INTRODUCTION
Chronic airway infection and subsequent progressive respiratory and clinical decline is the pathological hallmark of cystic fibrosis (CF). Patients tend to follow a classical chronological course of bacterial airway infection from infancy to adulthood. This manifests as dominance of Haemophilus influenzae and Staphylococcus aureus in the airways of infants and children: by adulthood Pseudomonas aeruginosa dominates.
In recent years, a number of non-fermenting Gram-negative bacteria have also been noted to colonise the airways of individuals with CF. These include the species Stenotrophomonas maltophilia and Inquilinus limosus and the genera Achromobacter, Pandoraea, Ralstonia and Cupriavidus. The current prevalence of these organisms is low and is generally reported as less than 10% but is rising [1–Reference Lipuma5]. Of these emerging pathogens, Ralstonia spp., in particular, remain an unknown entity with their prevalence and clinical impact in CF not yet fully described.
The genus Ralstonia was proposed in 1995 [Reference Yabuuchi6] and currently comprises six named species of Gram-negative, non-fermenting bacteria: Ralstonia mannitolilytica; Ralstonia pickettii; Ralstonia insidiosa; Ralstonia pseudosolanacearum, Ralstonia solanacearum and Ralstonia syzgii, the latter of which comprises three subspecies, Ralstonia syzgii subsp. syzgii, Ralstonia syzgii subsp. indonesiensis and Ralstonia syzgii subsp. celebesensis [Reference Coenye7, Reference Safni8]. Of these named species, the three reportedly isolated from patients with CF are R. mannitolilytica, R. pickettii and R. insidiosa [Reference Coenye7–Reference Coenye10]. The remaining three species have not yet been reported in CF.
The prevalence of Ralstonia in CF is unknown but is likely to be low given studies reporting only a small number of positive samples [Reference Coenye, Vandamme and Lipuma9, Reference Burns11]. However, true prevalence may be underestimated as Ralstonia spp. are typically extremely antibiotic resistant and capable of growth on Burkholderia cepacia complex selective agar making culture-based diagnosis difficult and the genus vulnerable to misidentification. There is a recent case series reporting chronic infection of Ralstonia mannitolilytica in CF, although the authors did not include their definition of chronic infection [Reference Coman12].
There are no other reports of chronic infection in CF with Ralstonia spp and the clinical impact of airway infection with Ralstonia spp. in individuals with CF is unknown. The above-mentioned case series described seven patients with R. mannitolilytica infection with increased exacerbation frequency and accelerated lung function decline. However, the majority of these patients had multiple co-infections including P. aeruginosa and methicillin-resistant S. aureus and it is therefore difficult to conclude that R. mannitolilytica was solely responsible for their clinical course. There are no data in the literature on the ability of this organism to cause person-to-person transmission.
At Manchester Adult Cystic Fibrosis Centre (MACFC), which serves over 400 adults with CF, we have noticed a number of isolations of Ralstonia spp. from our patients over recent years. We aimed to calculate the prevalence of Ralstonia spp. in patients attending MACFC, to determine whether cross-infection may have occurred and whether infection was transient or chronic. We also aimed to describe prospectively the phenotype, including age, gender, body mass index (BMI), presence of diabetes, pancreatic insufficiency and chronic co-infections and also the clinical outcomes for Ralstonia-infected patients.
METHODS
Prevalence calculation
For each year from 2008 to 2016 the number of patients with at least one isolation of Ralstonia spp. was calculated using patient case notes and analysing computerised microbiological reports. The total number of patients attending MACFC each year was taken from administrative records. To determine if any apparent longitudinal increase in prevalence during the study period was statistically significant, we compared prevalence between tertiles of study period, divided equally by chronology (2008–2010, 2011–2013, 2014–2016) using a χ2 test.
MALDI-TOF identification and gyrB sequencing
All patients with ⩾1 isolation of Ralstonia spp. at MACFC from sputum between 1 January 2008 and 31 December 2016 were identified using the hospital laboratory's online reporting system. Isolates were sent for molecular confirmation of identification to AMRHAI, Public Health England where they underwent preliminary identification by Matrix-assisted Laser-Desorption/Ionization Time-Of-Flight Mass Spectrometry (MALDI-TOF MS), following ethanol and formic acid extraction on a Bruker Microflex instrument (Bruker). Polymerase chain reaction (PCR) confirmation to species level was conducted by gyrB gene amplification using primers PAR gyrB F/R, followed by sequencing with additional sequencing primers PC2 and PC3 [Reference Kenna13]. Briefly a few colonies of bacterial growth were suspended in 100 µl of PCR grade water, vortexed and centrifuged at 15 000 rcf for 2 min. PCR reactions were carried out in a PTC-225 Peltier Themal Cycler DNA Engine Tetrad (MJ Research) using QIAGEN Core Kit reagents in 25 µl volumes containing 1 X PCR buffer (containing 1·5 mM MgCl2), an additional 1·5 mM MgCl2, 1 X Q solution, 250 µM of each deoxynucleoside triphosphate, 1·5 U Taq DNA polymerase, 10 pmol of each primer and 3 µl crude DNA extract. Amplification conditions were as follows: 94 °C for 3 min, then 35 cycles of 94 °C for 30 s, 60 °C for 30 s, 72 °C for 45 s and a final extension of 72 °C for 10 min. PCR amplicons were separated and visualised using the QIAxcel capillary electrophoresis system (Qiagen) with a DNA High Resolution cartridge. PCR amplicons were purified using ExoSAP-IT® (Affymetrix), combined with the appropriate primer and submitted for sequencing on Applied Biosystems Capillary Sequencers to PHEs Genomic Services and Development Unit, Colindale, London. Sequence data were analysed using BioNumerics 6.1 (Applied Maths) and compared with each other and with those of Ralstonia species type and reference strains (LMG 6866 T R. mannitolylitica, NCTC 11149 T R. pickettii, LMG 17144 R. solanocearum, ATCC 49129 R. insidiosa, LMG 10661 T, R. syzgii subsp. syzgii, LMG 27703 T, R. syzgii subsp. indonesiensis and LMG 27706 T R. syzgii subsp. celebesensis) using the Neighbour-Joining method. gyrB sequence data were not available for the type or reference strains of R. Pseudosolanocearum.
Antibiotic susceptibility testing
Antimicrobial classes used in susceptibility testing were: aminoglycosides; antipseudomonal penicillins with β-lactamase inhibitors; antipseudomonal cephalosporins; carbapenems; fluoroquinolones; folate pathway inhibitors; monobactams; phenicols; polymyxins and tetracyclines. The specific antimicrobial agents used in susceptibility testing were: ceftazidime; aztreonam, ciprofloxacin; timentin; tobramycin; colistin; tazocin; meropenem; chloramphenicol; co-trimoxazole; minocycline and temocillin. Isolates were deemed multidrug-resistant if they were non-susceptible to ⩾1 agent in ⩾3 antimicrobial categories. For each sample, all different colonial morphotypes (usually between 3 and 5 per sample) underwent separate susceptibility testing in order to screen for multi-resistant phenotypes. At present, there is no national or international guidance on antibiotic susceptibility testing of Ralstonia spp isolates. In this study, the European Committee on Antimicrobial Susceptibility Testing (EUCAST) Pseudomonas susceptibility testing guidelines were used to interpret results for Ralstonia spp. isolates for ceftazidime, aztreonam, ciprofloxacin, timentin, tobramycin, colistin, tazocin and meropenem [14]. The EUCAST Enterobacteriacae susceptibility testing guidelines were used to interpret antibiotic sensitivities of Ralstonia spp. isolates for chloramphenicol and co-trimoxazole [14]. British Society of Antimicrobial Chemotherapy (BSAC) guidelines were used for temocillin and susceptibility testing, due to the lack of EUCAST data [15]. For minocycline susceptibility testing a locally derived zone diameter breakpoint of ⩾28 mm (susceptible) and <28 mm (resistant) was used due to the lack of both EUCAST and BSAC criteria, Mueller–Hinton (Oxoid) agar was used for all susceptibility testing.
Cross infection:strain typing
Isolates were typed using pulsed-field gel electrophoresis (PFGE) of XbaI-digested genomic DNA using the method described by Kaufmann [Reference Kaufmann16]. BioNumerics 6.1 (Applied Maths) was used to calculate percentage similarity using the Dice coefficient, with isolates clustered by Unweighted-Pair Group Method with Arithmetic Averages (UPGMA).
Cross infection: epidemiological analysis
Epidemiology of patients with shared strains was analysed by reviewing patient addresses, outpatient appointments, admissions, previous CF centres and questioning patients about their social behaviour. Clinics at MACFC run daily from Monday to Friday and patients are segregated into separate clinics according to their dominant classical infecting pathogen. Patients attending clinics also have segregated time slots to attend depending on presence or absence of Achromobacter spp., Pandoraea spp. or Ralstonia spp. infection. Additionally, within each clinic, patients are segregated from each other, clinic rooms are cleaned between patient and practice adheres to national infection control guidelines [Reference Littlewood17–Reference Jones19]. Spirometry is performed within the clinic rooms using single use spirettes within an ultrasonic flow sensing spirometer, which is cleaned between patients.
Prospective study participants
In September 2013, all patients attending MACFC with ⩾1 positive sputum culture of Ralstonia spp. in the preceding 2 years were identified by analysis of microbiological reports from our laboratory's electronic reporting system. These patients were then stratified by infection status (previous, intermittent or chronic) as outlined below. Patients identified as having intermittent or chronic infection with Ralstonia spp. were invited to participate if they were ⩾18 years old, capable of giving informed consent and able to provide sputum samples spontaneously, but had no history of HIV infection or solid organ transplantation. Study recruitment occurred between October 2013 and May 2014. Samples were collected under the framework of the Manchester Allergy, Respiratory and Thoracic Surgery Biobank with ethical approval of the National Research Ethics Service (REC reference 15/NW/0409).
Prospective study design
A prospective, longitudinal, observational study was performed with a total follow up time of 12 months from recruitment. Patients had a baseline visit then follow up visits at approximately three monthly intervals for a total duration of 12 months.
Sputum samples were collected at every visit. All samples underwent general, fungal and mycobacterial culture using standard and selective culture media in keeping with national guidelines [20]. As standard, all different colonial morphotypes growing on B. cepacia agar were identified using MALDI-TOF and each of these colonies underwent separate susceptibility testing (usually between 3 and 5 per sample). This approach was consistent for all samples obtained from patients attending MACFC, regardless of previous culture results.
At recruitment, blood was taken for full blood count and C-reactive protein (CRP). Clinical data were recorded for demographics, co-morbid factors, concurrent medication and recent acute antibiotic therapies at all study visits.
Spirometry was performed at each study visit using Easy on-PC Spirometers (ndd Medizintechnik AG, Zurich) in accordance with ATS/ERS spirometry guidance [Reference Miller21]. Baseline spirometry was taken as the best Forced Expiratory Volume in 1 Second (FEV1) the patient had achieved in the 6 months prior to study enrolment.
Definition of intermittent and chronic infection
There is no consensus agreement on a set of criteria to define an emerging pathogen infection as intermittent or chronic. The ‘Leeds criteria’, originally created to define P. aeruginosa infection status, were used to categorise infections as either intermittent or chronic in this study and are outlined below [Reference Lee22].
-
• Chronic infection: positive culture in >50% of months where sputum samples were taken over preceding 12 months
-
• Intermittent infection: positive culture in ⩽50% of months where sputum samples were taken over preceding 12 months
-
• Free of infection: no positive culture within the previous 12 months but previous history of positive airway culture
-
• Never infected: no history of positive airway culture
These criteria were chosen as they are already used at MACFC to categorise patients’ P. aeruginosa status. Also, using proportion of positive cultures to define an infection as chronic rather than an absolute number of positive cultures ensures that patients with large numbers of sputum culture results per year will not be classified as being chronically infected based on just one or two positive results.
RESULTS
Prevalence
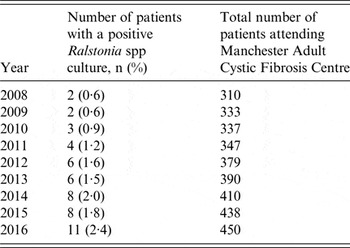
Between 2008 and 2016 the number of patients attending MACFC increased by 45%. The prevalence of Ralstonia spp. in patients attending MACFC has slowly risen from 0·6% in 2008 to 2·4% in 2016 (Table 1). The overall prevalence during 2008–2010 was 0·7%, was 1·4% during 2011–2013 and was 2·1% during 2014–2016 (p = 0·027). This shows a statistically significant difference between each time period. Of the 14 patients identified with one or more isolations of Ralstonia spp. in sputum since 2008, 12 (86%) have developed chronic infection. This is based on analysing sputum culture data from January 2016 to December 2016 for 10 patients and for the 12 months preceding lung transplantation for the remaining two patients (although notably both transplanted patients remained chronically infected post-transplantation). Each of the 12 patients had sputum samples taken from a minimum of three separate months and a maximum of 10 separate months during the 12-month period used to determine their infection status (mean number of months per year where a sputum sample was taken per patient was 6·4). For all 12 patients, Ralstonia spp. was cultured in 100% of months where sputum samples were taken.
Table 1. Prevalence of Ralstonia spp. infection at Manchester Adult Cystic Fibrosis Centre 2008–2016
MALDI-TOF identification and gyrB sequencing
Fourteen isolates from 13 patients were initially identified as R. mannitolilytica by Bruker MALDI-TOF MS with scores ranging between 1·74 and 2·3. One patient harboured two different strains of R. mannitolilytica. These 14 isolates clustered with 98·6% similarity to the type strain of R. mannitolilytica (LMG 6866) using gyrB sequence clustering. One of these 13 patients additionally harboured an isolate that did not cluster closely enough with any of the currently named species of Ralstonia within AMRHAI's gyrB database (Supplementary Fig. S1). The 14th patient was infected with a putative novel species of Ralstonia that did not amplify using the gyrB primers and was identified to genus level by 16S rRNA gene sequencing.
Strain typing
All 14 patients had successful genotyping of ⩾1 isolate using PFGE (Fig. 1) with nine (69·3%) patients having strains that were distinct from one another and from the remaining types. In two cases, patients harboured two distinct strains (patients 5 and 11, Fig. 1). Of the remaining five (35·7%) patients two shared a strain of R. mannitolilytica designated WYTH02RS-5, while three shared a further strain of R. mannitolilytica designated WYTH02RS-2. All patients that shared strains of R. mannitolytica were unrelated but, in both groups, the more recently infected patients had their first isolation of R. mannitolilytica during or immediately following an admission to the same ward as a patient already infected with that strain.

Fig. 1. Dendrogram of pulsed-field gel electrophoresis profiles of XbaI-digested genomic DNA from 16 Ralstonia species isolates from 14 patients attending Manchester Adult Cystic Fibrosis Centre 2008–2016. The line indicates 80% similarity.
Analysis of the home addresses of patients attending MACFC with at least one positive culture for Ralstonia species did not demonstrate a geographical link to suggest a particular postal area was linked to infection with WYTH02RS-2 or WYTH02RS-5 strains. In fact, the majority of patients infected with unique Ralstonia spp. strains lived in closer proximity than individuals sharing a strain of R. mannitolilytica.
Antibiotic resistance patterns
Antibiotic resistance patterns for Ralstonia spp. isolates from all 14 patients are shown in Table 2. Isolates from five of the 14 patients (36·7%) were resistant to all antibiotics tested. All isolates, where reported, were resistant to ceftazidime, aztreonam, timentin, tobramycin, colistin, meropenem, chloramphenicol and temocillin. Of the 13 isolates that underwent antibiotic susceptibility testing, the majority (69%) were susceptible in vitro to minocycline. Analysis of antimicrobial resistance patterns of WYTH02RS-2 strains from each infected patient revealed identical susceptibility profiles. Isolates from all three patients were resistant to all antimicrobials tested (ceftazidime, aztreonam, ciprofloxacin, tobramycin, colistin, tazocin, meropenem, chloramphenicol, co-trimoxazole, minocycline and temocillin). Similarly, isolates from both patients infected with WYTH02RS-5 had identical antimicrobial susceptibility profiles with isolates showing susceptibility to minocycline but resistance to all other antimicrobials tested (ceftazidime, aztreonam, ciprofloxacin, tobramycin, colistin, tazocin, meropenem, chloramphenicol, co-trimoxazole and temocillin).
Table 2. Antibiotic susceptibility testing results of Ralstonia spp. isolates from 14 patients attending Manchester Adult Cystic Fibrosis Centre

R, resistant; I, intermediate; S, sensitive.
Prospective study results
All five eligible patients with Ralstonia spp. isolated from sputum within the previous 2 years were recruited. Patient demographics and baseline investigations are shown in Table 3. At baseline, all of the patients had chronic infection and remained chronically infected at the end of the study period.
Table 3. Baseline characteristics of patients infected with Ralstonia spp. attending Manchester Adult Cystic Fibrosis Centre
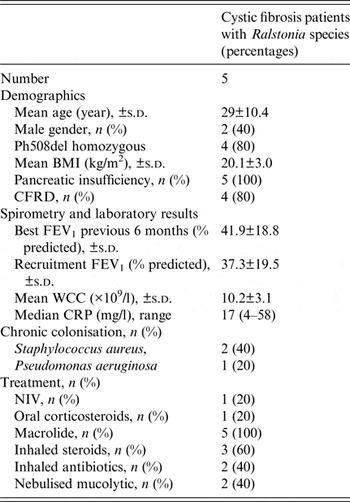
SD, standard deviation; BMI, body mass index; CFRD, cystic fibrosis related diabetes; WCC, serum white cell count; CRP, C-reactive protein; NIV, non-invasive ventilation.
Patients with chronic Ralstonia spp infection were predominantly Ph508del homozygous and diabetic and all were pancreatic insufficient. Lung function tended to be moderately to severely impaired. Long-term nebulised antibiotic therapy was used in two of the five patients (one patient was taking nebulised meropenem and the other patient was taking nebulised aztronam). Chronic co-infecting pathogens were relatively uncommon and there was a relatively low prevalence of chronic P. aeruginosa colonisation (20%).
DISCUSSION
There are very few published data on Ralstonia spp. infection in CF. To date, available literature mainly focuses on microbiological identification techniques and repository data. Here, we present the first single centre study on infection with Ralstonia spp. in CF with prevalence, genotyping, antimicrobial resistance and clinical data.
The current prevalence of Ralstonia spp. at our centre is low at 2·4% but appears to be gradually rising. Data from our study suggest a high risk of developing chronic infection following first acquisition of Ralstonia spp. in CF (86% of infected patients). There is very limited previous data on the ability of Ralstonia spp. to cause chronic infection. In 2002, Coenye et al. found only three out of 38 patients (7·9%) in their study had more than one positive culture for Ralstonia spp. [Reference Coenye, Vandamme and Lipuma9]. However, they did not describe the number of positive samples these patients had and whether they developed chronic infection, perhaps as it was a reference laboratory and relied on samples being sent from other laboratories. Our study shows a much higher risk of chronic infection developing; the difference between these two study findings may be due to improvements in detection of Ralstonia spp. in the past 15 years and a higher sampling frequency in our study. A case series published in 2016 has described seven patients with chronic R. mannitolilytica infection since the Canadian CF centre opened in 1984 [Reference Coman12]. However, the authors did not provide criteria used to define chronic infection nor did they state the number of positive cultures each of the seven patients had.
There is no evidence for an appropriate or effective antibiotic eradication regimen for Ralstonia spp., which is often multi-resistant and, at present, eradication is not routinely attempted at MACFC. There are no data in the literature on the resistance patterns commonly seen in this genus. Our study has found that all patients’ isolates of Ralstonia spp. were multidrug-resistant with over a third of patients harbouring strains resistant to all antibiotics tested. The antibiotic with the greatest in vitro activity was minocycline with 69% of patients harbouring strains susceptible to this antibiotic. The multi-resistant nature of this genus, combined with lack of evidence for suitable targeted antibiotic therapies, is likely to contribute to the high proportion of chronic infection amongst these patients.
R. mannitolilytica accounted for all but one of the 14 (92·8%) patients who have had at least one isolation of Ralstonia spp. since 2008. No other named species were isolated from patients attending MACFC. The majority (59·7%) of the 72 Ralstonia spp. isolates analysed by the University of Michigan's Burkholderia cepacia Research Laboratory and Repository were also R. mannitolilytica followed by R. picketii, which accounted for 34·8% of isolates [Reference Lipuma5]. The remainder of isolates were R. insidiosa.
Of the 13 patients that had a history of R. mannitolilytica infection, a pair and a group of three unrelated patients harboured the same strains. In the pair of patients, the most recently infected individual had their first positive culture during an admission to the same cystic fibrosis ward as a chronically infected patient. In the group of three patients, the second patient to be infected had their first positive culture following an admission to the same ward as a patient who had already been chronically infected for several years. The third patient's first positive culture coincided with an inpatient admission to the same ward as the second patient who had become chronically infected with the WYTH02RS-2 strain. It is possible that cross-infection occurred during these inpatient stays. All patients admitted to inpatient beds on our specialist CF ward have single occupancy rooms with en suite facilities and infection prevention policies and procedures are strictly adhered to by staff and advised and actively enforced to patients. However, we cannot exclude possible cross-infection during these hospital stays, nor are we able to exclude independent acquisition from an environmental source. Environmental sampling was not performed as part of this study. Of note, in the pair of patients sharing the WYTH02RS-5 strain, the patients lived over 50 miles apart; similarly the group of three patients sharing a further strain of R. mannitolilytica (WYTH02RS-2) lived between 15 and 60 miles apart. The possibility that the Ralstonia genus might be clonal in nature, making inferring cross-infection less convincing, was also considered. Of 25 Ralstonia spp. isolates from five hospitals examined by PFGE by AMRHAI, two other different shared strains were found in addition to WYTH02RS-2 and 5, the remaining 14 isolates had unique profiles, suggesting this is less likely to be the case, although a larger selection of Ralstonia sp. isolates needs to be examined for clonality of these organisms to be accurately assessed.
Numbers of patients included in the prospective study were small making it difficult to draw firm conclusions. The lung function of patients infected with Ralstonia spp. tended to be severely impaired, despite a relative lack of chronic co-infections with classical CF pathogens. This may suggest an increased vulnerability to Ralstonia spp. infection in advanced lung disease or that Ralstonia spp. infection is a cause of accelerated lung function decline. However, larger prospective case-controlled studies would be required to investigate this further.
In summary, prevalence of Ralstonia spp. is low at MACFC, but is slowly increasing. The risk of a patient developing chronic infection with Ralstonia spp following first acquisition is high. Shared strains of R. mannitolilytica were identified in our centre in a pair and a group of three unrelated patients with epidemiological connections. However, the numbers of such patients are too small to establish whether cross-infection or acquisition from a common environmental source is responsible. Patients with chronic Ralstonia spp. infection in our study have moderate to severe lung function impairment. Whether Ralstonia spp infection leads to accelerated lung function decline or whether our findings reflect that patients with advanced lung disease are more susceptible to infection with this organism need to be evaluated in larger prospective studies.
SUPPLEMENTARY MATERIAL
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268817001728
ACKNOWLEDGEMENTS
The authors acknowledge the Manchester Allergy, Respiratory and Thoracic Surgery Biobank and the North West Lung Centre Charity for supporting this project. In addition, the authors would like to thank all study participants for their contribution. The authors also like to thank Gemma Edwards and Matthew Smith (University Hospital of South Manchester Microbiology Laboratory) and Claire Perry, Amy Coward and Daniel Lilley (AMRHAI Reference Unit). This report is independent research supported by National Institute for Health Research South Manchester Respiratory and Allergy Clinical Research Facility at University Hospital of South Manchester NHS Foundation Trust. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
DECLARATION OF INTEREST
None.







