On March 11, 2020, the World Health Organization (WHO) classified coronavirus disease 2019 (COVID-19) as a pandemic, as the levels of spread and severity of the disease increased rapidly worldwide. 1 Nonpharmaceutical interventions are necessary to decrease the spread of the virus in community settings. These interventions include face mask-wearing, physical distancing, and hand hygiene.
Face mask use in health-care facilities is widely accepted, with several studies now comparing the efficacy of various types of medical masks for the prevention of infection transmission. Reference MacIntyre and Chughtai2–Reference MacIntyre, Wang and Rahman6 However, even amid the pandemic, with many states and municipalities mandating face mask use in enclosed community settings such as offices and schools, there has been no definitive answer on the efficacy of mask-wearing in community settings. In fact, opinions and policies vary greatly worldwide. Governments of various countries and the Centers for Disease Control and Prevention and WHO have disagreed on masking guidelines and changed views throughout the course of the pandemic. Reference Yan7–15
Under the threat of a relentless pandemic that could result in many more deaths across the globe, it is imperative that infection prevention and control interventions are based on current evidence. Therefore, this review aimed to generate data to support evidence-based public health policy development regarding mask-wearing in community settings. As there are few data examining the effectiveness of mask-wearing in the community for COVID-19, this rapid review examined the transmission of respiratory infections in general. It includes randomized controlled trials and summarizes the efficacy of mask-wearing on the transmission of respiratory infections in the community setting.
Methods
Data Sources and Searches
This review followed the methods outlined in the McMaster Rapid Review Guidebook. Reference Dobbins16 The original search was conducted by means of PubMed from May 20-26, 2020. The search was then expanded in the following 2 weeks (end date, June 10, 2020) to include Google Scholar, Scopus, Health Evidence, and medRxiv (search terms in Appendix Table 1). The search was limited to English language articles. In addition, all relevant systematic reviews arising from the search were reviewed for additional primary literature matching the search criteria. Reference MacIntyre and Chughtai2,Reference Chu, Akl and Duda17–Reference Brienen, Timen and Wallinga29
Study Selection
Article titles were parsed for relevance in terms of study topic and setting. Relevant articles included studies focused on the efficacy of mask-wearing to reduce the spread of respiratory infections in community settings. Respiratory infections included in the analysis were any infection spread by aerosol or droplet, including but not limited to influenza A or B, rhinoviruses, coronaviruses, picornaviruses, enteroviruses, adenoviruses, respiratory syncytial virus, human metapneumovirus, and parainfluenza viruses.
Full texts of the articles deemed relevant were reviewed and reduced by study type. This rapid review focused solely on randomized controlled trials reporting quantitative data. Excluded were studies relating to respiratory virus transmission in health-care settings and nonrandomized controlled trials. Additional inclusion criteria included English language articles conducted with participants of any age in a community setting that measured influenza-like illness (ILI) symptoms or laboratory-confirmed respiratory viruses as a study outcome. A comprehensive list of inclusion and exclusion criteria can be found in Appendix Table 2. The selected articles that met all inclusion criteria were confirmed by a second investigator and further examined for duplication; duplicate studies were removed.
Data Extraction and Quality Assessment
Two investigators extracted study data: title, author, year of study, year of publication, study design, methods, participants, number of participants, primary outcome, measurement of outcome, other outcomes, type of mask, comparator, results of control, results of interventions, whether the paper reported a significant difference according to their statistical standards, and papers’ self-identified strengths and limitations. After extraction by both investigators, data were compared to ensure accuracy and completeness. To establish consensus on the data extracted between the 2 investigators, any discrepancies were reviewed by the senior investigator.
Critical appraisal of each study was performed using the Cochrane Risk of Bias Tool Reference Sterne, Savović and Page30 by means of Covidence software (Melbourne, Australia). This assessment evaluated risk of bias in the following areas: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting, and other potential sources of bias. The risk of bias for each aspect of the study was rated as high, low, or unclear by 2 investigators, and the individual assessment results were compared; any discrepancies were discussed until consensus was met. Following consensus evaluation, the reviewers gave each article an overall risk-of-bias rating. If an article had a high risk-of-bias rating in ≥2 categories, it was considered to have an overall high risk of bias. If an article had a high risk-of-bias rating in 1 category and ≤2 unclear ratings, it was considered to have an overall medium risk of bias. Finally, if an article had no high risk-of-bias ratings and ≤2 unclear ratings, it was considered to have an overall low risk of bias (Appendix Tables 3 and 4).
Data Synthesis and Analysis
This analysis used the META package in STATA to construct forest plots for all the studies, examining masking data alone, enhanced hand hygiene alone and a combination of masking and enhanced hand hygiene, to compare against a control. Reference Anzures-Cabrera and Higgins31 Only quantitative data on rates of ILI and laboratory-confirmed respiratory infection from included publications were analyzed in forest plots. A fixed effects model was first used to calculate the individual and pooled risk ratios (RR). The level of heterogeneity was then calculated using the I2 statistic. Reference Higgins and Thompson32 Forest plots reporting substantial to considerable heterogeneity based on the following I2 index (low heterogeneity [I2 = 0-40%], moderate heterogeneity [I2 = 30-50%], substantial heterogeneity [I2 = 50-90%], and considerable heterogeneity [I2 = 75-100%]) were re-calculated using the Dersimonian and Laird random effects model. Reference DerSimonian and Laird33 Publication bias was assessed using contour-enhanced funnel plots and the Egger’s test. Two-sided tests were used with all P-values ≤ 0.05 considered statistically significant. All analyses were conducted using STATA 16 (StataCorp LLC, College Station, TX).
Results
Literature Search
The database search yielded 37,366 titles. After removing duplicate articles and reviewing titles and abstracts, 56 full texts met initial inclusion criteria. Narrowing to randomized controlled trials left 11 eligible articles that were included in this rapid review (Figure 1).

Figure 1. Literature search and selection.
Eleven studies were identified as randomized controlled trials of face mask use in the community, taking place between 2006 and 2015 (Table 1). In total, there were 9140 participants across all intervention groups, and 6918 participants across all control groups. Studies were conducted across the United States, Australia, China, Thailand, Germany, and France. Two studies were conducted in university residence halls, 2 during Hajj pilgrimages, and 7 in households. Nine studies collected data on self-reported ILI symptoms, and 10 studies used laboratory tests to confirm respiratory infection. Seven studies reported multiple interventions, including enhanced hand hygiene, education, and masking or a combination. All studies used surgical masks for the masking intervention.
Table 1. Randomized controlled trials measuring the effects of mask-wearing on the spread of respiratory viruses in community settings
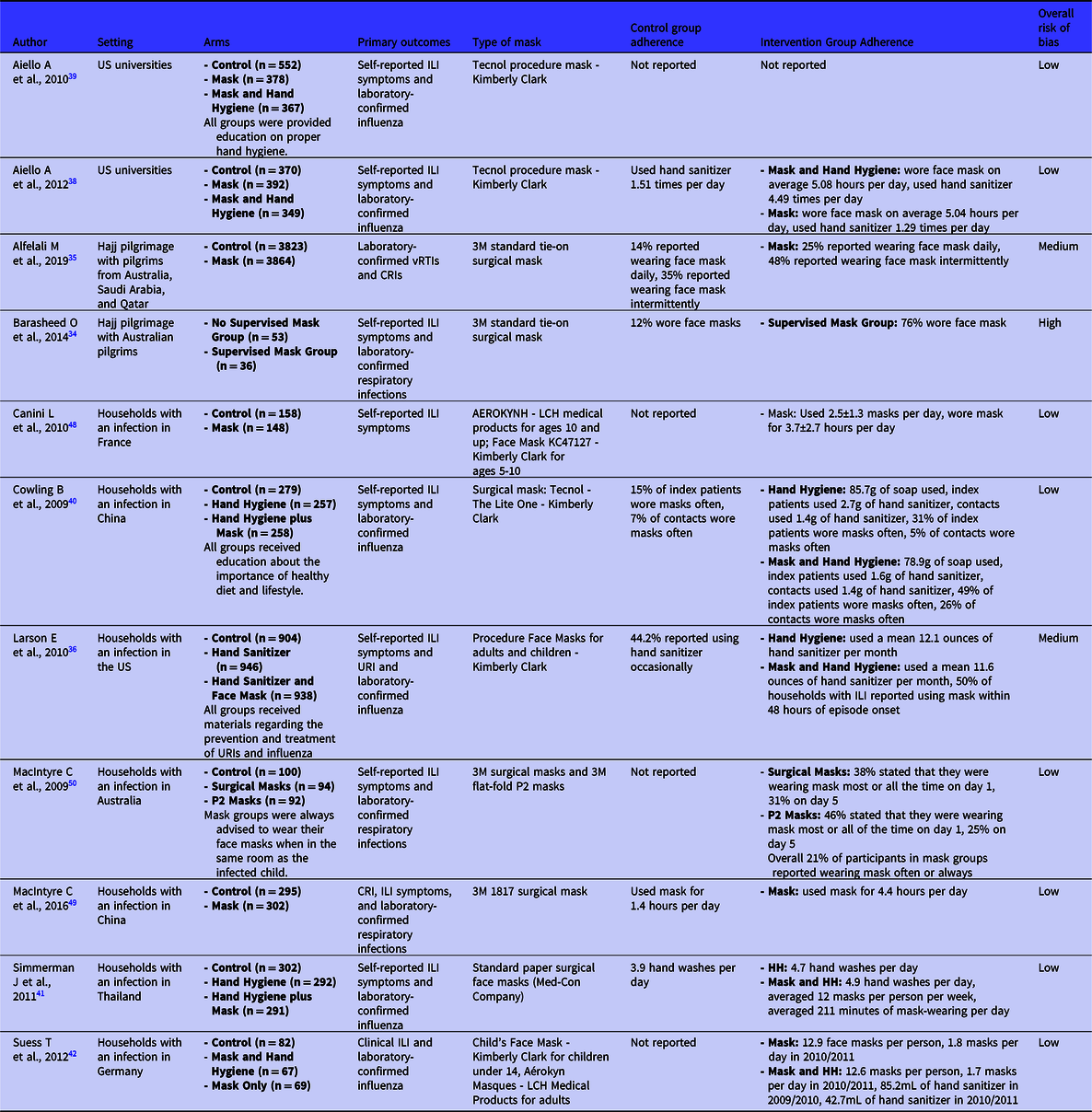
Abbreviations: HH, hand hygiene; vRTI, viral respiratory tract infection; CRI, clinical respiratory infection; URI, upper-respiratory infection.
Note: Risk of bias based on Cochrane Risk of Bias tool Reference Sterne, Savović and Page30
The overall risk of bias for the studies was generally low-to-medium. One study was identified, Barasheed et al., Reference Barasheed, Almasri and Badahdah34 that rated high for potential risk of bias based on the criteria, due to small sample size and demographic differences between intervention groups. Alfelali et al. Reference Alfelali, Haworth and Barasheed35 and Larson et al. Reference Larson, Ferng and Wong-McLoughlin36 both received an overall medium rank for risk of bias due to differences between intervention groups (Appendix Table 4).
Bias Testing
On the contour enhanced funnel plot (Appendix Figure 1), the measure of the study effect size (log risk) against the variance (standard error) was relatively symmetrical showing no signs of publication bias. The Egger’s regression test of asymmetry was not statistically significant (P = 0.54), also indicative that publication bias is absent.
Meta-analysis
Among the 7 studies evaluating mask-wearing alone that included ILI symptoms as an outcome, 14.5% (206/1419) of participants in the mask groups versus 19.5% (314/1610) of those in the control groups showed ILI symptoms, and masking was associated with decreased risk of ILI symptoms (RR, 0.83; 95% confidence interval [CI], 0.71 to 0.96) (Figure 2). There was no heterogeneity (I2 0.00%; H2 1.00). Two of the 7 studies found results that favored the control group (weight 9.15; RR, 1.02; 95% CI, 0.61 to 1.71; weight, 6.64; RR, 1.26; 95% CI, 0.69 to 2.31). In the other 5 studies, comprising 84.21% of the weight, masking was associated with reduced risk of ILI symptoms.

Figure 2. Forest plot of estimations of the association between face mask use and ILI symptoms. ILI+ = showed ILI symptoms; ILI− = did not show ILI symptoms.
Across the 7 studies evaluating mask-wearing alone that included laboratory-confirmed respiratory infection as an outcome, 3.51% (182/5188) of participants in mask groups versus 3.22% (172/5343) of those in control groups had a laboratory-confirmed respiratory infection. There was no statistically significant association between masking and risk of infection (RR, 1.04; 95% CI, 0.60 to 1.80) (Figure 3). In contrast to ILI symptoms, these studies showed a noteworthy effect of heterogeneity (I2, 56.14%; H2, 2.28). Three of the 7 studies found masking associated with reduced risk of illness. The other 4 studies found masking was associated with increased risk of illness, comprising 58.98% of the total weight.
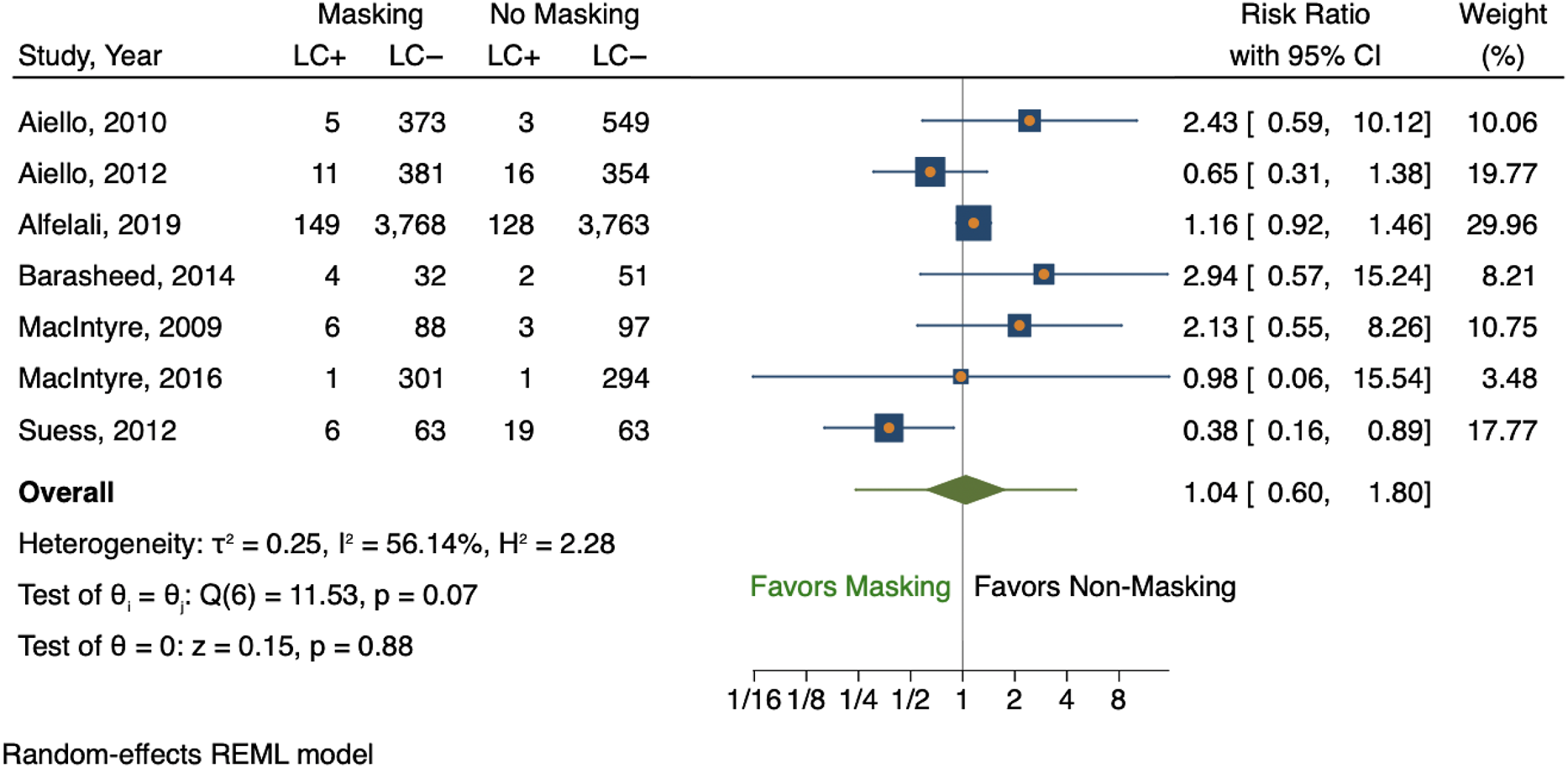
Figure 3. Forest plot of estimations of the association between face mask use and laboratory-confirmed respiratory infection. LC+ = laboratory-confirmed respiratory infection; LC− = no laboratory-confirmed respiratory infection.
In the 5 studies that also examined the effects of hand hygiene, masking combined with elevated hand hygiene was associated with a lower risk of ILI symptoms (RR, 0.88; 95% CI, 0.51 to 1.51) (Appendix Figure 2). These 5 studies showed a larger effect of heterogeneity (I2, 81.55%; H2, 5.42). Only 1 of the studies showed results that favored the control group (weight, 24.78; RR, 2.04; 95% CI, 1.31 to 3.17), while the other 4 studies associated masking and elevated hand hygiene with a reduced risk of ILI symptoms.
Last, in the 6 studies where it was examined, masking combined with improved hand hygiene was associated with a decreased risk of laboratory-confirmed respiratory infection (Appendix Figure 3). This was the strongest association among all the comparisons (RR, 0.79; 95% CI, 0.52 to 1.18). These 6 studies showed modest heterogeneity (I2, 41.87%; H2, 1.72). Only 1 of the studies showed results that favored the control group (weight, 35.93; RR, 1.18; 95% CI, 0.86 to 1.62), and another study found no difference in infections between the groups (weight, 4.67; RR, 1.00; 95% CI, 0.17 to 5.97). The other 4 studies, making up 59.40% of the total weight, favored masking and elevated hand hygiene as associated with a reduced risk of laboratory-confirmed respiratory infection.
Discussion
This rapid review summarizes the evidence regarding the efficacy of face masks for reducing respiratory illness in the community setting—a critical question given the ongoing COVID-19 pandemic. The evidence derived from randomized controlled trials shows that masking in a community setting reduces self-reported ILI symptoms by 17%. However, it found limited evidence to support the same association between masking and transmission of laboratory-confirmed respiratory infections. On the other hand, masking combined with enhanced hand hygiene was associated with significantly reduced transmission both in terms of ILI (12% reduction) and laboratory-confirmed respiratory infection (21% reduction).
Surprisingly, the results of the analysis of the effect of face masks alone for reducing laboratory confirmed-respiratory were inconsistent with those for the analysis of reduction of ILI symptoms. One possible explanation for this could be bias and variation in self-reporting. ILI symptoms were measured by participant reports of qualifying conditions, such as cough, sore throat, chills, fever, headaches, body aches, etc., although exact definitions differed. Some studies used the Centers for Disease Control and Prevention (CDC) definition of ILI, which is a “fever (temperature of 100°F [37.8°C] or greater) and a cough and/or a sore throat without a known cause other than influenza,” 37 while other studies simply required any listed symptoms to be noted by participants. Not only was reporting inconsistent across studies and participants, but certain symptoms could also have been due to allergies or other conditions beyond viral infection, ultimately skewing the ILI measurements. Multiple included papers addressed self-reporting issues in their limitations, stating specific problems with subjects under-reporting symptoms, Reference Larson, Ferng and Wong-McLoughlin36 reporting what they thought was expected, Reference Aiello, Coulborn and Aragon20,Reference Aiello, Perez and Coulborn38,Reference Aiello, Murray and Perez39 and reporting ILI symptoms that were likely not due to influenza infection. Reference Aiello, Murray and Perez39 Additionally, it is important to note that because only a subset of all upper respiratory infection-causing viruses were included in the analyses, ILI symptoms may also have resulted from viruses that were not included in laboratory analyses. For example, 3 of the 7 studies reporting laboratory confirmed infection rates in the face mask-alone category tested only for influenza.
Furthermore, discrepancies also exist between the results of the analysis of face masks alone versus face masks in combination with enhanced hand hygiene, which may be due to viral transmissibility. In 5 of the 6 studies included in the analysis of the effects of face masks with advanced hand hygiene, Reference Aiello, Perez and Coulborn38–Reference Suess, Remschmidt and Schink42 influenza A and B were the only respiratory viruses tested for. According to a 2021 review by Leung evaluating the transmissibility of respiratory viruses, Reference Leung43 infectious influenza viral particles have been recovered on surfaces suggesting possible roles for direct and indirect surface transmission of the influenza virus. Thus, hand hygiene may play a larger role in reducing transmission of influenza viruses—as was indicated in the studies analyzed here—than in other respiratory viruses that do not appear to use direct and/or indirect contact as a major mode of transmission, such as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Reference Mondelli, Colaneri and Seminari44 Future studies are needed to evaluate the roles of mask wearing versus hand hygiene in a wider range of respiratory viruses.
Overall, the findings were similar to other systematic reviews that have examined the benefit of masking in both health-care and community settings Reference MacIntyre and Chughtai2,Reference Chu, Akl and Duda17,Reference Bin-Reza, Lopez Chavarrias and Nicoll18 with some important differences. Bin-Reza et al. Reference Bin-Reza, Lopez Chavarrias and Nicoll18 found a limited evidence base to support the use of masks in health-care or community settings but concluded that mask use is best undertaken as a package of personal protective measures, including good hand hygiene. The community randomized controlled trials included in the 2015 review by MacIntyre and Chughtai Reference MacIntyre and Chughtai2 suggested that face masks provide protection against respiratory infection in various community settings, although this protection is subject to adherence. Chu et al. Reference Chu, Akl and Duda17 also reported a lack of robust data but suggested that face masks were protective for people in the community who had been exposed to infection. Another rapid review relevant to COVID-19 found that data on the effectiveness of masking in community settings for preventing infections associated with coronaviruses were limited but suggest possible reduced risk for SARS-1 transmission associated with masking. Reference Chou, Dana and Jungbauer45 Adding to this evidence, a cohort study conducted in Beijing, China during the pandemic produced results showing that face mask use by a COVID-19 positive patient before symptom development was 79% effective in reducing transmission in the household, while face mask use after the development of symptoms was not significantly effective. Reference Wang, Tian and Zhang46 In contrast to the prior systematic reviews, this review was limited to randomized controlled trials specific to community settings, providing us with the highest quality evidence from which to draw conclusions specific to the community setting.
A limitation of this analysis is that many studies reported adherence issues with mask-wearing or difficulty measuring and reporting adherence. Self-report was used as a measurement tool in 8 of 11 studies, and there was great variability in how adherence was measured among the studies, ranging from daily self-reported data to measurement of the amount of intervention material remaining at the conclusion of the study. As a result, it was difficult to set a uniform scale for adherence to assess its impact on measured outcomes. Lack of consistency related to adherence may influence individual study results and, thereby, the results of this analysis. With many studies reporting low mask-wearing adherence among study participants, the inability to consider these data may have resulted in an underestimation of the effects of the interventions in this analysis and also may explain why this review did not find a reduction with masking and laboratory-confirmed respiratory infection. However, the prevalence of adherence issues among the studies may provide practical insight for public health officials when considering mask-wearing mandates within a community setting. Looking at the greatest public health successes over the past few decades (eg, tobacco control, seatbelt use, motor vehicle safety, childhood lead poisoning, fluoridation, immunization), few can be attributed to changing personal or individual behavior; instead, these successes are directly attributed to laws or mandates. 47
When discussing limitations, it is also important to consider the additional limitations of the individual studies included in this rapid review. Foremost, there were different definitions of ILI within included studies, which made it difficult to make comparisons. In addition to varying definitions of ILI and the adherence issues discussed previously, several studies had small sample sizes and, therefore, were underpowered, limiting detection of small differences between intervention arms. Reference Barasheed, Almasri and Badahdah34,Reference Larson, Ferng and Wong-McLoughlin36,Reference Aiello, Murray and Perez39,Reference Suess, Remschmidt and Schink42,Reference Canini, Andréoletti and Ferrari48,Reference MacIntyre, Zhang and Chughtai49 Self-reported data, as discussed above, also present a potential source of bias. Moreover, in 2 studies, there was potential for infection in situations where masking was not required for the masking group—outside of the residence halls in Aiello et al. Reference Aiello, Perez and Coulborn38 and at dinner time in MacIntyre et al. Reference MacIntyre, Zhang and Chughtai49 In the Cowling et al. Reference Cowling, Chan and Fang40 study, there was potential bias due to the inclusion of symptomatic patients, which may have resulted in higher viral shedding, unavoidable delay between symptom onset and application of intervention, and households with existing immunity. Last, in multiple studies there were widespread community hygiene efforts in place that may have influenced control group practices. Reference Alfelali, Haworth and Barasheed35,Reference Larson, Ferng and Wong-McLoughlin36,Reference Simmerman, Suntarattiwong and Levy41
Conclusions
In conclusion, this analysis found that masking in the community setting may be an effective way to slow the spread of respiratory illnesses. Future research should examine the impact of universal masking by the public on SARS-CoV-2 transmission. It should also address how best to maintain and measure adherence in a community or household setting as well as how to eliminate bias from reporting of ILI symptoms.
To reduce transmission of COVID-19, masking in community settings in combination with a sustained emphasis on adherence with hand hygiene best practices is recommended. The benefits of masking may be lost if hand hygiene is de-emphasized in community settings.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2021.369
Funding statement
M.B. was supported by a National Library of Medicine (NLM) training grant to the Computation and Informatics in Biology and Medicine Training Program (5T15LM007359). Research reported in this publication was also supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (DP2AI144244). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict(s) of interest
None.






