In December of 2019, a highly transmissible and devastating disease known as the coronavirus disease 2019 (COVID-19) originated from Wuhan, China, leading to an epidemic of severe acute respiratory illnesses that rapidly spread to other countries across the globe. COVID-19, which is caused by a pathogen known as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is currently a leading cause of death in many countries and is responsible for more than 430 million cases, and almost 6 million mortalities in over 114 countries. 1–3 Although COVID-19 has placed massive socio-psychological, health, and economic burdens including deaths of countless lives, susceptibility to the pandemic’s detrimental effects has disproportionally fallen on vulnerable populations with social-economic disadvantages. Several socio-contextual risk factors, eg, poverty, unemployment, food insecurity, lack of health-care access, insecure housing, racial segregation, health insurance, etc. could have considerable negative impacts on the current public health crisis as well as COVID-19 outcomes. Moreover, underlying health inequalities and co-morbid health conditions, eg, asthma, obesity, diabetes, etc., profoundly increase susceptibility to COVID-19 infections and deaths. Reference Wang, Li and Lu4,Reference Smith5
Accordingly, the World Health Organization describes social determinants of health (SDoH) as encompassing “the conditions of where a person is born, where they grow up, where they live, where they work, and where they age.” 6 Based on the Healthy People 2030’s taxonomy, SDoH is classified into 5 major domains: Economic Stability, Education, Neighborhood and Built Environment, Health and Healthcare Access, and Social and Community Context. 7,8 There is scientific consensus that SDoH indicators, eg, available housing, social distancing, good hygiene, remote employment, food security, health access, etc., can mitigate the prevalence and severity associated with COVID-19 outcomes, Reference Paul, Arif and Pokhrel9–Reference Cyrus, Clarke and Hadley11 thereby significantly reducing the strain on the overburdened health-care systems posed by the pandemic. The impacts from COVID-19 are intricate and multi-layered; therefore, more studies are needed to explore the impacts of SDoH on COVID-19 and vice versa. Also, the B.1.617 (Delta) and more recently the B.1.1.529 (Omicron) variants of the SARS-CoV-2 have generated great concern due to their rapid spread and potential to reduce therapeutic effectiveness for treatments and vaccines. Accordingly, the objectives of this literature review were to (1) examine literature focused on SDoH and COVID-19 outcomes among minority communities; and (2) identify SDoH disparities associated with COVID-19 outcomes. The integration of SDoH indicators into policies, surveillance, and intervention strategies could mitigate morbidities and mortalities associated with COVID-19 and future disease outbreaks/pandemics.
Methods
Search Strategy
The review of literature incorporated studies that were identified from 2 databases (PubMed and Social Science Research Network [SSRN] published between October 2019 and October 2021). We adopted October 2019 as our timeline for study selection because this represented when COVID-19 first emerged from China. Our search terms were combined and used based on the following thesaurus and keywords: “Social Determinants of Health and COVID-19”, “Effects of Social Determinants of Health on COVID-19 Infection”, “Race and/or Ethnicity and COVID-19/SARS-CoV-2”, “Education and/or Income Level and COVID-19”, “Crime rates and COVID-19”, “Violent Crime and COVID-19”, “Transportation and Health Disparities, COVID-19”, and “Housing and/or Neighborhood and Health Disparities, COVID-19.”
Eligibility Criteria
Studies were included for review if they met the following eligibility criteria: (1) examined SDoH indicators (ie, race/ethnicity, poverty, median income level, housing density, housing insecurity, health-care access, occupation, etc.) and COVID-19 outcomes (ie, infectivity, hospitalization, and death rates among the populations studied), (2) were conducted in the United States, and (3) cross-sectional and cohort studies which were available in English language. Reviews and editorials were also included in our literature review. Studies were excluded if they neither focused on the COVID-19 pandemic nor addressed 1 or more of the 5 SDoH domains defined by the Healthy People 2030’s taxonomy.
Study Selection, Data Extraction, and Analysis
Our initial electronic database search generated articles whose titles/abstracts were collectively screened by 2 reviewers (B.W. and W.B.) using the eligibility criteria and which yielded 39 studies. Following the full-text screening, 11 studies were eliminated because they did not meet the inclusion criteria. Overall, a total of 28 studies were selected for the data extraction and analysis conducted by BW and WB see Figure 1). A third reviewer (O.O.) verified the study selection and data extraction process. The following data were extracted: title, lead author, publication year, study purpose, study design, sample size, sampling technique, participants’ demographics, and SDoH predictors. Extracted data were collated and stored on an excel spreadsheet coding matrix.
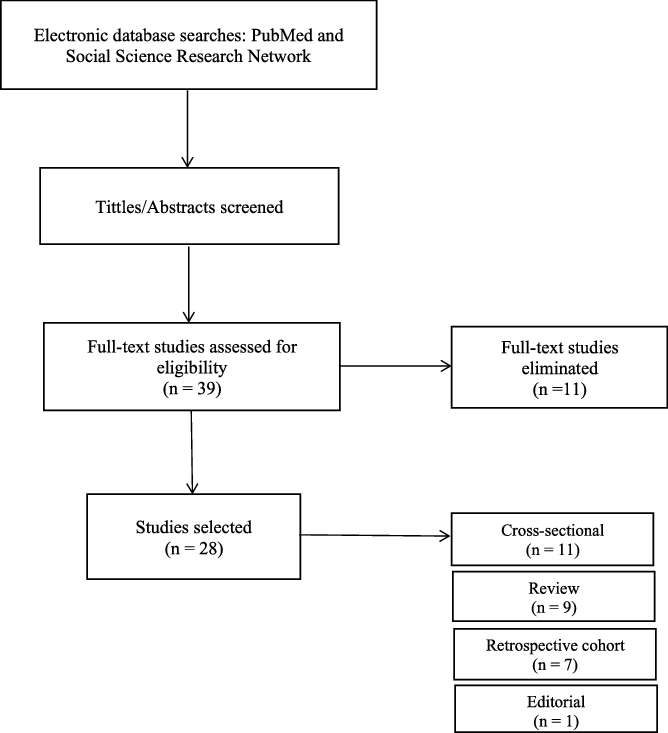
Figure 1. Literature review flow diagram.
Results
A total of 28 studies met the inclusion criteria for our review. Study characteristics and general information on articles selected for review are shown in Table 1. In this article, we also described 5 domains that focused on the SDoH detrimental factors exacerbating the rapid spread of COVID-19 cases and deaths. Specifically, extracted data describing SDoH characteristics from our literature review findings were categorized into the 5 domains from the Healthy People 2030’s SDoH taxonomy: (1) Economic Stability, (2) Education, (3) Neighborhood and Built Environment, (4) Health and Healthcare Access, and (5) Social and Community Context (see Table 2). Overall, COVID-19 positive cases and/or mortality were found to be impacted by SDoH indicators such as race/ethnicity, poverty, median income level, housing density, housing insecurity, health-care access, occupation, transportation/commuting patterns, education, air quality, food insecurity, old age, etc.
Table 1. Summary table representing the characteristics of selected studies

Table 2. Components of our SDoH classification

Economic Stability
Employment
The US Bureau of Labor Statistics reported that only 19.7% of African Americans were able to work from home in contrast to 29.4% of White employees who worked remotely during the pandemic. Reference Shah, Sachdeva and Dodiuk-Gad12 Concurrently, minorities were more predisposed to working low-wage positions (eg, cleaners, grocery workers, delivery truck drivers) in the service industry and essential work settings (eg, grocery stores, transportation, health-care facility) and more likely to rely on abbreviated train and bus schedules for transportation, thereby increasing susceptibility to COVID-19 infectivity and death rates. Reference Vasquez Reyes13,Reference Rozenfeld, Beam and Maier14 In addition, some low-wage workers were denied paid sick leave thus increasing the likelihood of nonadherence to quarantine measures when exposed and/or sick. Reference Vasquez Reyes13 Moreover, unemployment and residence in a rural county were significantly associated with COVID-19 mortality (unadjusted relative risk [RR] = 1.868; Bayesian credible interval [CrI] = 1.171, 2.127) in another study. Reference Paul, Arif and Pokhrel9
Poverty
Data from the US population census depicted that median income for Black ($41,361) and Hispanic ($51,450) households was among the lowest when compared with other races. 15 Likewise, the most potentially at-risk counties in the United States with a greater percentile of the Centers for Disease Control and Prevention’s (CDC’s) Social Vulnerability Index (SVI) had higher incident cases (RR = 1.05; 95% prediction interval [PI]: 0.98, 1.12) and death rates (RR = 1.08; 95% PI: 1.00,1.16) compared with those counties with a lower percentile of SVI. Reference Neelon, Mutiso and Mueller16 Many American Indian communities lived in multigenerational households that impacted physical distancing and other inequalities measures. Tribal geographic regions also recorded higher percentages of poverty and unemployment, as well as experienced lower levels of educational status and per capita income compared to the national averages. Reference Hathaway17,Reference Kakol, Upson and Sood18 Some American Indian communities experienced poor running water, crowded living conditions, and lack of access to proper health care. Reference Hathaway17,Reference Kakol, Upson and Sood18 Moreover, the pandemic negatively impacted immigrant and farming populations as Fielding-Miller et al. found that COVID-19 mortality risk to be significantly higher for non-urban farmworkers, and those living below the national poverty line (5.79 and 4.41 more deaths per percentage point increase, respectively). Reference Fielding-Miller, Sundaram and Brouwer19 This study also found that the percentage of non-English speaking households in each county significantly influenced the COVID-19 mortality, with a notable increase in the number of reported deaths. Reference Fielding-Miller, Sundaram and Brouwer19 In New York City, COVID-19 death rates were 2.0 times higher in poor neighborhoods versus wealthy neighborhoods. Reference Calderón-Larrañaga, Dekhtyar and Vetrano20 Conversely, Texas census tracts with lower income levels experienced a reduced risk of COVID-19 infection incident rate (RR = 0.972; 95% confidence interval [CI], 0.953, 0.993). Reference Bauer, Zhang and Lee21 Rising unemployment and financial insecurity led to an increase in homelessness, which increased the risk of contracting COVID-19. Reference Coughlin, Sandel and Homelessness22
Education
Some studies found a link between the COVID-19 mortality rate and education. Regions with a high percentage of the population with college or associate degrees were found to have lower COVID-19 morbidity and mortality rates. Reference Paul, Arif and Pokhrel9,Reference Ogunyemi, Mantilla and Markus23 Moreover, Bauer et al. found that the risk ratio for COVID-19 incidence was found to be higher in census tracts with a greater percentage of the population with limited English proficiency (RR = 1.015; 95% CI, 1.003, 1.028). Reference Bauer, Zhang and Lee21 Nonetheless, a higher percentage of no high school education (RR = 0.987; 95% CI, 0.976, 0.998) was protective and associated with a reduced COVID-19 risk with census tract subgroup aged 19 to 34 y. Reference Bauer, Zhang and Lee21
Neighborhood and Built Environment
Transportation and Housing Quality
Bai et al. focused on the commuting behavior of New York residents and found that counties with a high volume of bi-directional commuting patterns were spreading COVID-19 at higher rates than other counties with a low volume of commuting patterns. Reference Bai, Jiao and Chen24 Counties with high inward commute scores were found to have the highest rates of COVID-19 infection, while counties with high outward commute scores had the lowest rates of infection but were thought to be the primary means of transmission. Reference Bai, Jiao and Chen24 Another study found that COVID-19 infections were more likely with housing (odds ratio [OR], 1.32; 95% CI, 1.16-1.5; P < 0.0001) and transportation insecurities (OR, 1.11; 95% CI, 1.02-1.23; P = 0.03). Reference Rozenfeld, Beam and Maier14 A similar trend found that housing and transportation disparities (adjusted IRR per 10 percentile increase: 1.05; 95% CI, 1.04 to 1.05; P < 0.001) predisposed to COVID-19 deaths. Reference Islam, Nayak and Hu25 Paul et al. reported that for every 5% increase in residential segregation among those who identified as Black or White, COVID-19 death rates increased by 3.4% (adjusted RR = 1.034; CrI = 1.019, 1.050). Reference Paul, Arif and Pokhrel9 Also, the percentage of renters and racial minorities were found to be significantly associated with increased COVID-19 risk (RR = 1.014; 95% CI, 1.008, 1.020 and RR = 1.018; 95% CI, 1.005, 1.032) for people ≥ 65 y, respectively. Reference Bauer, Zhang and Lee21 Moreover, higher rates of COVID-19 positive cases were significantly correlated with areas with greater green space density, public transportation, median distance traveled, carpooling, male percentage, and percentage commuting by walking. Reference Chen, Jiao and Bai26
Air Quality and Environmental Toxins
Health disparities related to air quality and occupational hazards have been found to exist among minority communities for years. For instance, Tessum et al. found that racial-ethnic minorities disproportionally inhaled fine particulate matter (PM2.5) air pollution from agriculture, coal, electric utilities, and residential wood combustion. Reference Tessum, Apte and Goodkind27 In this review, 1 study linked COVID-19 death rates to air pollution and found that any microgram per cubic meter (µg/m3) increases in long-term average PM2.5 (particles with a diameter of ≤ 2.5 μm) exposure caused an 8% increase in COVID-19 mortality rate. Reference Wu, Nethery and Sabath28 Moreover, Millett et al. found that higher PM2.5 scores were linked to poor social distancing practices in vulnerable communities. These findings highlight evidence that air quality and environmental toxins have contributed to increased morbidity and mortality. Reference Millett, Jones and Benkeser29
Healthy Food Access
Additionally, the intersectionality between food insecurity, racial discrimination, and social class has exacerbated health disparities within marginalized communities. For instance, limited access to healthy foods and green vegetables, residential segregation, and zoning policies that disproportionately increase access to high density fast food establishments were linked to COVID-19 outcomes within these communities. Reference Nittle30–Reference Sharma, Chuang and Rushing32
Health and Health-Care Access
Comorbidity and Mortality
The prevalence of comorbidities in a population is often associated with their socio-economic disparities. Reference Shin, Kwon and Shaban-Nejad33 The SARS-CoV-2 has disproportionally impacted minority communities. Multiple studies have shown that counties with a higher density of African Americans had a higher percentage of COVID-19 cases and death rates Reference Millett, Jones and Benkeser29,Reference Kim and Bostwick34 and hospitalization rates. Reference Gold, Wong and Szablewski35 Of particular significance, Kim and Bostwick found that areas with higher percentages of African American residents in Chicago were associated with higher SVI and COVID-19 risk factor scores. Areas comprised of <5% African American residents had a lower percentile of SVI ranging from −2.0639 to −0.8391, whereas areas comprised of >75% African American residents had a greater percentile of SVIs ranging from 0.9670 to 2.4588. Reference Kim and Bostwick34 Moreover, regions with a greater prevalence of African American residents had significantly higher COVID-19 death rates, with autocorrelation between the percentage of African Americans and COVID mortality being 0.41 while merely –0.33 for the percentage of White residents. Reference Kim and Bostwick34 As of April 2020, preliminary data indicated that 131 predominantly Black US counties recorded infectivity rate at 137.5/100,000 and the death rate at 6.3/100,000. These infectivity and death rates were 3- and 6-fold greater than those reported in White counties. A similar trend was recorded approximately a year later (by March 7, 2021) in another study where death rates were 178/100,000 among African Americans, 172/100,000 among American Indians/Alaska Natives, and 154/100,000 among the Hispanic population. 36 In contrast, COVID-related mortality rates among Whites (124/100,000) and Asians (95/100,000) were slightly lower. 36
Researchers found that underlying health inequalities and co-morbid health conditions increased susceptibility to COVID-19 infection and death. Reference Wang, Li and Lu4,Reference Smith5 For instance, increased COVID-19 mortality rates in urban (RR = 1.862; CrI = 1.704, 2.035) and rural (RR = 1.962; CrI = 1.783, 2.158) areas were linked to 5% increase in frequent mental distress. Reference Paul, Arif and Pokhrel9 Also, Yancy Reference Yancy37 elaborated on the higher prevalence of health comorbidities (hypertension, diabetes, obesity, cardiovascular disease, and mental illness) and restricted access to health care among African Americans. Likewise, many American Indian and Alaskan Native communities experienced lower life expectancy and suffered higher death rates from comorbidities including liver disease, diabetes mellitus, and pneumonia when compared with other racial groups. Reference Hathaway17
Access to Health-Care and Health Literacy
The Indian Health Service (IHS), an operating division within the US Department of Health and Human Services, was reported to have inadequate health facilities offering intensive care, thus requiring medical transfers to other locations. In some Navajo communities, the intensive care unit (ICU) facilities were quite far from the residences thus requiring helicopter transportation. Reference Gutman, Yang and Shakya38 Moreover, incomplete documentation of health records resulted in difficulty tracking hospitalization and mortality rates compelling some communities to keep records outside of the electronic health system. Reference Nagle39 Additionally, Native Americans are sometimes miscategorized or labeled as “others” in research studies thereby causing a lack of representation and complicating efforts to obtain pertinent information to address the health inequalities. Reference Nagle39 Increased COVID-19 morbidity/mortality have also occurred among susceptible elderly individuals who resided in rural areas with limited access to health care. Although Telehealth was reported to be relatively available, reliable high-speed Internet access remained a major challenge among rural populations. Given the importance of clear communication in health-care settings, language barriers also deterred accessing health-care needs.
Social and Community Context
Civic Participation and Discrimination
Although social distancing and the opportunity to work from home decrease exposure risk levels and are established as effective strategies to combating COVID-19, their implementation remain suboptimal among minority groups living in poverty, high-density neighborhoods, and multigenerational households. Reference Yancy37,Reference Webb Hooper, Nápoles and Pérez-Stable40,Reference Laurencin and McClinton41 Specifically, Heath Reference Heath42 addressed how social distancing was a daunting task for those unable to secure housing, eg, the homeless because they were compelled to share common spaces with other displaced individuals. These living conditions made it difficult to adhere to social distancing guidelines and maintain hygiene standards, thereby increasing susceptibility to COVID-19 spread. Reference Heath42
Drivers of health disparities such as structural racial injustices as well as social, historical, and political discriminations have caused communities of color to be disproportionately impacted by the pandemic. This was underscored by initial data from the pandemic which indicated that African Americans and Hispanics experienced substantially higher hospitalization and death rates. Reference Vasquez Reyes13,Reference Green, Fernandez and MacPhail43 In addition, prioritization of resources and shortage of beds, and ventilators placed the elderly in an extremely vulnerable situation given the overburdened health-care setting as they faced double discrimination. Reference Bauer, Zhang and Lee21 Gender imbalances were also exacerbated by the pandemic with women being more likely to give up their paid jobs to take on the responsibility of childcare following school closures. Reference Green, Fernandez and MacPhail43
Social Support
Some disadvantaged groups, eg, senior citizens, displaced individuals are less likely to access and harness social support systems and other informational resources with respect to transportation, health care, and companionship. Due to social distancing measures, some older adults encountered hardship stockpiling food supplies and other necessities. Reference Heath42 Also, the lack of community capacity and mobilization in deprived areas greatly impacted timely care and support for older patients and their affected families. 2
Discussions and Future Directions
The COVID-19, which has led to a global pandemic, has disproportionally impacted groups and populations across the United States. Lately, the COVID-19 pandemic has exacerbated SDoH inequalities even though these have persisted throughout health systems for years. Concurrently, SDoH inequalities have increased susceptibility to COVID-19 outcomes. We summarized and categorized our findings into the 5 SDoH domains defined by the Healthy People 2030’s taxonomy: (1) Economic Stability, (2) Education, (3) Neighborhood and Built Environment, (4) Health and Healthcare Access, and (5) Social and Community Context. Our review established that SDoH disparities were related to COVID-19 outcomes, ie, infectivity, hospitalization, and death rates.
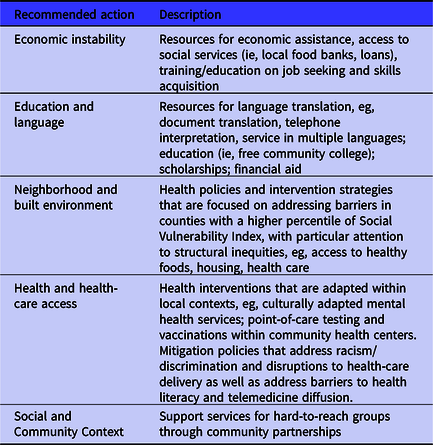
In addition to identifying SDoH disparities associated with COVID-19 outcomes, this study proposes that SDoH be incorporated into intervention strategies that address pandemic recovery and response (see Table 3). Investigating communities with public health surveillance and intervention strategies that address policies, health care systems, and society level determinants should be part of the solution process. Reference Webb Hooper, Nápoles and Pérez-Stable40 Moreover, “Moving forward, as the lessons of COVID-19 are considered, SDoH must be included as part of pandemic research priorities, public health goals, and policy implementation.” Reference Abrams and Szefler44 To plan and implement interventions for COVID-19 pandemic recovery and response, it is important to recognize and consider SDoH risk factors and vulnerabilities that may vary among different communities and populations. However, this process will require an in-depth understanding of minority communities to promote health equality for all its individuals. Maslow’s framework model proposed 5 hierarchies of needs: “physiology”, “safety”, “social”, “esteem”, and “self-actualization” which promote diversity in policy and health decision-making that are in the best interest of communities. Reference Ryan, Coppola and Canyon45 Moreover, Jani Reference Jani46 also recommended a heuristic approach to optimize the expenditure of limited resources and minimize the painful road to recovery following the pandemic. Meneses-Navarro et al. Reference Meneses-Navarro, Freyermuth-Enciso and Pelcastre-Villafuerte47 suggested that the government’s implementation of socio-culturally appropriate communication strategies include evidence-based best practices, due to mistrust of the government and health-care systems among minority communities. They emphasized that inequalities and barriers to health-care access should be eliminated for ground/air transportation and free health services during the COVID-19 pandemic.
Table 3. SDoH recommendations to address COVID-19 outcome disparities
Integrating SDoH indicators into intervention strategies should positively impact policies and decision-making regarding current/future pandemic preparedness and response. To a certain extent, preparedness ensures that “a degree of thought and resources are dedicated to generating the knowledge and materials needed for response to and recovery from actualized disasters.” Reference Ryan, Coppola and Canyon45 The inclusion of SDoH indicators into health-care systems and planning, designing, and implementation of intervention strategies facilitate a more holistic and systematic approach to mitigating the adverse impact of the ongoing crisis, particularly for the hardest-to-reach and most vulnerable population. Also, importantly, this approach ensures that specific societal needs are met and health education/promotion efforts adequately informed. While clusters of SDoH risk factors may coexist in certain individuals and communities, it is imperative that these are distinctly identified and adequately addressed. Moreover, artificial intelligence, epidemiological analyses/investigations (eg, ecological regression analyses, etc.), and other innovative disease surveillance methods are essential to rapidly access, understand, and effectively address the emerging big data sets from the ever-evolving COVID-19 health crises.
Our findings should be considered in light of some limitations. Our study was confined to only 2 database searches, as a result, it is possible that other significant studies not currently published in these databases were overlooked. Despite this limitation, our study identified SDoH disparities that exacerbate the ongoing public health threat particularly among vulnerable populations, and proposed the integration of SDoH into recovery efforts and pandemic preparedness. In addition, our study forms the basis for more extensive, in-depth systematic reviews and studies to gain insights on the short and long-term impacts of COVID-19 among minority communities.
Our future work is currently focused on implementing an Urban Population Health Observatory (UPHO) Reference Brakefield, Ammar and Olusanya48 that would generate actionable intelligence to improve COVID-19 surveillance. Actionable Intelligence investigates the causal pathways or effects between drivers (eg, SDoH indicators) and outcomes (eg, COVID-19 positive cases, COVID-19 morbidity, and mortality) and will involve the following processes: (1) collect and integrate data from multi-dimensional sources, (2) classify collected data into drivers and outcomes, (3) incorporate data science techniques to calculate measurable indicators from raw variables, and (4) examine the extent to which interventions are identified or developed to mitigate drivers that lead to the undesired outcomes. The design and development of a systematic surveillance platform that embeds SDoH indicators can improve equity in the distribution of quality health care and services, eg, vaccinations, inform policy/health decision-making from health officials, eg, on safety for re-openings, as well as address shortages of medical supplies to alleviate the health and economic crisis. Reference Shin and Shaban-Nejad49–Reference Ye51






