1. Introduction
Youth depression is one of the most prevalent disorders in children and adolescents. The prevalence rate in childhood is about 2.8%, and increases during the course of adolescence (5.6%) [Reference Costello, Erkanli and Angold1]. Research has shown no gender differences in prevalence rates of depressive disorders in children, but the rate is twice as high in adolescent girls compared to boys [Reference Thapar, Collishaw, Pine and Thapar2]. Depression has a high burden of disease [Reference Murray3], an increased risk of suicide [Reference Harrington4], development of disruptive behaviors, problematic substance use [Reference Chassin, Beltran, Lee, Haller, Villalta, Ingram and Price5], poor school performance and social functioning [Reference Smit, Bohlmeijer and Cuijpers6]. A major concern is that almost 50% of adolescents who have a depressive episode will have a recurrence within five years [Reference Curry, Silva, Rohde, Ginsburg, Kratochvil and Simons7]. Therefore, evidence-based treatment for youth with depression is essential.
Most pharmacological treatment have an unfavorable risk-benefit profile, their use is often not effective and controversial due to the possible increased suicide risk [Reference Cipriani, Zhou, Del Giovane, Hetrick and Qin8]. Therefore evidence-based psychological interventions are often the first choice of treatment. For example, NICE guidelines recommend cognitive behavioral therapy (CBT) as an evidence-based psychological intervention for mild, moderate and severe depression [Reference Murray and Cartwright-Hatton9]. Although CBT is effective, several meta-analyses have shown that effect sizes are small to moderate when utilized as indicated prevention for youth [Reference Hetrick, Cox, Witt, Bir and Merry10] or treatment for children [Reference Yang, Zhou, Zhou, Zhang, Pu and Liu11] and adolescents [Reference Klein, Jacobs and Reinecke12]. So far, other treatments have not led to larger effect sizes. For instance, interpersonal psychotherapy (IPT) has not been shown to be more effective than CBT as a treatment for adolescent depression [Reference Weisz, Kuppens, Ng, Eckshtain and Ugueto13].
So the next step in psychological intervention research is to identify effective mechanisms of existing psychological interventions in order to enhance the effectiveness [Reference Holmes, Ghaderi, Harmer, Ramchandani, Cuijpers and Morrison14], for a substantial proportion of youths with depression it’s especially relevant to help increase the limited effectiveness of CBT. It is possible to test differential effectiveness of CBT because CBT protocols are known to vary in the presence of different components, and contextual and structural factors [Reference Fréchette-Simard, Plante and Bluteau15]. For example, the Problem Solving For Life Project intervention [Reference Sheffield, Spence, Rapee, Kowalenko, Wignall and Davis16] does not have relaxation and challenging thoughts as part of treatment and ‘On Full Power’ [Reference Wijnhoven, Creemers, Vermulst, Scholte and Engels17] does, and the CBT intervention in the ‘Treatment of Adolescents with Depression Study’ does involve parents and the ‘Coping with depression for adolescents’ doesn’t [Reference Weersing, Rozenman and Gonzalez18]. Some work has been done to identify influential factors on treatment outcome in recent reviews [Reference Hetrick, Cox, Witt, Bir and Merry10, Reference Yang, Zhou, Zhou, Zhang, Pu and Liu11, Reference Dowell and Ogles19, Reference Arnberg and Ost20], but none of these studies have investigated if a certain individual component or a combination of intervention components improve the effectiveness of CBT.
Building the body of evidence for these influential factors, can help to personalize CBT so it can better fit the individual child or adolescent, which may potentially reduce costs and prevent harm by reducing the use of non-effective or counterproductive components of CBT in youth.
The aim of the current systematic review and meta-analysis is to identify components of CBT, as well as contextual and structural factors, which could influence treatment outcomes of CBT. We therefore set out to systematically identify controlled studies on the effectiveness of CBT in youth with clinical and subclinical symptoms of depression. Moreover, all CBT intervention protocols were rated for the presence of specific intervention components, and contextual and structural factors.
2. Methods
This review is conducted according the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [Reference Moher, Liberati, Tetzlaff and Altman21] (Appendix A for the PRISMA-checklist).
2.1. Eligibility criteria
We pre-specified our inclusion and exclusion criteria and included randomized controlled trials (RCTs) investigating CBT as an indicated prevention or treatment intervention for youth with subclinical depressive symptoms or with a clinical depressive disorder. CBT must have been delivered to children and adolescents (and caregiver(s)). At least one control condition in the study had to be an inactive intervention (for example, waitlist, no intervention, placebo, monitoring or an attention control group). Active control interventions (including treatment as usual) were not included due to the amount of expected heterogeneity it would create in the meta-regression and because a head to head comparator contain elements of CBT. Also, the majority of active control interventions contained some elements of CBT, mostly combined with other non-CBT elements. This comparison would not give a representative insight into the efficacy of specific CBT elements. Therefore, only passive control groups, without any type of CBT elements, were included into the study. Furthermore, only articles that were written in English or Dutch were included. Finally, RCTs from before 1990 were excluded because we expected intervention protocols to be irretrievable before this date.
2.2. Search strategy
CINAHL, CENTRAL (Cochrane), EMBASE, MEDLINE/PubMed and PsycINFO (including dissertation abstracts) were searched from inception to the 4th of September 2017. The searches were undertaken by a librarian using terms for children and adolescents, depression, randomized controlled trials, systematic reviews and meta-analyses; all search strings are reported in Appendix B. We then searched the reference lists of all the included and excluded studies and previous systematic reviews and meta-analysis. We also contacted authors of studies to request additional data. Two authors (LdW, RAT/MO) independently performed the title/abstract and full text selection, and disagreements were resolved through consensus.
2.3. Assessment of bias and confidence in results
Each included study was assessed independently by two authors (LdW, RAT/MO) using the Cochrane Collaboration Risk of Bias Assessment Tool [Reference Higgins, Green and Cochrane Collaboration22]. The level of agreement was moderate (κ = 0.60). Disagreements were resolved by consensus. Each study was rated for risk of bias (RoB) on sequence generation, allocation concealment, masking of participants, assessors and providers, selective outcome reporting and incomplete data. RoB for each domain was rated as high (seriously weakens confidence in the effect estimate), low (unlikely to seriously alter the effect estimate), or unclear.
Confidence in the effect estimates of the meta-analysis were assessed by MO and LdW using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) method [Reference Guyatt, Oxman, Schünemann, Tugwell and Knottnerus23], which is a structured assessment of the quality of evidence attending to the following factors: RoB, inconsistency, indirectness, imprecision and publication bias. Outcomes can be ‘downgraded’, based on the aforementioned factors resulting in ‘high’, ‘moderate’, ‘low’ or ‘very low’ confidence in the effect estimate.
2.4. Data management
Outcome measures included depressive symptoms, quality of life, number of youth diagnosed with a depressive disorder, recovery (no longer meeting DSM criteria), remission (different criteria of symptom decrease on various scales), response (Clinical Global Impressions–Improvement scale of (very) much improved) rate. The continuous measures are listed in Appendix C. If outcome data were missing or could not be used in the meta-analyses, authors were asked to provide additional data. We also extracted the following: the country in which the study was undertaken, setting, intervention format (face-to-face, bibliotherapy, online, and individual/group-based), number and length of sessions, attrition rate and participant details (mean age, proportion of females, proportion of participants using antidepressants at baseline, and proportion of participants with a diagnosis of major depressive disorder (MDD), dysthymia and/or comorbid anxiety disorder).
Most articles don’t provide detailed information regarding the investigated protocol [Reference Fréchette-Simard, Plante and Bluteau15]. It’s often unclear which modules of CBT are used, how the intervention was given and in which dosage. Since we were interested in this information, we developed a taxonomy to rate protocols. This taxonomy consists of a checklist in which different aspects of a protocol can be screened, namely CBT components (psychoeducation, cognitive restructuring, behavioral activation, monitoring, problem solving, relaxation, social skills, positive reinforcement (reward), modelling, setting goals, relapse prevention), contextual factors (for example, target population, target, theory) and structural factors (for example, content, dose, frequency, sequence). The content of the taxonomy is based on work of Chorpita and colleagues [Reference Chorpita, Becker and Daleiden24–Reference Chorpita and Daleiden26], and expert consensus. We used this taxonomy to rate protocol manuals.
Protocol manuals were requested by contacting the primary investigator or a co-author of the included studies. The taxonomy was applied to four of these manuals by three raters (DB and two pedagogs) trained in CBT. Additionally they received a training in the taxonomy explaining the specific parts and pitfalls. After the four manuals were rated, there was a meeting in which the raters discussed the agreements and disagreements. Some aspects of the taxonomy were adapted for clarification purposes. Also, some aspects of the taxonomy were difficult to rate (e.g. the dosage of each step of a specific component), therefor they were deleted. The four manuals were rated again and high consensus (90%) was obtained. Then, the two raters supervised by DB applied the taxonomy to the remaining manuals individually. It is unclear to which extent the manuals were actually applied in the included studies.

Fig 1. Flow Chart.
2.5. Statistical analysis
2.5.1. Meta-analysis
We conducted meta-analyses for different comparison groups and outcome types using Review Manager (RevMan) 5.3 [27]. Overall effects were calculated using random effects models and weighted by the inverse of variance [Reference Higgins, Green and Cochrane Collaboration22]. For continuous outcomes, we calculated the standardized mean difference (SMD), Hedges’ g, for between-group differences. SMDs were considered small (0.2 ≤ SMD<0.5), medium (0.5 ≤ SMD<0.8) or large (SMD ≥ 0.8) [Reference Cohen28]. For dichotomous outcomes, we calculated the risk ratio (RR) for events. All outcomes were reported with 95% confidence intervals (CIs). Statistical heterogeneity was assessed by MO by visual inspection of forest plots, by performing the χ2 test (assessing the 95% CIs), and by calculating the I² statistic, which describes the percentage of observed heterogeneity that would not be expected by chance. I² was considered moderate if it exceeded 50% and high if it was more than 75% [Reference Higgins, Thompson, Deeks and Altman29].
Table 1a Study characteristics per study.

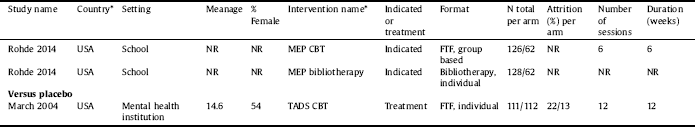
* 6-CDPI = 6-session CBT depression prevention intervention group; ACSC = Adolescent coping with stress class; ATS = ACT & THINK skills; AU = Australia; BAND = Belonging against Negative Thinking and Depression; BE = Belgium; CA = Canada; CH = China; CSG = Cognitive skills group; CTDSY = Cognitive Therapy Treatment manual for Depressed and Suicidal Youth; CWD-A = The Coping With Depression Course for Adolescents; FG = Feeling Good; FTF = Face-to-face; GO = Grasp the Opportunity; HK = Hong Kong; MEP = Mood Enhancement Program; NL = The Netherlands; NR = Not Reported; NZ = New Zealand; OVK = Op Volle Kracht [On Full Power]; PA = Pak Aan [Taking Action]; PASCET = Primary and Secondary Control Enhancement Training; POP = Penn Optimism Program; PSL = Problem Solving for Life project; PST = Problem solving therapy; RAP = Resourceful Adolescent programme; SB = Stressbusters; SCT = Social competence training; SPARX = Smart, Positive, Active, Realistic, X-factor thoughts; TADS = Treatment for Adolescents With Depression Study; UK = United Kingdom; USA = United States of America; TH = Thailand.
2.5.2. Meta-regression
To explain heterogeneity, and assess which CBT components or contextual and structural factors influence the overall efficacy of the CBT intervention, a meta-regression analysis was performed using STATA 12.1 [Reference StataCorp30]. Due to the large number of variables that could be used and the limited studies available, we had to limit these variables to prevent type 1 errors [Reference Thompson and Higgins31]. Therefore, we decided to perform two separate meta-regressions: one on CBT components and another on the contextual and structural factors; both meta-regressions would include the type of control condition and RoB. To further limit the number of included variables, a pre-specified hierarchy (Appendix D) was prepared that was based on children and adolescents’ views on the effectiveness and feasibility of intervention components [Reference Ng, Eckshtain and Weisz32] and clinical expert opinion from DB and YS. Finally, we determined that there should be a sufficient distribution of the presence or absence of variables between studies, within a study we chose for an arbitrary cut-off of at least 15% meeting one of the dichotomous criteria (15–85 ratio). Potential collinearity between the included variables was assessed by calculating the associations between the variables using a Spearman correlation matrix. For variables that were significantly associated with each other, the correlating variable that was lower on the pre-specified hierarchy of important variables was removed from the meta-regression model.
3. Results
3.1. Study flow
Of the 3974 potentially relevant citations from our database search, and nine through our hand search, we retrieved 284 full-text articles. A total of 215 articles were excluded in the full-text selection because of ineligible study design (k = 34), irrelevant outcomes (k = 17), the intervention was universal or selective prevention (k = 14) or not CBT (k = 21), participant samples that did not match our target population (k = 51), active comparison condition (k = 65), the article was not reported in English or Dutch (k = 6), the article was published before 1990 (k = 3), the article reported on an already included study with no new results (k = 3) and study data were not available (k = 1). The 69 remaining articles, published between 1990 and 2017, reported on results of 31 studies. More information about the study flow can be found in Fig. 1.
3.2. Study and intervention characteristics
Of the 31 studies (n = 4335) included in the quantitative syntheses, a total number of 2369 participants were randomized into the CBT intervention group and 1966 participants into the control group. The mean age of the 4335 participants was 14.2 years. Further study characteristics are reported per included study in Table 1a and summarized in Table 1b.
Thirty-seven CBT intervention arms containing 27 different types of CBT protocols were identified. If the protocol was not available (k = 12), the information within the published article was used to identify characteristics of CBT. If information on intervention components could not be identified it was labelled as missing/unclear. Table 2 provides a short description of context and structure characteristics of CBT, and an overview per intervention of the different components of CBT included in the meta-regression analysis.
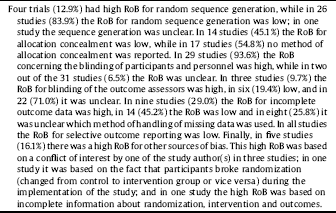
3.3. Risk of bias
Thirty trials were labelled as having a ‘high’ RoB and 1 trial as having a ‘low’ RoB. An overview of RoB criteria scores per included study is presented in Table 3a and summarized in Table 3b.
3.4. Overall quality of the evidence
Using the GRADE method [Reference Guyatt, Oxman, Schünemann, Tugwell and Knottnerus23] many outcomes were downgraded because of imprecision, mostly due to the CI crossing the threshold of no clinically important benefit. About half of the outcomes were downgraded for RoB. The amount of inconsistency in the results was low. There was no high-quality evidence, but moderate quality evidence was found for depression outcomes at post-treatment and follow-up (17–39 weeks) and for risk of having a diagnosis of depressive disorder at follow-up (17–39 weeks). Other evidence was of low or very low quality.
Table 1b Study characteristics summarized.
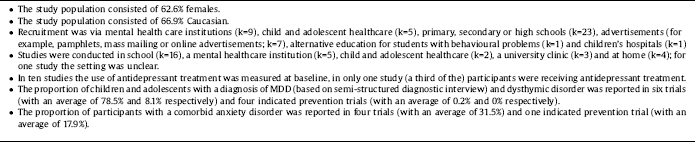
Table 2 Context and structure characteristics and overview of intervention components.

See Table 1a for meaning of abbreviations.
3.5. Quantitative data synthesis
Overall results and results of subgroups (different control conditions) are presented in Table 4 (post-treatment) and Table 5 (follow-up).
3.5.1. Overall results
3.5.1.1. CBT vs passive control
Low-quality evidence was found for CBT being associated with a small effect on depressive symptoms at post-treatment and at follow-up. Six trials reported low-quality evidence of CBT increasing the chance of remission by 45% and recovery by 36% at post-treatment. Low to very low-quality evidence provided inconclusive results on response, number of youths with a depressive disorder and quality of life.
Table 3a RoB criteria score per study.

Caption: Risk of bias was rated as low (+), high (−), or unclear (?).
Table 3b RoB criteria score summary.
3.5.2. Subgroups results
3.5.2.1. CBT vs waitlist/no treatment
Nineteen RCTs (n = 1760) compared CBT with a waitlist condition [Reference Sheffield, Spence, Rapee, Kowalenko, Wignall and Davis16, Reference Wijnhoven, Creemers, Vermulst, Scholte and Engels17, Reference Ackerson, Scogin, McKendree-Smith and Lyman33–Reference Kaesornsamut, Sitthimongkol, Williams, Sangon, Rohitsuk and Vorapongsathron49]. Very low-quality evidence was found for CBT being associated with a medium effect on depressive symptoms at post-treatment when compared to waitlist. There was moderate quality evidence for a small effect on depressive symptoms and 63% less risk of having a depressive disorder at follow-up. Very low-quality evidence was found for CBT increasing the chance of remission by 77% and low-quality evidence for increasing the chance of recovery by 36% at post-treatment. However, low to very low-quality evidence provided inconclusive results for risk of having a depressive disorder and quality of life at post-treatment.
3.5.2.2. CBT vs attention control
Eight RCTs (n = 1599) compared CBT with an attention control condition [Reference Brent, Kolko, Birmaher, Baugher, Bridge and Roth50–Reference Wright, Tindall, Littlewood, Allgar, Abeles and Trepel57]. Moderate quality evidence was found for CBT being associated with a small effect on depressive symptoms when compared with attention control at post-treatment. There was low-quality evidence from two studies (n = 125) that CBT reduces the risk of being diagnosed with a depressive disorder by 51% at post-treatment. However, low to very low-quality evidence provided inconclusive results for remission and remission rate at post-treatment and depressive symptoms and number of youths with a depressive disorders at follow-up.
3.5.2.3. CBT vs monitoring control
Three RCTs (n = 753) compared CBT (administered as indicated prevention) with a monitoring control condition [Reference Poppelaars, Tak, Lichtwarck-Aschoff, RCME, Lobel and Merry58–Reference Rohde, Stice, Shaw and Gau60]. Moderate quality evidence was found for CBT being associated with no clinically important benefit on depressive symptoms when compared with monitoring control at post-treatment and at follow-up. However, confidence intervals were compatible with both an increase in effect and no clinical important benefit.
3.5.2.4. CBT vs placebo
One RCT (n = 223) compared CBT with a placebo pill [Reference Curry, Rohde, Simons, Silva, Vitiello and Kratochvil61]. (Very) low-quality evidence provided inconclusive results for depressive symptoms, remission, response and quality of life at post-treatment.
3.6. Meta-regression
Significant statistical heterogeneity was detected when CBT was compared with passive control on depressive symptoms at post-treatment (I² = 81% [95% CI: 74–86%]) and at follow-up (I² = 68% [95% CI: 45–79%]). To perform a meta-regression we first established the variables (Table 6) on our predefined method (see Statistical analysis in the method section of the paper). Results of the meta-regression analyses of depressive symptoms of CBT intervention components and of contextual and structural factors can be found in Tables 7 and 8 respectively.
Recipient, behavioral activation and challenging thoughts as a predictor
In the intervention component meta-regression model, self-monitoring and social skills training were excluded, because they were significantly correlated with respectively behavioral activation (ρ = 0.657; p < 0.01) and psychoeducation (ρ = 0.425; p < 0.05). In the meta-regression, behavioral activation (b= −0.202; p < 0.01) and challenging thoughts (as part of cognitive restructuring; b = −0.312; p < 0.05) were significantly associated with a larger effect on depressive symptoms at follow-up. However, these treatment components (behavioral activation and challenging thoughts) were not significant predictors when they were analyzed individually in the meta-regression model (b= −0.11; p = 0.42 for behavioral activation; b= −0.18; p = 0.37 for challenging thoughts).
In the contextual and structural factors meta-regression model, the modalities face-to-face and online were excluded from the analysis because they were significantly correlated with respectively intervention dose (ρ = 0.361; p < 0.05) and online sessions (ρ = −0.693; p < 0.01), and format of the CBT intervention (ρ = −0.420; p < 0.01). In the meta-regression a significant association was found between ‘recipient of the intervention: child and caregiver’ (b= −0.38; p < 0.05) and a larger effect on depression symptoms at follow-up, this association remained significant (b= −0.467; p < 0.05) when analyzed individually in a regression model.
Table 4 Post-treatment outcomes CBT versus passive control.
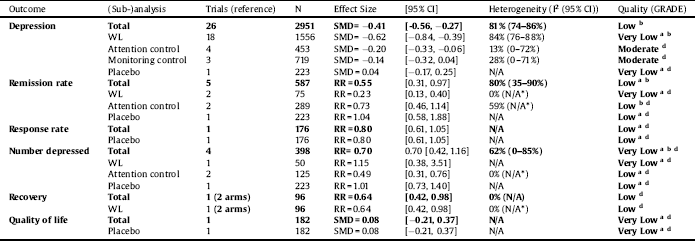
a = Risk of bias, b = Inconsistency, c = Indirectness, d = Imprecision, e = Publication/reporting bias; N/A not applicable; SMD = standardised mean difference; WL = waitlist.
*A minimum number of 3 trials was necessary for the 95% CI calculation of the heterogeneity statistic.
Table 5 Follow-up outcomes CBT versus passive control.

a = Risk of bias, b = Inconsistency, c = Indirectness, d = Imprecision, e = Publication/reporting bias; N/A not applicable; SMD = standardised mean difference; WL = waitlist.
*A minimum number of 3 trials was necessary for the 95% CI calculation of the heterogeneity statistic.
Table 6 Included variables.

4. Discussion
This comprehensive systematic review and meta-analysis (31 studies; 4335 participants) explored the overall effects of CBT interventions on depression in youth and is the first study that focuses on the question of whether certain combinations or lack of CBT components, and contextual and structural factors, can be identified that moderate the effects. Moreover, the specific characteristics of the CBT components were rated on a detailed level so differences between CBT interventions on components could be examined. Our results suggest that CBT is effective for youth in reducing depressive symptoms immediately after the end of treatment (SMD = −0.41) and at follow-up (17–39 weeks; SMD = −0.20). Also, a child/adolescent with subclinical depressive symptoms who receives CBT as indicated prevention has 63% less risk of having a depressive disorder at follow-up. Other results of our analyses showed that after receiving CBT, youth with depression have 45% more chance of being in remission and 36% more chance of recovery compared with control groups, but the quality of the evidence is less robust.
Table 7 Meta-regression analysis intervention components.
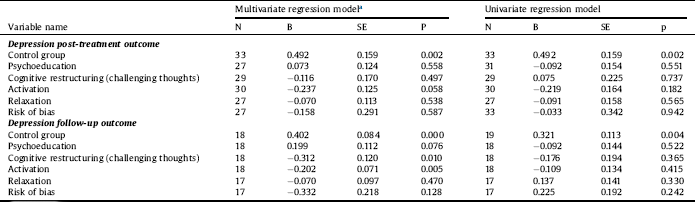
a Measuring variable within a regression model including all variables.
Table 8 Meta-regression analysis contextual and structural factors.

a Measuring variable within a regression model including all variables.
Despite these positive results, effects in terms of symptom reduction are small and have limited clinical importance when CBT (administered as indicated prevention) was compared with monitoring as control condition. Still, our results indicate that there might be room to improve the effects of CBT on the long-term, which is important because the recurrence of depression in youth is high [Reference Curry, Silva, Rohde, Ginsburg, Kratochvil and Simons7]. Results of our meta-regression showed a correlation between improvement on depression outcomes and the combination of the components behavioral activation and challenging thoughts (as part of cognitive restructuring) in a CBT intervention. We also found an association between more favorable treatment outcomes and caregiver(s) involvement in the intervention. Post-hoc sensitivity analysis indicated that this effect was especially beneficial for children younger than 12. For the other two CBT components (psychoeducation and relaxation) and three contextual and structural factors (format of the intervention, setting and intervention dose), no significant correlation with more favorable outcomes were found. Another important variable we included, which was not related to the intervention but to the research, was the quality of the studies (RoB). The quality of the studies did not have a moderating effect in our analysis. This might be due to the fact that we did not take dimensional aspects into account and worked with a cut-off point. As a last point we analyzed post-hoc if moderator effects might be influenced due to the intervention being treatment or indicated prevention. First of all we found only small differences between effects of indicated prevention and treatment on depression symptoms at follow-up. Secondly, when the distribution of moderators was analyzed, only the moderators psycho-education, psychiatric setting and high treatment intensity were significantly more prevalent in treatment trials. As those moderators had no significant influence on the primary outcomes, we concluded that moderating effects were not explained by intervention type (treatment or indicated prevention).
4.1. Our results in relation to other evidence
Recent reviews used inclusion criteria that were more stringent than the inclusion criteria we used in our review, for example regarding specific age groups (only children [Reference Yang, Zhou, Zhou, Zhang, Pu and Liu11, Reference Arnberg and Ost20] or adolescents [Reference Singh and Reece62]), specific types of preventive psychological therapy [Reference Hetrick, Cox, Witt, Bir and Merry10] or a different range of severity of depression. However, our overall results were in line with their outcomes such as non-significant or small effects on depressive symptoms and a decreasing effect as follow-up time progresses. Moderating variables have also been investigated in other research and meta-analyses, with some associations confirming or contradicting our results.
A recent meta-analysis found that the component behavioral activation is effective for young people with depression [Reference Tindall, Mikocka-Walus, McMillan, Wright, Hewitt and Gascoyne63]. This corresponds with another study in which the views of children and adolescents were analyzed. Children and adolescents identified behavioral activation and challenging thoughts as an achievable and effective strategy in reducing depressive symptoms, while 65% of other components of CBT were not judged to be effective [Reference Ng, Eckshtain and Weisz32]. Results of our meta-regression analyses correspond with these results.
With respect to caregiver involvement there are conflicting results between other reviews (and ours). In contrast to our results, one review found that CBT for children (aged 7–13 years) with depression without caregiver involvement was significantly more effective than with caregiver involvement [Reference Yang, Zhou, Zhou, Zhang, Pu and Liu11]. Two other reviews found no differences between involving a caregiver and not involving them when treating youth with depression and/or anxiety with CBT [Reference Spielmans and McFall64] and computerized CBT [Reference Ebert, Zarski, Christensen, Stikkelbroek, Cuijpers and Berking65]. In line with our results, a review focusing on all types of psychotherapy for youth (mean age of 12 (SD = 3.3)) with depression; the authors concluded that caregiver participation was associated with improved treatment outcomes [Reference Dowell and Ogles19]. These differences in effect of caregiver involvement might be explained by the way caregivers were involved. In the field of anxiety disorders, for example, an individual patient data meta-analysis did not find any additional benefit of caregiver involvement in general, but exploratory analyses showed that if CBT focused on contingency management (rewarding desirable behavior and ignoring unwanted behavior) or transfer of control (the process of transferring skills from the therapist to the caregiver) better outcomes were observed at follow-up [Reference Manassis, Lee, Bennett, Zhao, Mendlowitz and Duda66]. In our analysis, there were not enough studies to differentiate between the type of caregiver involvement. However, reviewing the studies with caregiver involvement, we do see differences for example, some interventions were delivered to the caregiver and child/adolescent simultaneously while others were delivered separately. In some interventions contingency management was used, while others did not use this.
Regarding intervention intensity, we did not find an association with an effect on depression symptoms, which is in accordance with Yang et al. [Reference Yang, Zhou, Zhou, Zhang, Pu and Liu11]. In contrast, Arnberg et al. concluded that more sessions (amount of sessions multiplied by the session duration in minutes) leads to a larger effect [Reference Arnberg and Ost20].
Although we did not find positive influence of psychoeducation and could not include goalsetting in our analysis, there is evidence that the combination of these in a brief psychosocial interventions can be as effective as a CBT intervention [Reference Goodyer, Reynolds, Barrett, Byford, Dubicka and Hill67]. So even if our results don’t show the added benefit of a component, it does not mean it does not contribute to an improved effect.
4.2. Strengths and limitations
A specific advantage of our review is that it is the first to investigate the components of different CBT protocols in detail, thereby continuing the work of Fréchette-Simard et al. [Reference Fréchette-Simard, Plante and Bluteau15]. As they suggested, we extracted information directly from the individual intervention protocols, rather than from the articles in which the studies were reported. This approach allowed us to obtain more detailed information about the intervention components. Another strength of our analysis is that the meta-regression gave insight into two CBT components and caregiver involvement being positively associated with improvement of effects of CBT.
Due to our decision to try and limit the heterogeneity that would be caused by active comparison groups (including treatment as usual), our review is limited by the number of studies included. And although we were able to perform a meta-regression analysis, we were limited by the number of variables we could include to keep sufficient statistical power and by the insufficient distribution of the presence or absence of variables between studies. Consequently, we could not include other important CBT components (for example, other elements of cognitive restructuring, positive reinforcement, goalsetting, relapse prevention), and contextual and structural factors (for example, indicated prevention/treatment, age or severity of the depression) in our meta-regression. Two limits to the outcome of the meta-regression should be made. First, The significant moderating effects of CBT components were only indicated in the multivariate regression model. This demonstrates that the activation and challenging thoughts components of CBT are effective as a combination, while there is no evidence for added benefit as stand-alone components. And secondly, recipient of the CBT intervention, which was a significant moderator for the depression outcomes at follow-up, only had one study of the 15 which targeted both children and caregivers. Another limitation is the high number of studies with a small sample size and/or studies at high RoB in the waitlist/no treatment subgroup. These aspects caused inconsistent results and made the depression outcome less robust at post-treatment. This is unfortunate because due to the number of included participants it could have created a precise result, which could have made us more confident of the true effect. Furthermore, we could not obtain some of the original intervention protocols, so we did not have detailed information on all included CBT interventions. Details were also missing about treatment protocol adherence and thereby it is unclear in how many cases the components were truly delivered by the therapist. Finally, there was an underrepresentation of studies conducted in children (k = 5) versus adolescents (k = 25).
4.3. Implications for practice
Based on our findings and other research, CBT that includes behavioral activation and a challenging thoughts component (as part of cognitive restructuring) might improve outcomes for youth in the long-term. However, it is premature to suggest that practice must only apply CBT that includes these two core components. More evidence is needed to provide a causal relationship between these components and improved outcomes.
The results seem to suggest that when treating youth with CBT that the involvement of caregivers might improve depression symptoms on the long term, this might be due to several reasons. First, an etiological factor in the development of depression is the quality of the attachment relationship [Reference Brumariu and Kerns68, Reference Brenning, Soenens, Braet and Bosmans69]. Although CBT does not target improvement of the attachment relationship directly, children learn to increase adaptive coping strategies and caregivers show their commitment by being involved in the intervention. These factors could improve the quality of the attachment relationship and might help to improve outcomes. Second, for children the possibility of transfer of control (caregiver involvement can lead to the transfer of information and skills to the child) might lead to higher intervention fidelity and might make the child more aware of the therapeutic process between the sessions. A meta-analysis of CBT treatment in children has already showed that CBT focused on transfer of control leads to long-term maintenance of treatment gains [Reference Manassis, Lee, Bennett, Zhao, Mendlowitz and Duda66]. Actively involving caregiver(s) in the therapeutic process at the same time by use of contingency management may also lead to improved effects [Reference Manassis, Lee, Bennett, Zhao, Mendlowitz and Duda66]. Furthermore, for the child/adolescent, caregiver involvement might lead to more consistency in their interactions with their therapist, because youth are more inclined to follow the sessions when caregivers are involved [Reference Compton, March, Brent, Albano, Weersing and Curry70, Reference Hardway, Pincus, Gallo and Comer71].
4.4. Directions for future research
The results of our review provides additional evidence and should give an impulse for more research into uncovering the working mechanisms of CBT, which has been strongly recommended to be the next step in improving psychological interventions [Reference Holmes, Ghaderi, Harmer, Ramchandani, Cuijpers and Morrison14]. Therefore, head-to-head RCTs should be undertaken with intervention arms consisting of CBT with and without the intervention components (and a combination of these components), and contextual and structural factors (especially, different types of (non) parental involvement) in order to replicate our results in a ‘real world’ setting. However, when viewing the overall evidence, in general more RCTs should be undertaken to improve the quality of the total evidence, which is currently moderate at best. In particular, it is important to investigate the effects of CBT on children with clinical depression, because this is an under-researched area.
Several aspects could not be analyzed in our meta-analysis. It would be very informative to further investigate the influence of these aspects such as other components and structural characteristics on outcomes. Clinically relevant topics to be investigated are the optimal sequencing and intensity of CBT components during the intervention, and how to improve or sustain long-term outcomes by the application of booster sessions or continuing CBT after remission has started, which has been advised for adults [Reference Bockting, Hollon, Jarrett, Kuyken and Dobson72, Reference Bockting, Smid, Koeter, Spinhoven, Beck and Schene73].
Finally, there have been several attempts to provide evidence on improving the effects of CBT, yet none have been fully successful in separating out the effectiveness of specific CBT components. A possibility for future research is to conduct an individual patient data meta-analysis (IPDMA) because this method can increase power and reliability, as well as enabling an examination of the differential effectiveness of CBT and its components among specific subgroups across studies [Reference Riley, Lambert and Abo-Zaid74]. Most importantly, IPDMA allows for analyzing the predictive value of specific (baseline) characteristics and intervention components [Reference Riley, Lambert and Abo-Zaid74].
Conflict of interest
All other authors have no competing interests. The views of the authors expressed in this paper do not necessarily reflect the views of NCCMH, Royal College of Psychiatrists, Trimbos Institute or NHS England.
Role of funding source
Funding for this study was provided by a grant from ZonMw (Dossier number: 70-72900-98-15101) had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.eurpsy.2018.12.008.














Comments
No Comments have been published for this article.