Fig. 1
Published online by Cambridge University Press: 23 March 2020
Inflammatory bowel diseases (IBDs) have high social impact. Aetiology is still unknown, however multifactorial genesis is surely implicated. We tried to correlate IBDs and psychological distress through evaluated psychometrical instruments and subsequently to relate subjective influences with gastroenteric clinical manifestation, defining new critical elements on which IBD are based.
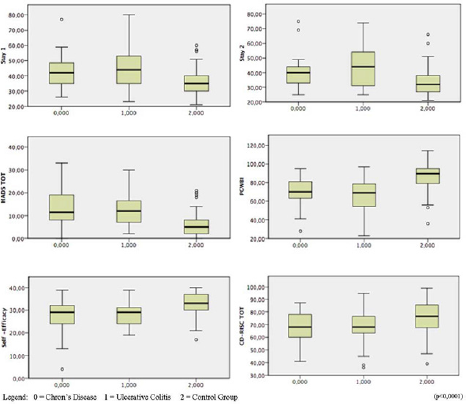
In our study, we included 57 participants, selected according to their diagnosis, between those attending our gastrointestinal ambulatory: 26 had Chron's disease, while 31 had ulcerative colitis. 78 people without gastroenteric or psychiatric disorder were also included in the study as control group. Psychometric questionnaires were administered to evaluate anxiety and depressive symptoms, quality of live, self-efficacy and resilience (Fig. 1).
Levels of anxiety and depression were higher in patients with IBDs than in the control group. STAI-Y highlighted higher state anxiety and trait anxiety levels in first group. HADS showed higher scores in ill patients, as well as CD-RISC showed a more impaired resilience. EQ-VAS, PGWBI and GSE revealed significant differences in health status, psychological wellness and self-efficacy between the two groups.
IBDs seem related to psychological diseases. Affected patients have higher anxiety and depression levels than general population as well as lower self-efficacy and resilience. Those elements being strictly linked to physical discomfort contributes to develop a loop in which patients get caught. Creating a model of integrated cooperation between gastroenterologist and psychiatrist during treatment of patients with IBDs seems fundamental to grant at once all the professional figures each patient needs for better care.
The authors have not supplied their declaration of competing interest.
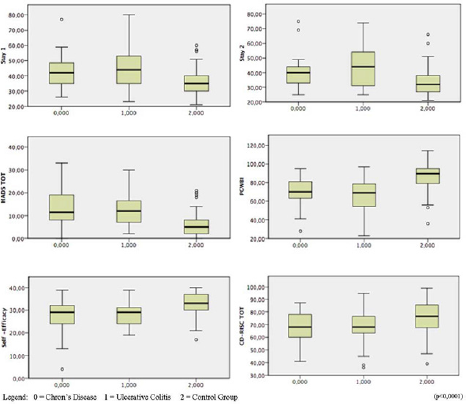
Fig. 1

Fig. 1
Comments
No Comments have been published for this article.