental status, it is difficult for ED providers to know whether the resident is experiencing a stroke, delirium, or dementia (Terrell et al., Reference Terrell, Brizendine, Bean, Giles, Davidson and Evers2005). Some evidence suggests that patients with cognitive impairment may be particularly vulnerable to gaps in information communication and documentation. A study by Boockvar, Fridman, and Marturano (Reference Boockvar, Fridman and Marturano2005) found that 62 per cent of resident LTC to ED transitions that had no mental status description recorded involved patients who had moderate to severe cognitive impairment.
Information gaps may affect residents’ personal information and thereby the care that they receive during transitions. Without communication of goals of care and advance directives, transitions in care cannot honour resident wishes. Personal items essential to daily life, such as glasses and dentures, are frequently not documented across care settings and may easily be lost or not transported across care settings (Field, Mazor, Briesacher, Debellis, & Gurwitz, Reference Field, Mazor, Briesacher, Debellis and Gurwitz2007; Hammel et al., Reference Hammel, Southall, Jutai, Finlayson, Kashindi and Fok2013; Reid et al., Reference Reid, Cummings, Cooper, Abel, Bissell and Estabrooks2013). These items can be difficult to impossible to replace.
Schoenborn, Arbaje, Eubank, Maynor, and Carrese (Reference Schoenborn, Arbaje, Eubank, Maynor and Carrese2013) found that clinicians regard a lack of standardized communization tools as a barrier to providing care during transitions. Recognizing the importance of communication gaps, health care practitioners (HCP) have called for strategies to improve communications as part of an overall strategy to improve quality of transitions (Griffiths, Morphet, Innes, Crawford, & Williams, Reference Griffiths, Morphet, Innes, Crawford and Williams2014; Manias et al., Reference Manias, Bucknall, Hutchinson, Botti and Allen2017).
Standardized documentation tools hold appeal within health services, particularly given well publicized successes in reducing morbidity and mortality in surgery using simple checklists (Haynes, Weiser, Merry, & Safe Surgery Saves Lives Study Group, Reference Haynes, Weiser and Merry2009; Weiser et al., Reference Weiser, Haynes, Dziekan, Berry, Lipsitz and Gawande2010). In LTC research, Ouslander and colleagues reported success in using a standardized reporting tool about resident health to reduce unnecessary hospitalizations (Ouslander et al., Reference Ouslander, Perloe, Givens, Kluge, Rutland and Lamb2009). Such checklist-style reporting tools have been reported to positively impact HCP communications, as the tools prompt more “key” care items to be discussed among HCPs (Newkirk, Pamplin, Kuwamoto, Allen & Chung, Reference Newkirk, Pamplin, Kuwamoto, Allen and Chung2012). Furthermore, such standardized tools may have independent value as data sources for evaluating health care improvement efforts (Canadian Institutes of Health Information, 2020). A number of studies of emergency transitions of LTC residents have therefore tested standardized communication tools (e.g., forms, e-documentation) to improve communication of critical information among HCPs (Carson et al., Reference Carson, Gottheil, Gob and Lawson2017; Hustey & Palmer, Reference Hustey and Palmer2010; Kelly, Mahoney, Bonner, & O’Malley, Reference Kelly, Mahoney, Bonner and O’Malley2012; Terrell et al., Reference Terrell, Brizendine, Bean, Giles, Davidson and Evers2005; Zamora et al., Reference Zamora, McCall, Patel, Biese, Lamantia and Platts-Mills2012).
Generally, studies of communication between LTC and the ED during emergency transitions have focused on one-way communication between the two sites (e.g., LTC to ED). Through a partnership among clinicians, researchers, and a Canadian provincial health authority, we implemented and evaluated a communication form to maximize inter-facility communication by having HCPs at every transition point (LTC to EMS to ED and back) document LTC resident health, care, and personal information on a two-page paper communication form (hereafter, “the form”).
This article reports the feasibility and utility of form use. We were aware that clinicians sometimes choose not to use standardized tools (Hustey & Palmer, Reference Hustey and Palmer2010; Kelly et al., Reference Kelly, Mahoney, Bonner and O’Malley2012; Terrell et al., Reference Terrell, Brizendine, Bean, Giles, Davidson and Evers2005; Zafirau, Snyder, Hazelett, Bansal, & McMahon, Reference Zafirau, Snyder, Hazelett, Bansal and McMahon2012); that the degree to which standardized tools are completed determines the degree to which they impact patient outcomes (Mayer et al., Reference Mayer, Sevdalis, Rout, Caris, Russ and Mansell2016; Russ et al., Reference Russ, Rout, Caris, Mansell, Davies and Mayer2015), and that HCP motivation to use a tool is an important mediating factor between tools and patient outcomes (Kane et al., Reference Kane, Huckfeldt, Tappen, Engstrom, Rojido and Newman2017).
Therefore, our specific research objectives were to
-
1. Enumerate and evaluate use of the form across transitions;
-
2. Document and assess rates of form and data element completion; including (a) resident information, (b) documents attached, and (c) assistive devices accompanying LTC residents throughout their transition
-
3. Examine HCP assessment of feasibility of use, usefulness, and applicability of the form to their practice
Methods
This study received ethics approval from the University of Alberta Health Research Ethics Board (Pro00049492). We employed a mixed-methods descriptive study design to evaluate form implementation. Quantitative results address all objectives, whereas qualitative results address only objective three. Chart review of form completion and HCP survey responses were used to assess implementation and feasibility of the form. No control group was followed. We noted whether alternative pre-existing transition forms were used when the study form was not used.
The study was designed with the intent of collecting data for quantitative analysis. Initially, open-ended questions were included on HCP surveys with the expectation that respondents would provide short responses that could be re-coded for purely quantitative reporting. However, open-ended survey responses proved unexpectedly rich (Denzin & Lincoln, Reference Denzin and Lincoln2005) and our choice to analyse these data qualitatively resulted in a mixed-methods approach. The project thus utilizes an emergent mixed-methods design, as described by Creswell and Plano Clark (Reference Creswell and Plano Clark2011), because mixed-methods analyses were not intended at the outset but rather driven by the unanticipated richness of the qualitative data.
In keeping with the criteria of rigour for qualitative methods (Lincoln & Guba, Reference Lincoln and Guba1985), we disclose the characteristics and methodological commitments of our research team. The principal investigator is a PhD nurse scientist whose expertise is broadly in quantitative methods, but who has led mixed-methods studies. Other authors are, broadly, health services researchers with interests in implementation science and expertise in the fields of emergency medicine, nursing, and sociology, and some have qualitative experience. The research paradigm informing the study is pragmatist (Denzin, Reference Denzin2010; Feilzer, Reference Feilzer2010). We have combined qualitative and quantitative tools to generate deeper understanding to fulfill our research objectives.
Setting and Participants
Implementation and data collection occurred from February to October 2015, with the goal of collecting 100 forms, and included a post-intervention survey of HCPs in all care settings (i.e., ED, LTC, EMS). One large urban teaching hospital ED (75,000 patients per year) was selected as the study ED. The 15 LTC facilities that reported the highest overall numbers of transitions to the participating ED in previous research were approached to participate in this study (Cummings et al., Reference Cummings, Reid, Estabrooks, Norton, Cummings and Rowe2012; Reid et al., Reference Reid, Cummings, Cooper, Abel, Bissell and Estabrooks2013). Of these, 11 (73%) agreed to participate. These 11 LTCs represent a variety of public, private, and non-profit organizations with 106–495 beds (median 180, interquartile range [IQR] 71). Forms were collected for emergency transitions of patients 65 years of age and older, resident in one of the LTCs and transitioned to the included hospital by EMS. At the time of the study, LTCs used paper and electronic documentation (sometimes sending copies to the ED), EMS used electronic charting printed at ED arrival, and ED staff used paper charts and forms.
Survey participants in the ED were registered nurses (RNs) and licensed practical nurses (LPNs). Survey participants at LTC sites included RNs, LPNs, administrative staff, managers, and directors of care. EMS survey participants were paramedics, emergency medical technicians, and supervisors.
Form Design and Use
Form design was led by researchers, clinicians, and health care administrators from settings including LTC facilities, the provincial health authority, one ED, and EMS. Information items on the form were derived from insights gained in the Older Persons’ Transitions in Care (OPTIC) study (Cummings et al., Reference Cummings, Reid, Estabrooks, Norton, Cummings and Rowe2012, Reference Cummings, McLane, Reid, Tate, Cooper and Rowe2020), and from a review of the literature (Cortes, Wexler, & Fitzpatrick, Reference Cortes, Wexler and Fitzpatrick2004; Cwinn et al., Reference Cwinn, Forster, Cwinn, Hebert, Calder and Stiell2009; Hustey & Palmer, Reference Hustey and Palmer2010; Jones, Dwyer, White, & Firman, Reference Jones, Dwyer, White and Firman1997; Kelly et al., Reference Kelly, Mahoney, Bonner and O’Malley2012; Kenneth, Bella, & Cinthya, Reference Kenneth, Bella and Cinthya2005; Madden, Garrett, & Busby-Whitehead, Reference Madden, Garrett and Busby-Whitehead1998; Sanders, Reference Sanders1997; Terrell et al., Reference Terrell, Brizendine, Bean, Giles, Davidson and Evers2005, Reference Terrell, Hustey, Hwang, Gerson, Wenger and Miller2009; Terrell & Miller, Reference Terrell and Miller2006; Zamora et al., Reference Zamora, McCall, Patel, Biese, Lamantia and Platts-Mills2012). See Figure 1 for a diagram of form components. The majority of the form (one and a half of two pages) was to be completed at the LTC. Items completed by the LTC included reasons for transition, medical history, principal diagnosis, practitioner name and contact details, allergies, medications, mental/behavioral/cognitive issues, alerts (e.g., fall risk), details on whether family and usual physician were notified of the transition, and records of the resident’s personal items. The form also directed LTC staff to attach supplementary documents to the form, such as personal directives, goals of care orders, and medication records.

Figure 1. Form section diagram
EMS personnel transporting the resident to the hospital signed off on whether another HCP transferred care of the resident to them, whether they received the resident’s personal items, and whether they consulted the transport physician. A photocopy of the form was sent with the resident to the ED. Nursing staff in the ED signed off on receipt of the resident and provided the name and contact information of the receiving HCP.
On sending the resident back to the originating LTC (if applicable) the discharge nurse at the ED marked whether there was a change in the resident’s condition or not (attaching explanatory documentation if a change had occurred), and provided their name and signature. Transport staff for the return trip then signed for the patient, and checked off whether next of kin had been notified of the transition, whether the LTC had been notified of the resident’s return, and whether (and which) personal items were returned with the resident.
Implementation
Research assistants (RAs) provided in-person training on the new form to night and day shift HCPs at study LTC sites and the ED. Training sessions lasted approximately 1 hour. Research assistants provided each HCP with a copy of the form, and gave a 10–15 minute oral presentation on the purpose of the form, sections to be completed, and the process for sending the form to the ED via EMS. Using fictional transition information, the RA then went through each data element on the form with the HCPs to clarify points of ambiguity and address their questions. During all training, RAs stressed that form completion should never delay urgent medical transitions and provision of care. LTC sites were provided with a paper copy of an instruction manual for using the form, and this guide was available electronically to ED and EMS HCPs. RAs trained ED nurses on the use of the form through presentations at morning rounds for each unit within the ED that receives seniors. Approximately 2 weeks prior to the project launch, EMS leaders provided a brief overview of the study and instructions about completing the form at the beginning of shift for all EMS staff. Repeat training was available upon site request. In two instances, educators contacted RAs with follow-up questions. No sites indicated a desire for additional training sessions.
Data Collection
Using the local Emergency Department Information System, RAs identified all transitions from participating LTCs to the participating ED by searching for patients whose addresses matched that of an LTC. Copies of completed forms were collected at the ED and upon resident return to the LTC. RAs also took note when an alternate transition form was used (i.e., various LTC developed forms, and one government-issued form). A post-intervention survey was administered to HCPs in person at participating sites, but not linked to specific transitions using the form. Respondents were asked to respond to two sets of questions, one for the most recent transition that they were involved in for which the form was used, and one for the most recent transition that they were involved in without the form. Each set of questions consisted of 13 ordinal scale questions. The majority of survey items asked about ease of accessing information required to care for the resident including: reason for transition, “code status”, baseline mental status, allergies, medical history, current medications, baseline mobility, contact information, laboratory test results/x-ray records, and transition information. Other items asked whether the respondent could access information needed to care for the resident within 2 minutes, whether documents listed as attached to transition records (e.g., goals of care) were in fact attached, and whether the availability of information allowed the respondent to provide more personalized care to the resident than would have been possible without this information.
In addition, four open-ended questions asked about what providers found most and least helpful in the form, as well as their experience using it, and elicited any other comments that they wished to make that were relevant to resident transitions. The ED/EMS version of the survey questionnaire appears as Appendix 1. Wording was modified slightly for the LTC version, to make the terminology used appropriate to that care setting. Only questionnaires from respondents who had seen the form used in practice are included in our analysis.
Analysis
Form utilization data were analysed by counting the number of forms used in the sample of transitions and calculating the proportion of forms completed at each setting (LTC, EMS, ED on receiving the resident, ED upon discharge, and EMS on the resident’s return trip). Two RAs independently determined whether each form section was complete and resolved discrepancies by consensus. We counted completion percentages for each information item (e.g., primary physician name). Information provided in the relevant space on the form counted as completion of the item.
Continuous data are reported as medians and IQR; dichotomous data are reported as counts and proportions. Wilcoxon signed rank tests were conducted for post-survey responses within settings (LTC, EMS, ED) to compare HCP perceptions of transitions using the form compared with transitions not using the form. The Wilcoxon signed rank test was chosen rather than a t test, because it is a non-parametric test appropriate for ordinal level and skewed data. Values of less than or equal to 0.05 were considered statistically significant. All quantitative data were analysed using SPSS (Version 24; Armonk, NY, United States).
Qualitative data were analysed through inductive content analysis (Elo & Kyngäs, Reference Elo and Kyngäs2008; Vaismoradi, Turunen, & Bondas, Reference Vaismoradi, Turunen and Bondas2013). HCP responses to open-ended questions were coded by a single RA, and coding decisions were discussed by the research team. We provide counts of survey question responses labeled with particular codes. Doing so provides the reader with a sense of how common a concern about the form or transition process was among respondents, and is more specific than using general terms such as “many” or “few” (Sandelowski, Reference Sandelowski2001). Like much pragmatically oriented research within the health sciences, emergency medicine (Choo, Garo, Ranney, Meisel, & Morrow, Reference Choo, Garo, Ranney, Meisel and Morrow2015; Cooper & Endacott, Reference Cooper and Endacott2007) and nursing, our qualitative methods are “descriptive” (Vaismoradi et al., Reference Vaismoradi, Turunen and Bondas2013) and “generic” (Caelli, Ray, & Mill, Reference Caelli, Ray and Mill2003; Kahlke, Reference Kahlke2014).
A descriptive approach to our qualitative data is appropriate because they were generated through written responses to standardized survey questions. Survey responses generally do not provide sufficient data for the purposes associated with the major qualitative traditions such as grounded theory or ethnographic methods (LaDonna, Taryn, & Lingard, Reference LaDonna, Taryn and Lingard2018). Despite these limitations, when interpreted alongside our quantitative results, our qualitative results strengthen our understanding of form use in practice. In keeping with the advice of LaDonna and colleagues on the limits of open-ended survey responses as qualitative data, we have treated our qualitative analysis as a supplement to our overall quantitative analysis (2018).
Results
Objective 1: Enumerate and Evaluate Form Use across Transitions
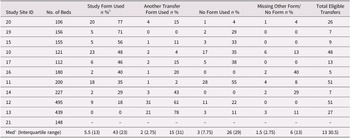
RAs identified 244 eligible transitions across 11 LTC facilities. Ninety forms were used in these transitions (37% of eligible transitions). Among sites, a median of 13 (IQR: 7, 48) eligible transitions occurred, and form use varied by site from 77 per cent to 0 per cent. The median uptake of forms among sites was 43 per cent (see Table 1 for uptake rates by site). One enrolled site had no eligible transitions during the study period. Sites that used the form in a low proportion of their transitions generally used a pre-existing transition form (see Figure 2 for form use comparisons). In 18 cases, the data collector could not access the resident’s chart to determine whether any transition form was used.
Table 1. Form uptake rates by site a

a Categories are mutually exclusive. If the study form was used and another transfer form was also used, we counted this transfer as using the study form. In 18 cases in which a nurse checked the patient chart for the data collector (e.g., on inpatient units), we know that the study form was not used, but do not know if another form was used.
b All percentages are calculated as n divided by total eligible transfers per site.
c This row excludes site 21 because this site had no eligible transfers, except in the “total eligible transfers” column, where 0 is a valid value.

Figure 2. Form use versus another form used Note: Facility bed numbers provided on horizontal axis.
Objective 2: Assess Form and Item Completion across Settings
In 16 of 90 cases (18%), one of the two pages of the form was missing (presumed lost). Of the remaining 74 forms, all (100%) were completed by LTC staff, whereas 19 (26%) included information completed by EMS and 5 (7%) contained information recorded by ED nurses. One case was identified for which the form was completed by all settings involved in the transition. In 12 of 90 cases (13.3%), the resident had died in hospital; therefore, the form was not returned to the LTC. In 6 of 90 cases (6.6%), transition information was provided by EMS or ED HCPs and returned to the LTC via the form.
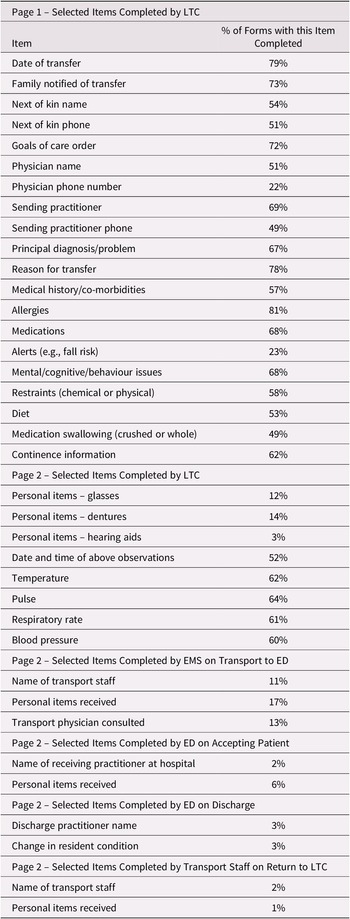
Completion of specific information items on the form was further examined (see Table 2). Item completion in LTC ranged from 79 per cent (reason for transition) to 0 per cent for several items (e.g., bariatric alerts, site of second peripheral venous line). Item completion by EMS on transport to hospital ranged from 18 per cent (whether the handover was provided to EMS) to 6 per cent (event number, which is an administrative tracking number for the transport). In the ED, item completion ranged from 6 per cent (receiving facility name) to 0 per cent (checkboxes for “alert” and “oriented” mental status). For EMS on the return trip, item completion ranged from 2 per cent (e.g., receiving transport staff) to 1 per cent (e.g., transport physician consulted; see Table 2).
Table 2. Selected form items and completion rates

Note. Items appear in the table in the order in which they appear on the form.
LTC = long-term care; EMS = emergency medical services; ED = emergency department.
LTC HCPs completed the principal diagnosis on 67 per cent of forms, mental/cognitive or behavioural issues on 68 per cent of the forms, and whether the resident’s family was notified of the transition on 73 per cent of the forms. Allergy information was marked as attached, or not applicable, on 81 per cent of forms. Goals of care documents (e.g., do not resuscitate) were marked attached on 72 per cent, and medication lists were attached (or the resident marked as having no medications) on 68 per cent. Whether the resident had dentures (specified as being with them, with family, or left at LTC) was documented by the LTC on 14 per cent of the forms, and glasses were documented on 12 per cent of the forms. Assistive devices were acknowledged as received by EMS, or not received, on 17 per cent of the forms and acknowledged by the ED on 6 per cent of the forms.
Objective 3: Examine HCPs Assessment of Form (Survey Results)
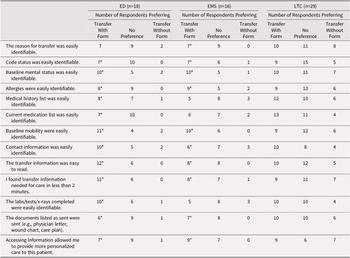
Overall, 103 LTC post-transition surveys were collected (87% response rate). Of the LTC respondents, 29 (28%) indicated that they had seen the form in practice and could answer questions about identifying/utilizing resident information during transitions using the form. ED nurses completed 72 post-surveys (77% response rate) of which 18 (25%) reported seeing the form in practice. EMS HCPs completed 91 post-surveys (86% response rate), of which 16 respondents (18%) had seen the form in practice. Post-survey results are presented in Table 3.
Table 3. Post-survey results

Note. *Results for this category for this setting are significant at the ≤ 0.05 level.
ED = emergency department; EMS = emergency medical service; LTC = long-term care.
In the ED, all but one of the differences between respondent ratings of ease of identifying/utilizing resident information where the form was used, compared to without the form being used, were statistically significant. The exception was a question about whether the reason for the transition was easily identified, for which form use did not impact responses. For all items, a majority of ED respondents ranked ease of identifying resident information better when the form was used than when the form was not used.
For the EMS survey, all differences in responses related to transitions that used the form and those that did not use the form were significant except for: current medication list, medical history and laboratory tests/x-rays. For all significant items, more respondents ranked transitions with the form higher than transitions without the form. Results for the LTC survey were nonsignificant.
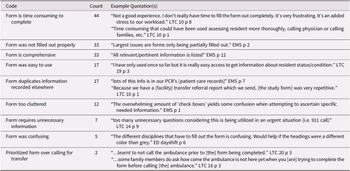
Open-Ended Survey Responses
Codes arising from HCP responses to open-ended questions are presented in Table 4. Overall, HCP responses showed a mix of views on the form. Issues of the time taken to complete the form were noted by 44 participants. As one HCP wrote, “…in an emergency situation where every minute counts [the form] is very time consuming [and] stressful to complete…” (LTC 16 p3). Some comments about the time taken to complete the form also noted that completing the form took time away from direct patient and family-centred care. “Time consuming [when time] could have been used assessing resident more thoroughly, calling physician or calling families, etc.” LTC 10 p1).
Table 4. Qualitative coding of open-ended responses

Note. Quotations are labeled with the setting the participant worked in (LTC, EMS or ED), followed by a site number, then p for “participant,” followed by a participant number.
LTC = long-term care; EMS = emergency medical service; ED = emergency department.
In addition, some responses showed evidence of frustration about the process of sharing a paper form among sites. An EMS respondent wrote “I have an issue signing [a] form that I have not filled … My [patient care record] should be the only documentation I need to sign. I found many errors in [the] form that had been filled out” (EMS p2). An LTC respondent noted “we are using the form but it is rarely (if ever) sent back to us. Hospitals are not following the process. - did not improve anything for us” and “from a management perspective: the form requires too much information from the sending site in comparison to what is provided to us on return.” (LTC 20 p4).
The open-ended responses also revealed an unintended consequence of the form: two LTC respondents noted that they prioritized form completion over arranging urgent transport. A third respondent’s comment (LTC 20 p6), about a resident “deteriorating” because of the time taken to complete the form, also suggests that completing the form was prioritized over care, despite RA instructions during training sessions.
Discussion
This study examined the use of a new communication form by HCPs caring for LTC residents being transitioned by EMS to the ED and back. The goal of the form was to improve consistency of documentation and thus continuity of care by reducing information gaps at each step of the transition.
Despite formal training of LTC, EMS, and ED HCPs by dedicated research staff, the form was only used in approximately two of every five transitions. This is markedly lower than a 73 per cent form uptake reported in an LTC to ED transition form study by Kelly et al. (Reference Kelly, Mahoney, Bonner and O’Malley2012), and below the 50 per cent uptake reported by Zafirau et al. (Reference Zafirau, Snyder, Hazelett, Bansal and McMahon2012); however, it is comparable with the 28 per cent uptake reported by Hustey and Palmer (Reference Hustey and Palmer2010) and the 32 per cent uptake reported by Terrell et al. (Reference Terrell, Brizendine, Bean, Giles, Davidson and Evers2005). Nursing documentation in LTC has been historically inadequate (Campbell, Stirling, & Cummings, Reference Campbell, Stirling and Cummings2017; Griffiths et al., Reference Griffiths, Morphet, Innes, Crawford and Williams2014; Morphet et al., Reference Morphet, Griffiths, Crawford, Crow, Williams and Innes2014; Zafirau et al., Reference Zafirau, Snyder, Hazelett, Bansal and McMahon2012) as has both ED documentation (Ayatollahi, Bath, & Goodacre, Reference Ayatollahi, Bath and Goodacre2013; Lorenzetti et al., Reference Lorenzetti, Quan, Lucyk, Cunningham, Hennessy and Jiang2018) and documentation on transition to acute care (Harl, Saucke, Greenberg, & Ingraham, Reference Harl, Saucke, Greenberg and Ingraham2017; Parashar, McLeod, & Melady, Reference Parashar, McLeod and Melady2018).
Open-ended comments suggest that the time needed to complete the form was a major factor limiting its uptake and completion. However, the form included information that LTC HCPs would have already included in transition documentation or that was indicated as necessary in emergency transitions (Cummings et al., Reference Cummings, McLane, Reid, Tate, Cooper and Rowe2020; Griffiths et al., Reference Griffiths, Morphet, Innes, Crawford and Williams2014), in a condensed checklist and “fill in the blank” format. It is unclear if complaints about the time taken to complete the form highlight a problem with the form itself, the implementation of the form, or potentially unrealistic documentation expectations in emergent situations. During urgent medical events, form completion may not be a priority in any setting. This finding is consistent with those of Keenan, Yakel, Tschannen, and Mandeville (Reference Keenan, Yakel, Tschannen, Mandeville and Hughes2008), who report widespread disdain for formal health record keeping.
Use of competing forms for transition documentation also likely detracted from maximal form uptake. The two sites with the lowest proportionate form use relied heavily on alternate forms (in 61% and 78% of their transitions). Low form uptake rates may also be explained by low LTC satisfaction with the form, insofar as LTCs were responsible for initiating use of the form and completing the largest section. There may also have been a sense that the form sought more detailed information than was necessary for a successful care transition, a finding consistent with those of McCloskey (Reference McCloskey2011). Poor form completion in EMS and the ED may demonstrate discomfort with sharing documentation across settings, driven by distrust of information provided by other HCPs. Reay et al. report issues of ED nurses’ trust in EMS handover information (Reay et al., Reference Reay, Norris, Nowell, Hayden, Yokom and Lang2020), while Tupper, Gray, Pearson, and Coburn (Reference Tupper, Gray, Pearson and Coburn2015) discuss distrust and differing expectations around communication among nursing facilities, EMS and the ED. In crowded EDs, transitions are also time sensitive. In our study ED, most nurses care for more than three patients in their area and must balance documentation against other acute patient care tasks, including maintaining capacity for the arrival of new patients.
Results similar to our findings have been found in studies of the impacts of surgical checklists (Mayer et al., Reference Mayer, Sevdalis, Rout, Caris, Russ and Mansell2016; Russ et al., Reference Russ, Rout, Caris, Mansell, Davies and Mayer2015), and some findings in that domain may be applicable to LTC to ED transitions. Although pilot sites for surgical checklists showed significant reductions in morbidity and mortality, the same levels of success were not sustained when the checklists were adopted more widely. Mayer et al. (Reference Mayer, Sevdalis, Rout, Caris, Russ and Mansell2016) found that surgical checklists may have been treated in a “tickbox” fashion and “largely seen as ‘completed’ by the operating room team when only 1 or 2 components of it have been completed.” If a tendency to view partial use of the form as completion of the form was also present in HCPs utilizing our form, this could have contributed to particular information items being inadequately completed.
Russ et al. (Reference Russ, Rout, Caris, Mansell, Davies and Mayer2015) also found that checklists were frequently completed only in part because clinical teams faced time pressures and were uncertain when aspects of the checklist should be completed. Time pressures were similarly noted by our respondents, and uncertainty about when our form was meant to be completed may be inferred from respondent comments about decisions to fill out the form prior to calling 911.
Russ et al. (Reference Russ, Rout, Caris, Mansell, Davies and Mayer2015) further found that certain factors lead to greater surgical checklist completion; namely, presence of all team members and having the senior surgeon lead checklist completion. In LTC to ED transitions, however, unlike with surgeries, there is no point when all HCPs involved are physically present together, and there is often no senior leader with oversight of the entire transition. Physicians are infrequently present in the LTC at the time of patient transfer to the ED. The absence of these factors in LTC to ED transitions may nonetheless help explain our findings of poor form completion.
Among the qualitative results, the fact that form use was prioritized over calling 911, by at least two HCPs, was perhaps the most surprising study finding. We were further surprised that any HCPs were willing to disclose this practice and wonder if more respondents may have used the form in this way without reporting it. This result provides an example of how a seemingly benign bureaucratic change (an attempt to replace multiple transition forms with a single improved form) may have had the opposite effect of what was intended in some cases (worsening emergency care of LTC residents, rather than improving it). This result also illustrates the importance of examining unintended consequences of efforts intended to improve health services (Goodman et al., Reference Goodman, Ogrinc, Davies, Baker, Barnsteiner and Foster2016). Finally, this result shows the utility of qualitative data, which allowed in this case for detection of an unintended outcome that the researchers did not anticipate at the outset of the study and would not have become aware of through quantitative data alone.
Given our qualitative findings, we can consider our results in light of Kitson, Athlin, and Conroy’s critiques of depersonalized and disaggregated, task-based, health care (Kitson et al. Reference Kitson, Muntlin Athlin and Conroy2014). The form was composed of discrete information on care needs, resident information, and health conditions, rather than comprising an integrated care plan or promoting a focus on the resident as a unique individual undergoing a dangerous series of transitions in care. Problematic use of the form illustrates what Kitson and colleagues call an “inherent systemic tension between the task and time approach to ‘getting the job done’ and the need for someone (on the patient’s behalf) to be integrating and personalizing the experience through thinking about the whole experience and linking the activities into a series of meaningful encounters” (Kitson et al., Reference Kitson, Muntlin Athlin and Conroy2014). The form alone did not support an integrated care experience for the resident. Instead, HCPs viewed the form through a lens of what it required of them and how their care setting benefited from it. This is exemplified by concerns among LTC staff that they were doing more work than HCPs in other settings, and EMS concerns about reliability of LTC-provided data.
Two positive results of the form implementation were a modest increase in documentation of personal items (e.g., glasses, dentures), suggesting that including specific space to record these items in documentation is worthwhile, and higher ranking of HCP ability to identify/utilize information in transitions using the form, compared with usual practice, by EMS and ED HCPs.
Recommendations
In the future, form designers should consider feedback to make documentation take as little time as possible. Time to fill out the form could be reduced by pre-filling information that rarely changes or using electronic systems to automatically populate forms. Carson et al. (Reference Carson, Gottheil, Gob and Lawson2017) reported success in improving transition documentation by implementing printable electronic records at LTCs, thus “minimizing extra work”. Shared electronic health records may also be beneficial in consolidating patient information across settings. Although the paper-based version of the form may be cumbersome, the content has been co-developed by representatives of the ED, EMS, and LTCs, and perhaps is best applied in more sophisticated electronic environments.
Furthermore, we would suggest that future efforts in LTC to ED transitions should address trust and relationships among HCPs working in distinct settings. Improving collaboration between ED and LTC settings has been previously identified as critical for addressing the insufficiencies of introducing a standardized transition form alone (Campbell et al., Reference Campbell, Stirling and Cummings2017; Cwinn et al., Reference Cwinn, Forster, Cwinn, Hebert, Calder and Stiell2009).
Finally, informed by Kitson et al.’s (Reference Kitson, Muntlin Athlin and Conroy2014) critique of task-based and depersonalized care, it seems to us that bureaucratic interventions of the kind that we studied may easily lead to perverse outcomes if not carefully implemented. We therefore recommend that future communication forms be implemented as part of broader transition improvement programs (with robust evaluation including qualitative methods) rather than as stand-alone interventions. Implementing formal care coordinator roles, with responsibility for personalizing resident care and bridging communication among all HCPs across transitions settings as part of such programs may help to guard against depersonalized care while reducing the workload of HCPs within each setting.
Limitations
The overall sample of transitions in this study was small, and related to only one ED. Surveys relied on convenience samples, raising concerns that our sample of respondents differs in important ways from the general population of ED, EMS, and LTC HCPs. High response rates among all respondent groups mitigate this concern.
Conclusion and Implications
This study demonstrated low form uptake, incomplete documentation, and potentially harmful unintended consequences of the form. We recommend that future transition communication forms be part of broader transition improvement programs that support personalized care while addressing trust among HCPs working in different settings. Moreover, it is likely that electronic health innovations such as automatic transfer of relatively static demographic and goals of care details, and sharing of health information across electronic systems, may address communication barriers without the need for paper forms.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/S0714980821000039.