No CrossRef data available.
Published online by Cambridge University Press: 13 August 2021
Anticholinergic medications block cholinergic transmission. The central effects of anticholinergic drugs can be particularly marked in patients with dementia. Furthermore, anticholinergics antagonise the effects of cholinesterase inhibitors, the main dementia treatment.
This study aimed to assess anticholinergic drug prescribing among dementia patients before and after admission to UK acute hospitals.
352 patients with dementia were included from 17 hospitals in the UK. All were admitted to surgical, medical or Care of the Elderly wards in 2019. Information about patients’ prescriptions were recorded on a standardised form. An evidence-based online calculator was used to calculate the anticholinergic drug burden of each patient. The correlation between two subgroups upon admission and discharge was tested with Spearman’s Rank Correlation.
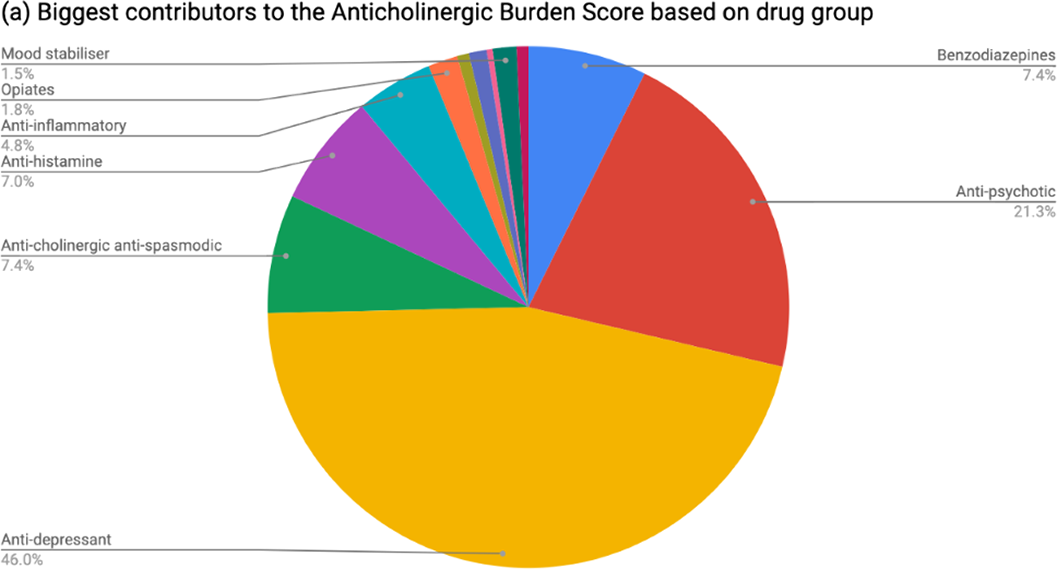
Table 1 shows patient demographics. On admission, 37.8% of patients had an anticholinergic burden score ≥1 and 5.68% ≥3. At discharge, 43.2% of patients had an anticholinergic burden score ≥1 and 9.1% ≥3. The increase was statistically significant (rho 0.688; p=2.2x10-16). The most common group of anticholinergic medications prescribed at discharge were psychotropics (see Figure 1). Among patients prescribed cholinesterase inhibitors, 44.9% were also taking anticholinergic medications.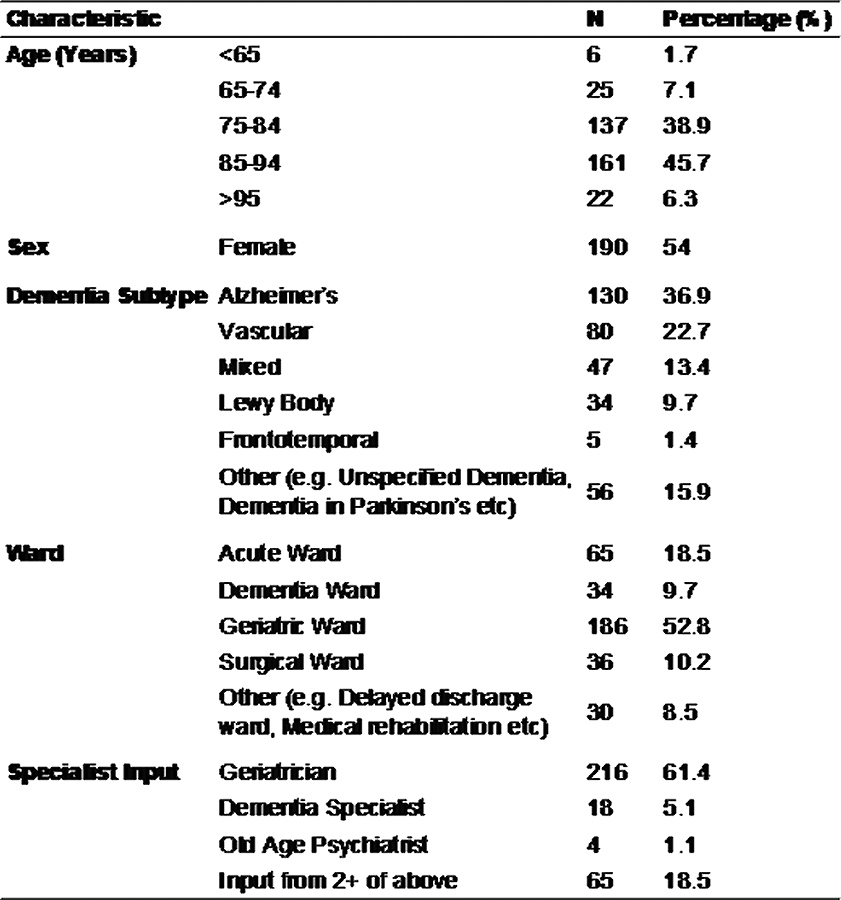
This multicentre cross-sectional study found that people with dementia are frequently prescribed anticholinergic drugs, even if also taking cholinesterase inhibitors, and are significantly more likely to be discharged with a higher anticholinergic drug burden than on admission to hospital.
This project was planned and executed by the authors on behalf of SPARC (Student Psychiatry Audit and Research Collaborative). We thank the National Student Association of Medical Research for allowing us use of the Enketo platform. Judith Harrison was su
Comments
No Comments have been published for this article.