Impact statement
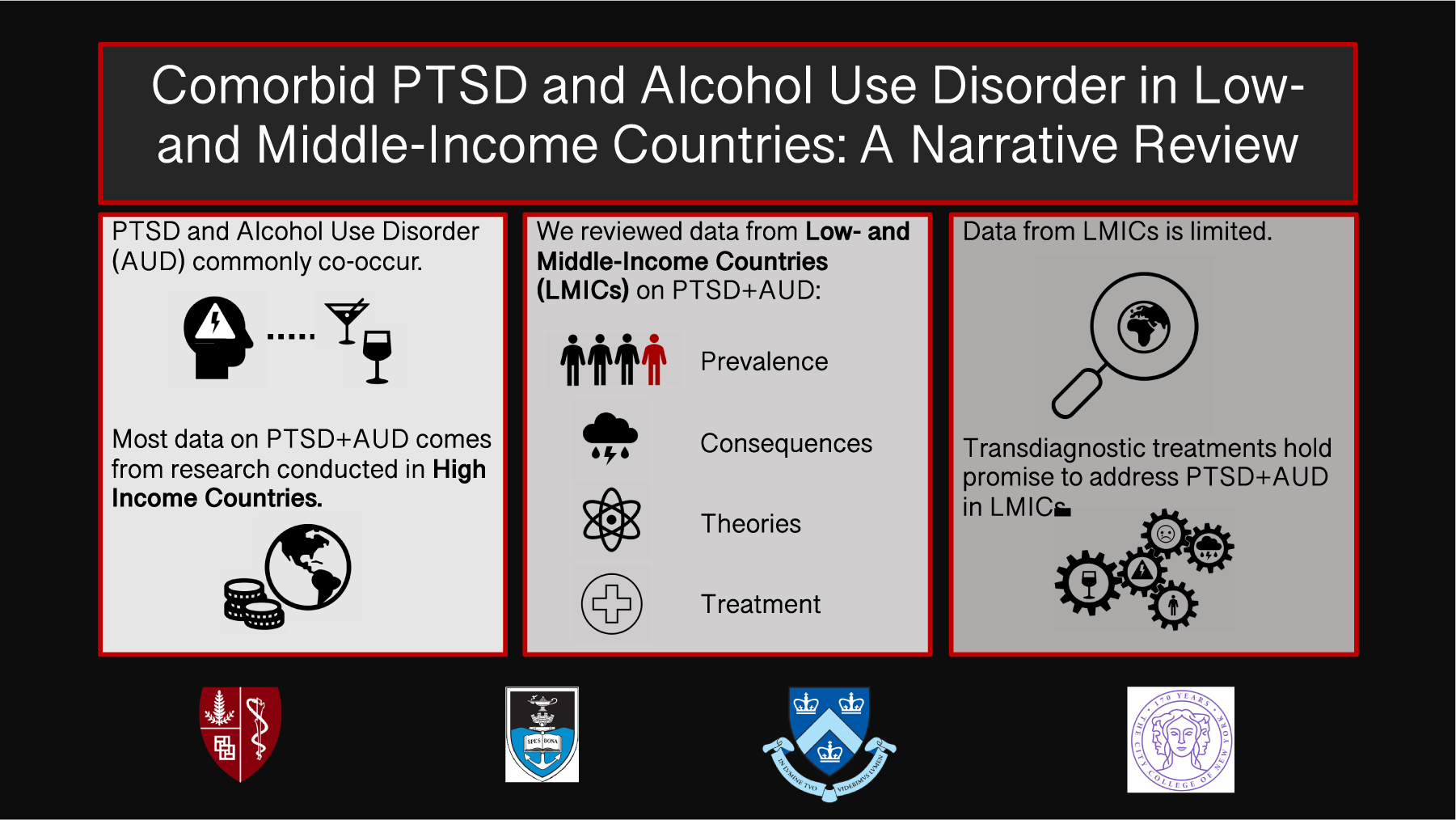
Despite the fact that the majority of the world’s population lives in low- and middle-income countries (LMICs), most of the research on the co-occurrence of posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD) comes from data on samples from high-income countries. This review entailed a targeted examination of the existing literature on the prevalence, consequences, etiology, and treatment of comorbid PTSD + AUD derived from LMICs. Emphasis is placed on a need for more research on the epidemiology, etiology, and treatment of PTSD + AUD in LMICs. It further offers guidance based on the data thus far for how to conduct this research in methodologically sound, resource-sustainable, and culturally relevant ways.
Due to strong, consistent associations between posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD), their co-occurrence (PTSD + AUD) has been a topic of extensive study (Pietrzak et al., Reference Pietrzak, Goldstein, Southwick and Grant2011; Smith and Cottler, Reference Smith and Cottler2018). Data from 42 studies conducted primarily in the USA and other high-income countries (HICs) estimate that 10–61% of people with PTSD also misuse alcohol. Among people with AUD, an estimated 2–63% was found to have co-occurring PTSD (Debell et al., Reference Debell, Fear, Head, Batt-Rawden, Greenberg, Wessely and Goodwin2014). Studies examining variation in the presentation of PTSD + AUD have found that it is generally associated with more severe PTSD symptoms and higher rates of drinking relapse (McCarthy and Petrakis, Reference McCarthy and Petrakis2010; Debell et al., Reference Debell, Fear, Head, Batt-Rawden, Greenberg, Wessely and Goodwin2014; Smith and Cottler, Reference Smith and Cottler2018). However, these findings are largely based on research conducted in HICs, and overall there is a dearth of research on the onset, course, and treatment of comorbid PTSD and AUD in low- and middle-income countries (LMICs; Seedat and Suliman, Reference Seedat, Suliman, Nemeroff and Marmar2018). This is problematic, given that the majority of the world’s population resides in LMICs (Jacob et al., Reference Jacob, Sharan, Mirza, Garrido-Cumbrera, Seedat, Mari, Sreenivas and Saxena2007).
Global burden of PTSD and AUD
Individually, PTSD and AUD present major public health burdens and are associated with high rates of functional impairment. Mental health and substance use disorders (SUDs) are the highest contributors to years lived with disability globally (Whiteford et al., Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari, Erskine, Charlson, Norman, Flaxman, Johns and Burstein2013). Alcohol use is the seventh leading risk factor for all deaths and disability, with 5.1% of the global burden of disease attributable to alcohol use (World Health Organization, 2018; Iranpour and Nakhaee, Reference Iranpour and Nakhaee2019). PTSD affects approximately 4% of the world’s population and is estimated to contribute approximately as much to the global burden of disease as schizophrenia and more than anxiety disorders (Vos and Mathers, Reference Vos and Mathers2000; Ayuso-Mateos, Reference Ayuso-Mateos2002; Benjet et al., Reference Benjet, Bromet, Karam, Kessler, McLaughlin, Ruscio, Shahly, Stein, Petukhova, Hill and Alonso2016).
Despite consistent and robust findings documenting the respective prevalence rates and consequences of PTSD and AUD, available data on PTSD + AUD are limited. The lack of research on PTSD and AUD in LMICs (Seedat and Suliman, Reference Seedat, Suliman, Nemeroff and Marmar2018) presents a major limitation to our understanding of the onset and course of PTSD + AUD globally. Most of the available epidemiological literature on PTSD + AUD is from HICs, with a large proportion focused on military populations and relatively small proportion reporting data from general population surveys (Debell et al., Reference Debell, Fear, Head, Batt-Rawden, Greenberg, Wessely and Goodwin2014; Lo et al., Reference Lo, Patel, Shultz, Ezard and Roberts2017). Studies conducted in the USA have found that individuals with PTSD + AUD demonstrate greater psychiatric impairment, suicidal ideation, and social impairment than those with PTSD alone or AUD alone (Simpson et al., Reference Simpson, Rise, Browne, Lehavot and Kaysen2019), underscoring the need to better understand the onset and course of PTSD + AUD in LMICs in order to address the global burden of disease caused by the comorbidity.
Epidemiology of PTSD and AUD in LMICs
Although the literature from LMICs is limited, the existing evidence suggests that while respective rates of PTSD and AUD appear to be higher in HICs and upper-middle income countries, the burden of harm is greater in LMICs and among those of lower socioeconomic status (Loring, Reference Loring2014; Koenen et al., Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet, Stein, Karam, Ruscio, Benjet, Scott and Atwoli2017). Alcohol consumption is positively associated with country income group, and the unconditional lifetime prevalence of AUD in LMICs (5.9%) is lower than that of HICs (7.2%; Glantz et al., Reference Glantz, Bharat, Degenhardt, Sampson, Scott, Lim, Al-Hamzawi, Alonso, Andrade, Cardoso and De Girolamo2020). However, heavy episodic drinking is highest in LMICs (Parry and Amul, Reference Parry and Amul2022) and low socioeconomic status is associated with increased risk of alcohol-related death (Loring, Reference Loring2014). Similarly, PTSD prevalence ranges from 2.1 to 2.3% in LMICs, compared to 5.0% in HICs (Koenen et al., Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet, Stein, Karam, Ruscio, Benjet, Scott and Atwoli2017). Although trauma exposure risk is higher in LMICs (Atwoli et al., Reference Atwoli, Stein, Koenen and McLaughlin2015), particularly for insidious forms of trauma such as exposure to war zones (Hoppen et al., Reference Hoppen, Priebe, Vetter and Morina2021), treatment seeking for PTSD is more common in HICs (Koenen et al., Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet, Stein, Karam, Ruscio, Benjet, Scott and Atwoli2017) and there are fewer evidence-based treatment options available to individuals living in LMICs (Patel et al., Reference Patel, Chowdhary, Rahman and Verdeli2011).
Rates of AUD and PTSD each vary widely by country (Koenen et al., Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet, Stein, Karam, Ruscio, Benjet, Scott and Atwoli2017; World Health Organization, 2018), highlighting the influence of cultural and socioeconomic factors on prevalence and burden. Moreover, studies of PTSD prevalence in LMIC countries tend to focus on examining rates of PTSD among high-risk populations such as refugees, disaster survivors, conflict-affected populations, or gender-based violence survivors, rather than within the general population (Horyniak et al., Reference Horyniak, Melo, Farrell, Ojeda and Strathdee2016; Lo et al., Reference Lo, Patel, Shultz, Ezard and Roberts2017). Additionally, there is substantial clinical and methodological heterogeneity in the epidemiological studies that have been conducted on PTSD and on AUD, precluding cross-study exploration of risk and protective factors. Some of this heterogeneity is explained by variable approaches to measuring AUD. Existing reviews describe the co-occurrence of PTSD and alcohol misuse, which is used as a term to cover a range of alcohol-related conditions from risky alcohol use behaviors to AUD (Roberts et al., Reference Roberts, Lotzin and Schäfer2022). Additionally, the assessment tools developed in HIC settings used to measure PTSD and AUD are not always adequately validated or adapted for LMIC contexts (Nadkarni et al., Reference Nadkarni, Garber, Costa, Wood, Kumar, MacKinnon, Ibrahim, Velleman, Bhatia, Fernandes and Weobong2019; Mughal et al., Reference Mughal, Devadas, Ardman, Levis, Go and Gaynes2020). Taken together, definitional heterogeneity, the lack of diversity in study populations, and limitations to the cultural appropriateness of standardized assessments of AUD and PTSD make it difficult to determine the extent to which the epidemiological data from HICs generalize to LMICs, where drinking behavior, trauma exposure, and trauma response may vary considerably.
Although some studies in LMICs have examined the impact of AUD or of PTSD separately, literature on the epidemiology and impacts of PTSD + AUD is limited and has produced mixed findings (Lo et al., Reference Lo, Patel, Shultz, Ezard and Roberts2017). In specific, at-risk populations (e.g., those living with HIV), cross-sectional studies have found that PTSD or probable PTSD was significantly associated with current alcohol use, heavy alcohol use, or AUD commonly co-occur (Dévieux et al., Reference Dévieux, Malow, Attonito, Jean-Gilles, Rosenberg, Gaston, Saint-Jean and Deschamps2013; Duko et al., Reference Duko, Toma, Abraham and Kebble2020; Kekibiina et al., Reference Kekibiina, Adong, Fatch, Emenyonu, Marson, Beesiga, Lodi, Muyindike, Kamya, Chamie and McDonell2021). Studies designed to evaluate this comorbidity have identified a significant increase in the likelihood of PTSD + AUD in refugee samples in Uganda (Bapolisi et al., Reference Bapolisi, Song, Kesande, Rukundo and Ashaba2020) and male urban trauma survivors in Sri Lanka (Dorrington et al., Reference Dorrington, Zavos, Ball, McGuffin, Rijsdijk, Siribaddana, Sumathipala and Hotopf2014). This increased risk of PTSD + AUD has also been observed in population-based studies (e.g., in Brazil; de Castro Longo et al., Reference de Castro Longo, Vilete, Figueira, Quintana, Mello, Bressan, de Jesus, Ribeiro, Andreoli and Coutinho2020), with a particularly strong co-occurrence observed in rural settings (Colombia; Gaviria et al., Reference Gaviria, Alarcón, Espinola, Restrepo, Lotero, Berbesi, Sierra, Chaskel, Espinel and Shultz2016). However, one population-based study examining lifetime prevalence of mental disorders by AUD status in Colombia and two studies evaluating harmful alcohol use among internally displaced persons in Georgia and Uganda did not find relationships between PTSD and AUD (Roberts et al., Reference Roberts, Ocaka, Browne, Oyok and Sondorp2011, Reference Roberts, Murphy, Chikovani, Makhashvili, Patel and McKee2014; Rincon-Hoyos et al., Reference Rincon-Hoyos, Castillo and Prada2016). Gender as a risk factor for PTSD + AUD in LMICs may differ from those reported in studies conducted in HICs. For example, one study conducted in refugee camps in Croatia identified increased rates of PTSD + AUD among men, but not women (Kozarić-Kovacić et al., Reference Kozarić-Kovacić, Ljubin and Grappe2000). Similarly, in a study of urban trauma survivors in Sri Lanka, the relationship between PTSD and AUD was only found among men (Dorrington et al., Reference Dorrington, Zavos, Ball, McGuffin, Rijsdijk, Siribaddana, Sumathipala and Hotopf2014). This is in contrast to studies conducted in HICs examining gender differences in PTSD + AUD rates, which have generally found PTSD increases risk of AUD among women more so than among men (Olff et al., Reference Olff, Langeland, Draijer and Gersons2007; O’Hare et al., Reference O’Hare, Sherrer, Yeamen and Cutler2009; Kachadourian et al., Reference Kachadourian, Pilver and Potenza2014).
Differences in the epidemiology of PTSD + AUD may reflect limitations and heterogeneity in the evidence. Approaches to sampling and measurement across these studies vary, which may explain differences in findings. Even in circumstances where there is consistency in measurement, cross-cultural differences may make certain tools less valid in some contexts and populations, introducing further variability. Additionally, much of the literature on PTSD in LMICs focuses on civilian populations affected by humanitarian emergencies where the prevalence of PTSD and common mental disorders is generally higher than that observed in the general population (Charlson et al., Reference Charlson, van Ommeren, Flaxman, Cornett, Whiteford and Saxena2019).
Exposure to potentially traumatic events and norms around alcohol, which are central to the etiology and assessment of PTSD and AUD, respectively, is known to vary across cultures and contexts. Together, differences in the characteristics of various populations, how they are sampled, and the validity and comparability of measurement tools used to assess AUD and PTSD may contribute to high variability in rates of PTSD + AUD observed across studies. In addition, the PTSD diagnostic criteria may not translate cross-culturally, introducing additional heterogeneity across studies (Michalopoulos et al., Reference Michalopoulos, Unick, Haroz, Bass, Murray and Bolton2015). Further research to disentangle this variability is needed to distinguish true differences in the epidemiology of PTSD + AUD from variation that can be explained by methodological limitations of the available literature.
Theoretical models of PTSD + AUD
There are multiple explanatory theories for the association between PTSD and AUD, including the susceptibility model and the self-medication/negative reinforcement model (Haller and Chassin, Reference Haller and Chassin2014). The susceptibility model proposes that alcohol use increases risk of PTSD both through increased exposure to traumatic events and increased vulnerability to develop PTSD. Alcohol intoxication can increase vulnerability to perpetrators of interpersonal trauma and increase likelihood of engaging in risky behavior (Chilcoat and Breslau, Reference Chilcoat and Breslau1998; Jacobsen et al., Reference Jacobsen, Southwick and Kosten2001; Brady et al., Reference Brady, Back and Coffey2004; Schumm and Chard, Reference Schumm and Chard2012; Afzali et al., Reference Afzali, Sunderland, Batterham, Carragher, Calear and Slade2017). Alcohol use appears to increase risk of exposure to traumas such as accidental injury, sexual assault, and violence (Read et al., Reference Read, Wardell and Colder2013; Lorenz and Ullman, Reference Lorenz and Ullman2016; Duke et al., Reference Duke, Smith, Oberleitner, Westphal and McKee2018). Alcohol use may inhibit individuals’ ability to respond to risk cues due to alcohol’s impairing effects on perception (e.g., alcohol myopia; Broach, Reference Broach2004; Griffin et al., Reference Griffin, Umstattd and Usdan2010) or movement and coordination (Valenstein‐Mah et al., Reference Valenstein‐Mah, Larimer, Zoellner and Kaysen2015). After trauma exposure, alcohol use may also increase the likelihood to develop PTSD by inhibiting trauma processing and preventing habituation (Brady et al., Reference Brady, Back and Coffey2004; Back et al., Reference Back, Brady, Sonne and Verduin2006; Balachandran et al., Reference Balachandran, Cohen, Le Foll, Rehm and Hassan2020). For example, alcohol use has been found to prospectively increase risk of PTSD among women who have experienced sexual or physical assault (Kaysen et al., Reference Kaysen, Atkins, Moore, Lindgren, Dillworth and Simpson2011; Read et al., Reference Read, Wardell and Colder2013).
The theory that has received the preponderance of both research and support is the self-medication model (Khantzian, Reference Khantzian1997; Hawn et al., Reference Hawn, Cusack and Amstadter2020). This theory rests on a negative reinforcement paradigm, wherein alcohol is consumed as a means to reduce distress related to the traumatic event or symptoms of PTSD. The short-term reduction in symptoms and distress then serves as a reinforcer for continued alcohol use. Over time, this can lead to independent alcohol use that develops into AUD (Smith and Cottler, Reference Smith and Cottler2018; Hawn et al., Reference Hawn, Cusack and Amstadter2020). In longitudinal studies, trauma exposure and PTSD precede increases in drinking (Boscarino et al., Reference Boscarino, Kirchner, Hoffman, Sartorius and Adams2011; Read et al., Reference Read, Colder, Merrill, Ouimette, White and Swartout2012; Haller and Chassin, Reference Haller and Chassin2014; Lane et al., Reference Lane, Waters and Black2019). In micro-longitudinal studies, such as studies using experience sampling or daily diary designs, which collect a large amount of data typically over moments, days, or weeks, increases in PTSD symptoms precede alcohol use (Sullivan et al., Reference Sullivan, Armeli, Tennen, Weiss and Hansen2020; Dworkin et al., Reference Dworkin, Jaffe, Bedard-Gilligan and Fitzpatrick2021). Taken together, these studies provide support for the self-medication model, highlighting potential mechanisms such as coping-related drinking, emotion regulation, and negative affect (Luciano et al., Reference Luciano, Acuff, Olin, Lewin, Strickland, McDevitt-Murphy and Murphy2022; Weiss et al., Reference Weiss, Brick, Schick, Forkus, Raudales, Contractor and Sullivan2022).
Studies in LMICs have found relationships between alcohol use and increased risk of trauma exposure, although these studies have not tested this in relation to PTSD. For example, alcohol use has been associated with risk of intimate partner violence in several studies conducted in Africa (Shamu et al., Reference Shamu, Abrahams, Temmerman, Musekiwa and Zarowsky2011; Greene et al., Reference Greene, Kane and Tol2017). For relationships between PTSD and alcohol use, most studies presume self-medication as the mechanism of action. In one of the few studies looking at potential mechanisms in a LMIC, in Uganda, alcohol was found to moderate relationships between trauma exposure and PTSD, which was attributed to self-medication (Ertl et al., Reference Ertl, Saile, Neuner and Catani2016). However, overall in LMICs little research has tested these causal models and those that have rely on cross-sectional designs, which preclude examining temporal effects.
The models of PTSD + AUD comorbidity have largely been developed in HIC settings and may not encompass other potential explanatory mechanisms (Shuai et al., Reference Shuai, Anker, Bravo, Kushner and Hogarth2022). Models of broad relevance to LMIC settings may further be limited by the fact that, as previously discussed, prior examinations of PTSD + AUD in LMICs have focused on specific, at-risk groups rather than population-level data. Syndemics theory has been proposed as a helpful framework for understanding PTSD + AUD associations and identifying additional avenues for intervention in some global settings (de Jong et al., Reference de Jong, Berckmoes, Kohrt, Song, Tol and Reis2015). Syndemics theory proposes that intersecting epidemics, such as violence, HIV, and substance use, interact synergistically to compound the burden of disease (Singer et al., Reference Singer, Bulled, Ostrach and Mendenhall2017; Mendenhall et al., Reference Mendenhall, Newfield and Tsai2022). This theory considers the role of harmful social conditions in understanding disease concentration and interaction. In addition, there is a need for research examining ways in which culture, community, and local context may promote resilience, given that PTSD, AUD, and PTSD + AUD are not evenly distributed across communities (Pollack et al., Reference Pollack, Weiss and Trung2016). The lack of research evaluating theories of PTSD + AUD outside of HIC’s is especially problematic, as theories often drive treatment approaches and help to identify target mechanisms for intervention.
Treatment of PTSD + AUD in HICs
Treatment for PTSD + AUD has overwhelmingly been designed in and for HIC settings and has undergone significant shifts over time, influenced by improvements in best practice guidelines for the treatment of each respective disorder and evolutions in conceptualizations of PTSD + AUD itself. The contemporary repertoire of evidence-based AUD care includes cognitive-behavioral treatments (CBTs) such as relapse prevention and mindfulness-based relapse prevention, motivational enhancement therapy, family/couples interventions (e.g., the community reinforcement approach), and pharmacotherapies (e.g., disulfiram, naltrexone, and acamprosate). For PTSD, trauma-focused psychotherapies have garnered the strongest empirical support and are broadly recommended as the front-line interventions (Bisson et al., Reference Bisson, Berliner, Cloitre, Forbes, Jensen, Lewis, Monson, Olff, Pilling, Riggs and Roberts2019; Lewis et al., Reference Lewis, Roberts, Andrew, Starling and Bisson2020). The umbrella term of trauma-focused therapies refers to treatments that involve the direct processing of trauma-related cues, including memories, thoughts, physiological sensations, and external reminders. Prevailing trauma-focused therapies include prolonged exposure, cognitive processing therapy, trauma-focused CBT, and eye movement desensitization and reprocessing (EMDR).
Historically, the dominant philosophy for treating PTSD + AUD advised applying AUD and PTSD treatments sequentially; alcohol-related problems were treated first, aiming to achieve a state of clinical stability (usually defined as a period of alcohol abstinence), and then PTSD was addressed (Back et al., Reference Back, Killeen, Badour, Flanagan, Allan, Santa Ana, Lozano, Korte, Foa and Brady2019). This sequential approach was largely predicated on clinical concerns that prematurely employing trauma-focused therapies would exacerbate AUD symptoms and/or derail recovery gains in non-abstinent individuals (Becker et al., Reference Becker, Zayfert and Anderson2004).
Beginning in the early 2000s, scientific advances in the study of the functional relationship between PTSD and AUD suggested that addressing trauma symptoms could facilitate reductions in alcohol use by reducing the need for coping-related drinking (Coffey et al., Reference Coffey, Saladin, Drobes, Brady, Dansky and Kilpatrick2002). At the same time, a growing interest in non-abstinence outcomes and harm reduction approaches led to the widening of AUD treatment goals to include moderation alongside complete abstinence (U.S. Department of Health and Human Services, 2015). Against this backdrop, a new wave of concurrent treatments emerged that target PTSD + AUD simultaneously. Concurrent approaches either provide stand-alone PTSD and AUD treatments conducted in parallel, or integrated interventions in which PTSD + AUD is treated by the same clinician (e.g., Concurrent Treatment of PTSD and Substance Use Disorders with Prolonged Exposure, Back et al., Reference Back, Killeen, Badour, Flanagan, Allan, Santa Ana, Lozano, Korte, Foa and Brady2019). Clinical trials data of concurrent, trauma-focused PTSD + AUD treatments have consistently shown reductions in PTSD without worsening of AUD (Roberts et al., Reference Roberts, Lotzin and Schäfer2022). Crucially, these studies have suggested that improvements in PTSD also lead to future decreases in AUD symptoms, but that the inverse is much less likely (Hien et al., Reference Hien, Smith, Owens, López-Castro, Ruglass and Papini2018).
Several conventional meta-analyses and systematic reviews including data from HICs now generally point to the superiority of concurrent trauma-focused interventions over sequential treatments or treatments for AUD only, primarily noting reductions in PTSD yet minimal effects on AUD outcomes (van Dam et al., Reference van Dam, Vedel, Ehring and Emmelkamp2012; Simpson et al., Reference Simpson, Goldberg, Louden, Blakey, Hawn, Lott, Browne, Lehavot and Kaysen2021; Roberts et al., Reference Roberts, Lotzin and Schäfer2022). The first meta-analysis of individual-level patient data of comorbid PTSD and SUD treatment trials has offered uniquely expanded and novel insights (Hien, Reference Hien, Morgan-López, Saavedra, Ruglass, Ye, López-Castro, Fitzpatrick, Killeen, Norman, Ebrahimi and Backin press). Applying specialized techniques to address limitations such as measurement and selection biases in summary data integration, the analysis harmonized data from 36 behavioral, pharmacological, and combination treatment studies (n = 4046), compared each intervention to treatment-as-usual, and provided head-to-head comparisons (i.e., comparative efficacy) across treatment types. Treatment types included trauma-focused therapy, integrated behavioral PTSD + AUD treatment, pharmacotherapy for PTSD (e.g., sertraline, paroxetine), pharmacotherapy for SUD (e.g., naltrexone, methadone), and stand-alone behavioral AUD therapy and treatment-as-usual, non-manualized care. Findings suggest that trauma-focused therapies (e.g., prolonged exposure and cognitive processing therapy) when combined with AUD pharmacotherapy (e.g., naltrexone and zonisamide) provide optimally effective care for comorbid PTSD and AUD, showing the largest comparative effect size (CES) against treatment-as-usual (d = −.92 for PTSD, d = −1.10 for alcohol use at end-of-treatment). Findings also highlight the relative efficacy of several other tested approaches. For example, also evidencing large CES were stand-alone trauma-focused interventions (d = −.24 for PTSD, d = −.45 for alcohol use at end-of-treatment), stand-alone pharmacotherapy for AUD (d = −.41 for PTSD, d = −.83 for alcohol use at end-of-treatment), and integrated trauma-focused and AUD behavioral therapies (d = −.47 for PTSD, d = −.42 for alcohol use at end-of-treatment). Improvements in PTSD + AUD symptoms were found for almost all evaluated treatment types, which is consistent with a prior review’s conclusion of “no wrong door” for PTSD + AUD treatment (Simpson et al., Reference Simpson, Goldberg, Louden, Blakey, Hawn, Lott, Browne, Lehavot and Kaysen2021). Because study inclusion required a formal diagnosis of AUD or SUD, relevance of these findings to the treatment of alcohol misuse remains unknown. Critically, all 36 trials included in this meta-analysis were conducted in either the USA, Germany, or Australia, leaving the question of their applicability to LMIC contexts unanswered.
Treatment of PTSD + AUD in LMICs
To our knowledge, no empirical studies have explored the comparative efficacy of concurrent PTSD + AUD treatment approaches in LMICs. Compounding the lack of evidence for these integrated treatment approaches, there is also sparse evidence from LMIC settings for the targeted treatment of alcohol use problems in samples with PTSD or of PTSD in alcohol-using samples. Systematic reviews indicate that trauma-focused CBT, EMDR, and narrative exposure therapy (which embeds exposure-based CBT in an autobiographical narrative) are effective in reducing PTSD in LMIC contexts of mass violence or humanitarian crisis (Morina et al., Reference Morina, Koerssen and Pollet2016; Purgato et al., Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Tol2018). However, the effect of these treatments on concurrent AUD has not been evaluated. Similarly, while there is evidence that AUD treatments such as CBT, motivational interviewing (MI), and structured brief interventions are effective in reducing alcohol use and alcohol-related harm in LMIC settings (Preusse et al., Reference Preusse, Neuner and Ertl2020; Ghosh et al., Reference Ghosh, Singh, Das, Pandit, Das and Sarkar2022; Staton et al., Reference Staton, Vissoci, El-Gabri, Adewumi, Concepcion, Elliott, Evans, Galson, Pate, Reynolds and Sanchez2022), effects on concurrent PTSD have seldom been reported. It is also unclear whether PTSD + AUD acts as a moderator on treatment outcomes. In sum, samples with PTSD and samples with AUD have largely been conceptualized as distinct clinical populations in treatment research in LMICs to date. This is concerning given the increased risk of PTSD + AUD that has been reported in both at-risk and general populations in LMIC settings.
Transdiagnostic approaches
Given high rates of PTSD + AUD globally, another intervention option that has been gaining in popularity is the use of a transdiagnostic therapy approach. Transdiagnostic interventions were developed to address a broad range of commonly comorbid mental and behavioral health problems more effectively and efficiently. This approach differs from concurrent treatment in that it integrates evidence-based therapeutic techniques common to treatments for depression, anxiety, and other mental health problems and aims to address shared mechanisms causing these problems, such as cognitive and behavioral avoidance.
There are at least three reasons a transdiagnostic approach in LMICs may be preferable to traditional concurrent approaches. Transdiagnostic treatments are intrinsically designed to (1) be delivered by a single provider; (2) address additional comorbidities beyond PTSD + AUD; and (3) address a range of symptom severity, such that they do not require a formal diagnosis. The latter strength is especially helpful in a LMIC context where comprehensive assessment and diagnosis may not be feasible (Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary, Haydary, Weiss and Bolton2014; Kane et al., Reference Kane, Vinikoor, Haroz, Al-Yasiri, Bogdanov, Mayeya, Simenda and Murray2018). Two transdiagnostic approaches have been developed and tested in LMICs: the Common Elements Treatment Approach (CETA) and Problem Management Plus (PM+; Dawson et al., Reference Dawson, Bryant, Harper, Tay, Rahman, Schafer and Van Ommeren2015). In both cases, these treatments were not initially designed to address AUD but have since been adapted to do so. Recently, an integrated trauma-focused substance use treatment was also developed in South Africa (Myers et al., Reference Myers, Carney, Browne and Wechsberg2019).
CETA was designed as a multi-problem, flexible transdiagnostic intervention that could be delivered by lay counselors to address a range of mental and behavioral health problems (Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary, Haydary, Weiss and Bolton2014). It was originally designed to focus on common mental health problems of PTSD, depression, anxiety, behavioral issues (for children and adolescents), and impaired relationship and psychosocial functioning. CETA was based on transdiagnostic treatments developed in HICs (Chorpita and Daleiden, Reference Chorpita and Daleiden2009; Farchione et al., Reference Farchione, Fairholme, Ellard, Boisseau, Thompson-Hollands, Carl, Gallagher and Barlow2012; Weisz et al., Reference Weisz, Chorpita, Palinkas, Schoenwald, Miranda, Bearman, Daleiden, Ugueto, Ho, Martin and Gray2012), and treatment components were based on CBTs. Across six LMIC-based randomized-controlled trials (RCTs) of CETA, the treatment has demonstrated robust evidence for treating PTSD among trauma-affected populations (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey, Robinson, Ugueto and Bass2014; Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen, Dorsey, Lindgren, Gross, Murray, Bass and Bolton2015; Bonilla-Escobar et al., Reference Bonilla-Escobar, Fandiño-Losada, Martínez-Buitrago, Santaella-Tenorio, Tobón-García, Muñoz-Morales, Escobar-Roldán, Babcock, Duarte-Davidson, Bass and Murray2018; Murray et al., Reference Murray, Kane, Glass, Skavenski van Wyk, Melendez, Paul, Kmett Danielson, Murray, Mayeya, Simenda and Bolton2020; Bogdanov et al., Reference Bogdanov, Augustinavicius, Bass, Metz, Skavenski, Singh, Moore, Haroz, Kane, Doty and Murray2021; Kane et al., Reference Kane, Sharma, Murray, Chander, Kanguya, Lasater, Skavenski, Paul, Mayeya, Danielson and Chipungu2022).
Bolton et al. (Reference Bolton, Lee, Haroz, Murray, Dorsey, Robinson, Ugueto and Bass2014) first attempted to address co-occurring unhealthy alcohol use and trauma with CETA in a RCT conducted among Burmese refugees in Thailand. This version of CETA added MI aimed at reducing unhealthy alcohol use to the existing intervention. Although the trial demonstrated strong effects of CETA in treating PTSD, there were no impacts on alcohol misuse. Methodological limitations, including the quality of the alcohol screening measure and a small sample size of individuals who reported alcohol misuse, may have contributed to the null findings. However, there was also a concern that MI components were challenging for lay counselors to deliver with fidelity.
Following the Thailand trial, the alcohol/substance use reduction element of CETA was revised as a CBT-based substance use reduction and relapse prevention component (Henggeler et al., Reference Henggeler, Clingempeel, Brondino and Pickrel2002; Danielson et al., Reference Danielson, McCart, Walsh, de Arellano, White and Resnick2012; Kane et al., Reference Kane, Van Wyk, Murray, Bolton, Melendez, Danielson, Chimponda, Munthali and Murray2017). In two recent CETA trials conducted in Zambia, evidence suggested effectiveness of this modified CETA protocol in treating PTSD + AUD. In the first trial, CETA significantly reduced alcohol use among both women and men in families with ongoing interpersonal violence and among whom PTSD was highly prevalent (Murray et al., Reference Murray, Kane, Glass, Skavenski van Wyk, Melendez, Paul, Kmett Danielson, Murray, Mayeya, Simenda and Bolton2020). In the second trial, CETA reduced unhealthy drinking among people living with HIV, and a subgroup analysis in the trial indicated that the effect size for CETA was largest among those who had unhealthy alcohol use and mental health comorbidities, including PTSD (Kane et al., Reference Kane, Sharma, Murray, Chander, Kanguya, Lasater, Skavenski, Paul, Mayeya, Danielson and Chipungu2022).
PM+ was developed by the World Health Organization as a low-intensity intervention, meaning that it was designed to be less time- and resource-consuming when compared to formal, high intensity psychological treatments delivered by mental health professionals and thus increases feasibility and sustainability potential in LMICs (Dawson et al., Reference Dawson, Bryant, Harper, Tay, Rahman, Schafer and Van Ommeren2015). PM+ is a transdiagnostic approach designed to be delivered by lay providers to address a range of common mental health (e.g., depression, anxiety, stress, or grief) and practical problems (e.g., unemployment, interpersonal conflict). Compared to CETA, PM+ has a stronger focus on behavioral, as opposed to cognitive, therapeutic techniques based on the rationale that lay providers would be able to implement behavioral strategies more easily than cognitive interventions. Because it is a less intensive transdiagnostic intervention than CETA, PM+ is considered inappropriate for more severe mental health problems (Dawson et al., Reference Dawson, Bryant, Harper, Tay, Rahman, Schafer and Van Ommeren2015; World Health Organization, 2018). PM+ has been tested in three RCTs in LMICs (Rahman et al., Reference Rahman, Hamdani, Awan, Bryant, Dawson, Khan, Azeemi, Akhtar, Nazir, Chiumento and Sijbrandij2016, Reference Rahman, Khan, Hamdani, Chiumento, Akhtar, Nazir, Nisar, Masood, Din, Khan and Bryant2019; Bryant et al., Reference Bryant, Schafer, Dawson, Anjuri, Mulili, Ndogoni, Koyiet, Sijbrandij, Ulate, Harper Shehadeh and Hadzi-Pavlovic2017). All three trials found effectiveness of PM+ in addressing the stated primary outcomes (i.e., reductions in psychological distress, depression, anxiety). Efficacy outcomes of PM+ on PTSD have varied, and alcohol use was not measured. However, there is currently an effort underway to develop and test an alcohol-specific component to PM+ (PM + A) in trials in Ukraine and Uganda (Fuhr et al., Reference Fuhr, Bogdanov, Tol, Nadkarni and Roberts2021).
In South Africa, Myers et al. (Reference Myers, Carney, Browne and Wechsberg2019) developed a trauma-informed intervention called Women’s Health Coop to address the interrelated problems of substance use, traumatic stress, and sexual risk behaviors in young women from low-income communities. Women’s Health Coop is a 6-session, group-based treatment that integrates feminist empowerment theory and CBT components. A single-arm feasibility study with 60 participants reported significant reductions in alcohol and other substance use, PTSD symptoms, depression symptoms, and sexual risk behaviors at 3 months post-treatment (Myers et al., Reference Myers, Carney, Browne and Wechsberg2019).
Discussion
The aim of the present review was to examine the literature to date on the prevalence, impact, theories of etiology, and treatment approaches to addressing PTSD + AUD in LMICs, which have historically gone underrepresented in PTSD + AUD research. Information on PTSD + AUD prevalence, phenomenology, symptom severity, scope and range of consequent functional impairment, and mechanisms of maintenance in LMICs is currently inconclusive, with limitations stemming from heterogeneity in the evidence derived from various studies, as well as sampling and methodological variation. There appears to be some evidence that both PTSD and AUD occur less frequently in LMICs than HICs, but that symptoms and consequences are more severe when they do occur. The reasons for these findings are not well understood and do not address prevalence or severity rates of PTSD + AUD specifically (Loring, Reference Loring2014; Koenen et al., Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet, Stein, Karam, Ruscio, Benjet, Scott and Atwoli2017). The majority of the literature on PTSD + AUD to date supports a self-medication-based relationship between PTSD symptoms and alcohol use, but there is little research evaluating this theory or culturally informed alternatives in LMICs. Moreover, there is a need for more research that clearly evaluates PTSD + AUD within a societal and cultural context to help elucidate possible differences in risk and protective factors across populations.
The present review also examined the existing literature on treatment, including approaches that address AUD and PTSD individually, approaches that directly address concurrently PTSD + AUD, and transdiagnostic approaches that might address AUD and/or PTSD among other mental and/or behavioral health concerns. PTSD + AUD treatment has largely been examined in HICs, where the evidence base has moved from sequential to concurrent treatment models. However, PTSD and alcohol treatment studies conducted in LMICs are largely siloed, with studies failing to address PTSD + AUD. Though several evidence-based treatments developed in HICs, including intensive trauma-focused therapies, have been successfully implemented in LMICs, there are barriers to broad dissemination and implementation efforts in these settings (i.e., time and resource limitations, the fact that treatments were designed to be implemented by trained specialists rather than lay professionals). Novel interventions being tested in LMICs, such as transdiagnostic treatment approaches that target common mechanisms of psychopathology and can be implemented by a single provider, have potential to provide new avenues for intervention on PTSD + AUD. As of this writing, only CETA has demonstrated efficacy in randomized trials, and other concurrent models have yet to be tested for their effects on PTSD + AUD. Moreover, research on the efficacy of PTSD + AUD treatment delivery by lay professionals in LMICs has potential to expand access to PTSD + AUD care globally, in both LMICs and HICs. Results of this review also highlight that a syndemics approach to alcohol treatment, in which addressing AUD was embedded into a broader public health interventions for other diseases highly relevant to LMIC contexts, such as HIV, shows promise in reducing heavy drinking and related consequences. However, there is a need for studies of these interventions to test whether they also improve PTSD.
One major challenge in understanding relationships between trauma exposure, PTSD, and alcohol misuse is the paucity of data globally, despite evidence that both PTSD and AUD have a large impact on population health that disproportionally affects those in LMICs. This lack of representation means that many of our assumptions as a field regarding how these disorders are interrelated are based on a relatively small and globally non-representative sample. Research examining potential reasons for geographic and cultural variations in symptom presentation and comorbidity may provide the groundwork for development for new prevention and intervention strategies.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2022.63.
Data availability statement
Not applicable to this narrative review.
Acknowledgements
This article was supported by grants from the NIMHD (R01MD011574, PIs: Pearson/Kaysen), NIMH (T32MH019938, PIs: Schatzberg/Manber; K01MH129572, PI: Greene), and NIAAA (K01AA026523, PI: Kane).
Author contributions
Drs. Debra Kaysen was responsible for the conception and design of the this review. All authors contributed to material preparation, literature reviews, and manuscript preparation. All authors read and approved the final manuscript.
Financial support
This work was supported by the National Institute of Mental Health (grant number T32MH019938); the National Institute on Alcohol Abuse and Alcoholism (grant number K01AA026523); and the National Institute on Minority Health and Health Disparities (grant number R01MD011574).
Competing interest
We have no known conflicts of interest to disclose.




Comments
September 1, 2022
Dear Dr. Belkin,
We have uploaded a manuscript entitled, “Comorbid PTSD and Alcohol Use Disorder in Low- and Middle-Income Countries: A Narrative Review” for your review for publication in Global Mental Health.
This manuscript seeks to review the literature to data on the co-occurrence of PTSD and Alcohol Use Disorder in low- and middle-income countries, which have long been neglected in the development of our epidemiological and theoretical understanding of the comorbidity, limiting the development of globally-relevant treatments.
The purpose of this review is to identify current state of the scientific literature on the comorbidity between PTSD and Alcohol Use Disorder stemming from limited investigations of these constructs in Low- and Middle-Income Countries (LMICs) around the world. Discussion and conclusions focus specifically on the limitations in our understanding of comorbid PTSD and Alcohol Use Disorder based on the historic neglect to investigate these constructs in LMICs. Improvement/expansion of our understanding of the global incidence, consequences, and treatment best practices of comorbid PTSD and Alcohol Use Disorder will require the inclusion of more data from LMICs. As part of our review we attempted to include studies using a global lens, rather than focusing on a specific region.
We hope that you will give our manuscript serious consideration for publication in your journal, as we believe it is timely and will make a substantive contribution to an emerging literature on this topic.
Thank you for your consideration of our work and we look forward to hearing from you.
Sincerely,
Debra Kaysen, Ph.D., ABPP
Professor
Department of Psychiatry and Behavioral Sciences
Stanford University
Email: dkaysen@stanford.edu