Recent experience with COVID-19 has reminded us of the importance of scientific progress in enabling pharmaceutical innovation. Fortunately, recent advances in vaccine science accelerated the development of COVID-19 vaccines using novel (e.g., mRNA) and recently established (e.g., viral vectors) technologies. The first-in-kind mRNA vaccines became available in the U.S. in December 2020 (1)—after 500,000 deaths from COVID-19 in the U.S. and 2.5 million deaths globally. However, if the COVID-19 pandemic had occurred 10 years earlier, before these new technologies were ready to be tested, the outcome most likely would have been far worse. Early evidence suggests that COVID-19 vaccines using older technologies such as the inactivated virus have lower efficacy rates (Reference Mallapaty2;Reference Olliaro, Torreele and Vaillant3). The success of novel technologies such as mRNA vaccines built upon multiple prior setbacks (4). Public funding undoubtedly played a major role in supporting the development of these technologies, but so did knowledge gained and shared through their collective successes and failures. This raises the question: could our current success-oriented reward system for pharmaceutical innovation be better designed to promote learning from our collective research and development (R&D) efforts—both successes and failures?
Health technology innovations have played a major role in improving life expectancy and quality of life for humankind (Reference Buxbaum, Chernew, Fendrick and Cutler5;Reference Lichtenberg6). A recent study estimates that pharmaceutical innovations have contributed 35 percent of the 3.3 years of improved life expectancy between 1990 and 2015 in the U.S. (Reference Buxbaum, Chernew, Fendrick and Cutler5). Currently, the field of health economics and outcomes research (HEOR) evaluates the economic value of innovative vaccines and pharmaceuticals mainly in terms of the expected gains in patients’ life expectancy and quality of life, factoring in any cost savings compared to the current standard of care. In other words, the price is established at launch based on these expected gains, with likely follow-up studies identifying if they are realized. But what about the companies that invested in research but failed to have products reach the market? They receive no immediate direct revenue rewards for their efforts, but we all—including their competitors—learn from their efforts. If we only pay for the “winners,” are we devoting enough resources to this global R&D enterprise? On the other hand, do we want to pay for “failures” (e.g., compounds that were advanced into human subjects, but never reached the market, or promising early-stage candidates not put into a phase 1 clinical trial)?
It is well-known that about nine of every ten candidate compounds that enter phase 1 clinical trials fail to reach the market, and our R&D system counters this high risk of failure with rights to high rewards (through the patent/exclusivity system) to incentivize innovation. The question is: does this “blockbuster” approach provide correct incentives for R&D, or should we consider rewarding the “losers” for the knowledge they have generated that benefits everyone (Reference Bountra, Lee and Lezaun7;Reference Chiou, Magazzini, Pammolli and Riccaboni8)?
In this paper, we argue that this important question is not well addressed in the HEOR field and deserves further attention and debate. The general economics literature on the broader economics of innovation (Reference Aghion and Jaravel9;Reference Scotchmer10) tells us that the pharmaceutical development process not only produces innovative drugs, but also information valuable to innovators in the marketplace. In technical terms, these are called knowledge spillovers or knowledge externalities—and have been labelled “scientific spillovers” (Reference Lakdawalla, Doshi, Garrison, Phelps, Basu and Danzon11;Reference Garrison, Kamal-Bahl and Towse12). In general, economists argue that these are positive externalities and will be underproduced relative to socially optimal levels, while negative externalities (e.g., air pollution) will be overproduced, as producers of externalities are not able to (or do not want to) “internalize” (i.e., take into account) these benefits or costs (Reference Dahlman14).
In this paper, we explore whether the existing reward system for pharmaceutical R&D efforts leads to socially optimal level of scientific knowledge generation and sharing, with a particular focus on the value of failures. First, we outline a conceptual approach based on the idea that pharmaceutical R&D efforts produce both medicines and information, and illustrate this with some examples of how failures may generate information beneficial to concurrent and subsequent efforts. Second, we summarize the relatively small literature on the impact of failures on R&D decision making. Third, we discuss whether there are policy approaches that could address shortcomings of the current system that might result in suboptimal R&D and knowledge sharing.
Conceptual Approach
Innovation is a cumulative societal process where innovators learn from prior efforts and adjust their scientific and commercial strategies accordingly (Reference Aghion and Jaravel9;Reference Scotchmer10;Reference Garrison, Mestre-Ferrandiz and Zamora13). For example, Lichtenberg (Reference Lichtenberg6) estimated that about 70 percent of improvements in the 5-year observed survival rates of all cancer sites could be attributed to novel ideas generated 12–24 years earlier. In pharmaceutical R&D, when preclinical research indicates the promise of a novel mechanism of action in treating diseases (e.g., PD-L1 inhibitors in immuno-oncology), innovators evaluate and advance promising compounds into clinical trials. The race to launch the first-in-class compound is a costly and risky competition and one that includes multiple, sequential phases: preclinical, phases 1–3, and phase 4/in-market.
Knowledge is continuously generated through these phases and can be disseminated through patents filed, decisions to move on to the subsequent phases or discontinue, company news announcements and updates, and scientific publications. Upon the completion of each phase, or when deciding to commence a new area of research, an innovator with an ongoing or potential project (called a “focal project”), decides whether to advance to the next phase based on the likelihood of success, the expected payoff in the event of success, and the total costs of development(Reference Dahlman14)(Reference Krieger16). An innovator updates his/her beliefs based on two information sources: (i) private information through their own trials and research and (ii) publicly available information from other research efforts including those of competitors. To maximize expected profit from a project, both scientific and commercial information is considered in this process. In the domain of public knowledge, the information generated by competitors investing in the same target mechanism of action is especially valuable, particularly for a novel mechanism of action with great uncertainty (Reference Magazzini, Pammolli and Riccaboni15;Reference Krieger16). In practice, R&D projects can be discontinued due to a number of reasons including failure to demonstrate incremental efficacy, lack of commercial viability, and setbacks in regulatory approvals (Reference Krieger16;17). Supplementary Table 1 included some examples of discontinued R&D efforts.
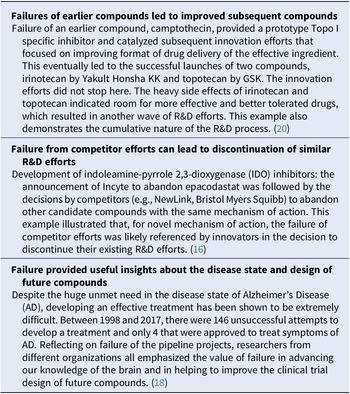
Figure 1 summarizes channels through which knowledge from both successful and failed R&D efforts can “spillover” during the development process. Although the success of a competitor compound could signal the increased likelihood of scientific success, knowledge generated from competitors’ failures could also be equally valuable for the subsequent and/or competing innovators in several ways. The decision to abandon competitive compounds could signal to the innovator that the target mechanism is less likely to succeed, leading to decisions to discontinue the focal project and reallocate resources to other pipeline projects (Reference Chiou, Magazzini, Pammolli and Riccaboni8;Reference Garrison, Mestre-Ferrandiz and Zamora13). On the other hand, reasons behind the failure of competitive compounds could also contain useful information that will allow the innovator to adjust the design of the focal project in the subsequent phases, which could lower the R&D costs and/or increase the likelihood of success for this project, bringing a higher-quality drug to patients in a shorter time period (Reference Krieger19). Table 1 presents some examples that illustrate how failures can benefit subsequent R&D efforts.
Figure 1. Scientific knowledge spillovers: examples from R&D on a novel mechanism of action.
Table 1. Examples of Scientific Knowledge Spillovers from Failed R&D Efforts
In sum, similar to “sinking dry wells” in oil exploration, knowledge generated from failure can improve social welfare as it helps optimize the allocation of R&D resources to more promising projects, lowers the cost of R&D efforts by avoiding the replication of failures, increases the expected payoff, and shortens the time to success for promising compounds.
Findings from Existing Literature
General understanding and appreciation of the scale and influence channels of failed R&D efforts is limited. We conducted a literature search using MEDLINE and IDEAS databases (see Supplementary Tables 2 and 3 for details) on the impact of failed R&D efforts on innovation in the pharmaceutical industry and found empirical evidence showing that failed efforts had a significant impact on the decision making of concurrent and subsequent innovation efforts. Using forward citation of pharmaceutical patents—that is, citations as “prior art” by subsequent patents (essential to securing patent protection)—Chiou et al. (Reference Chiou, Magazzini, Pammolli and Riccaboni8), Magazzini et al. (Reference Garrison, Mestre-Ferrandiz and Zamora13), and Magazzini et al. (18) found that patents of failed R&D efforts were highly cited. Although patents of successful (marketed) products received more forward citations, both failures and successes were more highly cited than those lacking information about the outcomes of preclinical or clinical development. In their model of cumulative innovation, Chiou et al. (Reference Chiou, Magazzini, Pammolli and Riccaboni8) expect failures to be “particularly informative under conditions of high uncertainty among multiple plausible research lines.” Dahlman (Reference Dahlman14) found that the failure of competitors had a significant impact on the decision to exit a project, especially news from compounds with the same target mechanism of action and indicated for the same disease area. However, besides the signaling effect of failed efforts, exactly how failure influenced the decision making of innovators is unclear. It remains challenging to empirically estimate these patterns, partly due to incomplete information and data on the project-level decision-making process (Reference Dahlman14;17;Reference Magazzini, Pammolli, Riccaboni and Rossi20).
Policy Approaches and Implications
Despite the positive societal value of information from failed R&D efforts, information about the reason for failure was typically not consistently disclosed (Reference Chiou, Magazzini, Pammolli and Riccaboni8). Supplementary Table 1 presents six examples of different levels of disclosure from the initial public announcement of companies to discontinue their innovation efforts and follow-on dissemination activities. Possible explanations for the partial disclosure include: (i) the lack of regulatory requirements or their enforcement, (ii) strategic considerations by innovators either to repurpose the failed candidate compounds for other indications or to withhold information from competing researchers (Reference Trajtenberg and Shalem21;Reference Magazzini, Pammolli and Riccaboni22), and (iii) a view that this is information the company generated using its own resources and no one else has a right to it. In existing market structure, the information could be shared via a few private channels including: (i) economies of scope for companies with wide R&D portfolios, internalizing knowledge spillovers as best they can (Reference Magazzini, Pammolli and Riccaboni22); (ii) venture capitalists who invest in multiple biotechnology firms; (iii) mergers and acquisitions; and (iv) research labor mobility (Reference Krieger19). However, these will likely yield incomplete sharing.
How can we incentivize more information-sharing from failed R&D efforts for greater social welfare? In this section, we identify a few market-based and nonmarket-based approaches, discussing advantages, disadvantages, and implementation challenges.
Creating a Market to Trade Failure Information
Given the economic value of information of failed R&D efforts, standard economic theory suggests that a well-designed market trading mechanism could enable interested parties to trade, thereby allowing the externality to be appropriated. As far as we know, no such trading platform currently exists in the marketplace. Trajtenberg and Shalem (Reference Trajtenberg and Shalem21) showed that a market trading mechanism is theoretically feasible in a competitive patent race model under the assumptions of a well-established patent system and a third party to verify the quality of the failure information. However, it could be challenging to implement in practice. Failure is easy to generate: innovators can generate low-quality failure information by exerting less effort, which could be of lower value to potential purchasers. Moreover, it can be difficult to monitor the use of failure information. This is partly because interested parties purchase failure information to avoid it, rather than apply it. The existence of a failure market might also result in less effort by the innovator who anticipates benefitting from failure information generated by other competitors. Although this will improve efficiency in principle, it may lead to aggregate underinvestment. Trajtenberg and Shalem (Reference Trajtenberg and Shalem21) discussed these and other challenges and potential solutions. A standard economic approach will not, however, be easy to implement, and we explore some nonmarket or quasi-market solutions below.
Promoting Open-Science Collaboration
Open-science collaboration models are quasi-market solutions that are being experimented with in multiple countries (Reference Magazzini, Pammolli and Riccaboni22;Reference Henderson and Cockburn23;Reference Chesbrough and Chen28). Chesbrough (Reference Chesbrough and Chen28) described four public–private partnerships in the U.S. and UK where participants can work together to repurpose abandoned compounds, with clarity as to who owns intellectual property (IP) rights and responsibilities to develop and market repurposed drugs. Bountra et al. (Reference Bountra, Lee and Lezaun7) argued that open-science models have the potential to change the paradigm and improve the declining productivity of R&D effort by facilitating “the sharing of data and know-how in the earliest and riskiest stages of the drug discovery process,” reducing duplication of effort. They cite four precompetitive R&D consortia and three open-source initiatives. Notable challenges in implementing this approach include: establishing success metrics, coordinating R&D cost-sharing among participating members, and defining the property rights and an accompanying profit-sharing structure if the compounds succeed. The model that Bountra et al. (Reference Bountra, Lee and Lezaun7) propose “to push the threshold of precompetitive and open-source drug discovery down the development pathway” can, we believe, be better exploited by the use of innovation partnerships that respect IP rights and pool know-how and learnings from successes and failures with drug candidates in phase 1 and, possibly, phase 2. The challenges identified by Krieger (Reference Krieger19) could, however, also arise in this model.
Promoting Public Policies to Incentivize Information-Sharing
In the absence of clear market incentives, government agencies can use both “carrot” and “stick” policy instruments to encourage more complete disclosure of failure information and more collaborative R&D efforts.
Regulatory agencies such as the Food and Drug Administration (FDA) and research funders such as the National Institutes of Health (NIH) can require more consistent and higher quality information disclosure from innovators for failed R&D efforts. This can be especially relevant for R&D projects that have benefited from knowledge generated from publicly funded research in the preclinical stage (Reference Laplane and Mazzucato24;Reference Piller25). Although both the European Medicine Agency (EMA) and the FDA require the trial results of unapproved products to be electronically available in public registries, these requirements have not been strictly enforced and violators have not been publicly identified. Currently, compliance rates with such requirements are low, and the data reports are inconsistent (26;Reference Mazzucato and Li27;Reference Goldacre, DeVito and Heneghan29).
To incentivize more information-sharing of failed R&D efforts through open-science collaboration efforts (discussed above), government could use policy instruments such as providing additional tax incentives for drugs developed via open-science collaboration models, or for innovators who take the effort to publish the trial results (Reference Bountra, Lee and Lezaun7).
Governments could also seek to support a market to trade failure information, perhaps even directly rewarding innovators who share information that has generated significant social value.
Encouraging Academic Publication
Journals and academic institutions can improve information-sharing by encouraging articles, conference presentations, and other forms of dissemination using failed R&D efforts. For example, the Journal of Negative Results in Biomedicine offers an avenue for researchers to distribute failure knowledge that will lead to more success in the future(Reference Magazzini, Pammolli and Riccaboni15).
Increasing Rewards to “Winners”—More Money in the Pot
Increasing the total reward for successful products is one way to stimulate more R&D and compensate for the underinvestment arising from nondisclosure of failure information and from other scientific knowledge spillovers for which the knowledge creator is not compensated. A higher reward will incentivize investment from well-diversified investors in more risky R&D efforts (i.e., those who have a lower probability of success or require more upfront investment costs): hence, more information will be available to share. This broad general subsidy—although administratively simple—could, however, be less efficient than directly compensating knowledge creators.
Future Areas of Research/Limitations
In this article, we argue that scientific knowledge from failed R&D efforts generates valuable information that could benefit concurrent and subsequent innovation efforts. We find that this is an understudied field, with literature suggesting that due to the lack of market incentives and strict enforcement of regulatory requirements, information behind failed attempts is usually only partially disclosed if at all. We discuss several policy instruments—both market-based and nonmarket-based—that could incentivize more information-sharing from failed R&D efforts and improve both returns to investment and social welfare.
Future research should include: (i) exploring the specific channels through which failed R&D efforts affect other innovation efforts—including whether and how failure ultimately leads to more success; (ii) modeling the impact of complete information disclosure on social welfare using a general equilibrium approach, which explicitly models how the different markets (e.g., health and nonhealth sectors) in an economy interact to create a balance in demand and supply in the aggregate; and (iii) comprehensive evaluation of different policy solutions.

Recent experience with COVID-19 has reminded us of the importance of scientific progress in enabling pharmaceutical innovation. Fortunately, recent advances in vaccine science accelerated the development of COVID-19 vaccines using novel (e.g., mRNA) and recently established (e.g., viral vectors) technologies. The first-in-kind mRNA vaccines became available in the U.S. in December 2020 (1)—after 500,000 deaths from COVID-19 in the U.S. and 2.5 million deaths globally. However, if the COVID-19 pandemic had occurred 10 years earlier, before these new technologies were ready to be tested, the outcome most likely would have been far worse. Early evidence suggests that COVID-19 vaccines using older technologies such as the inactivated virus have lower efficacy rates (Reference Mallapaty2;Reference Olliaro, Torreele and Vaillant3). The success of novel technologies such as mRNA vaccines built upon multiple prior setbacks (4). Public funding undoubtedly played a major role in supporting the development of these technologies, but so did knowledge gained and shared through their collective successes and failures. This raises the question: could our current success-oriented reward system for pharmaceutical innovation be better designed to promote learning from our collective research and development (R&D) efforts—both successes and failures?
Health technology innovations have played a major role in improving life expectancy and quality of life for humankind (Reference Buxbaum, Chernew, Fendrick and Cutler5;Reference Lichtenberg6). A recent study estimates that pharmaceutical innovations have contributed 35 percent of the 3.3 years of improved life expectancy between 1990 and 2015 in the U.S. (Reference Buxbaum, Chernew, Fendrick and Cutler5). Currently, the field of health economics and outcomes research (HEOR) evaluates the economic value of innovative vaccines and pharmaceuticals mainly in terms of the expected gains in patients’ life expectancy and quality of life, factoring in any cost savings compared to the current standard of care. In other words, the price is established at launch based on these expected gains, with likely follow-up studies identifying if they are realized. But what about the companies that invested in research but failed to have products reach the market? They receive no immediate direct revenue rewards for their efforts, but we all—including their competitors—learn from their efforts. If we only pay for the “winners,” are we devoting enough resources to this global R&D enterprise? On the other hand, do we want to pay for “failures” (e.g., compounds that were advanced into human subjects, but never reached the market, or promising early-stage candidates not put into a phase 1 clinical trial)?
It is well-known that about nine of every ten candidate compounds that enter phase 1 clinical trials fail to reach the market, and our R&D system counters this high risk of failure with rights to high rewards (through the patent/exclusivity system) to incentivize innovation. The question is: does this “blockbuster” approach provide correct incentives for R&D, or should we consider rewarding the “losers” for the knowledge they have generated that benefits everyone (Reference Bountra, Lee and Lezaun7;Reference Chiou, Magazzini, Pammolli and Riccaboni8)?
In this paper, we argue that this important question is not well addressed in the HEOR field and deserves further attention and debate. The general economics literature on the broader economics of innovation (Reference Aghion and Jaravel9;Reference Scotchmer10) tells us that the pharmaceutical development process not only produces innovative drugs, but also information valuable to innovators in the marketplace. In technical terms, these are called knowledge spillovers or knowledge externalities—and have been labelled “scientific spillovers” (Reference Lakdawalla, Doshi, Garrison, Phelps, Basu and Danzon11;Reference Garrison, Kamal-Bahl and Towse12). In general, economists argue that these are positive externalities and will be underproduced relative to socially optimal levels, while negative externalities (e.g., air pollution) will be overproduced, as producers of externalities are not able to (or do not want to) “internalize” (i.e., take into account) these benefits or costs (Reference Dahlman14).
In this paper, we explore whether the existing reward system for pharmaceutical R&D efforts leads to socially optimal level of scientific knowledge generation and sharing, with a particular focus on the value of failures. First, we outline a conceptual approach based on the idea that pharmaceutical R&D efforts produce both medicines and information, and illustrate this with some examples of how failures may generate information beneficial to concurrent and subsequent efforts. Second, we summarize the relatively small literature on the impact of failures on R&D decision making. Third, we discuss whether there are policy approaches that could address shortcomings of the current system that might result in suboptimal R&D and knowledge sharing.
Conceptual Approach
Innovation is a cumulative societal process where innovators learn from prior efforts and adjust their scientific and commercial strategies accordingly (Reference Aghion and Jaravel9;Reference Scotchmer10;Reference Garrison, Mestre-Ferrandiz and Zamora13). For example, Lichtenberg (Reference Lichtenberg6) estimated that about 70 percent of improvements in the 5-year observed survival rates of all cancer sites could be attributed to novel ideas generated 12–24 years earlier. In pharmaceutical R&D, when preclinical research indicates the promise of a novel mechanism of action in treating diseases (e.g., PD-L1 inhibitors in immuno-oncology), innovators evaluate and advance promising compounds into clinical trials. The race to launch the first-in-class compound is a costly and risky competition and one that includes multiple, sequential phases: preclinical, phases 1–3, and phase 4/in-market.
Knowledge is continuously generated through these phases and can be disseminated through patents filed, decisions to move on to the subsequent phases or discontinue, company news announcements and updates, and scientific publications. Upon the completion of each phase, or when deciding to commence a new area of research, an innovator with an ongoing or potential project (called a “focal project”), decides whether to advance to the next phase based on the likelihood of success, the expected payoff in the event of success, and the total costs of development(Reference Dahlman14)(Reference Krieger16). An innovator updates his/her beliefs based on two information sources: (i) private information through their own trials and research and (ii) publicly available information from other research efforts including those of competitors. To maximize expected profit from a project, both scientific and commercial information is considered in this process. In the domain of public knowledge, the information generated by competitors investing in the same target mechanism of action is especially valuable, particularly for a novel mechanism of action with great uncertainty (Reference Magazzini, Pammolli and Riccaboni15;Reference Krieger16). In practice, R&D projects can be discontinued due to a number of reasons including failure to demonstrate incremental efficacy, lack of commercial viability, and setbacks in regulatory approvals (Reference Krieger16;17). Supplementary Table 1 included some examples of discontinued R&D efforts.
Figure 1 summarizes channels through which knowledge from both successful and failed R&D efforts can “spillover” during the development process. Although the success of a competitor compound could signal the increased likelihood of scientific success, knowledge generated from competitors’ failures could also be equally valuable for the subsequent and/or competing innovators in several ways. The decision to abandon competitive compounds could signal to the innovator that the target mechanism is less likely to succeed, leading to decisions to discontinue the focal project and reallocate resources to other pipeline projects (Reference Chiou, Magazzini, Pammolli and Riccaboni8;Reference Garrison, Mestre-Ferrandiz and Zamora13). On the other hand, reasons behind the failure of competitive compounds could also contain useful information that will allow the innovator to adjust the design of the focal project in the subsequent phases, which could lower the R&D costs and/or increase the likelihood of success for this project, bringing a higher-quality drug to patients in a shorter time period (Reference Krieger19). Table 1 presents some examples that illustrate how failures can benefit subsequent R&D efforts.
Figure 1. Scientific knowledge spillovers: examples from R&D on a novel mechanism of action.
Table 1. Examples of Scientific Knowledge Spillovers from Failed R&D Efforts
In sum, similar to “sinking dry wells” in oil exploration, knowledge generated from failure can improve social welfare as it helps optimize the allocation of R&D resources to more promising projects, lowers the cost of R&D efforts by avoiding the replication of failures, increases the expected payoff, and shortens the time to success for promising compounds.
Findings from Existing Literature
General understanding and appreciation of the scale and influence channels of failed R&D efforts is limited. We conducted a literature search using MEDLINE and IDEAS databases (see Supplementary Tables 2 and 3 for details) on the impact of failed R&D efforts on innovation in the pharmaceutical industry and found empirical evidence showing that failed efforts had a significant impact on the decision making of concurrent and subsequent innovation efforts. Using forward citation of pharmaceutical patents—that is, citations as “prior art” by subsequent patents (essential to securing patent protection)—Chiou et al. (Reference Chiou, Magazzini, Pammolli and Riccaboni8), Magazzini et al. (Reference Garrison, Mestre-Ferrandiz and Zamora13), and Magazzini et al. (18) found that patents of failed R&D efforts were highly cited. Although patents of successful (marketed) products received more forward citations, both failures and successes were more highly cited than those lacking information about the outcomes of preclinical or clinical development. In their model of cumulative innovation, Chiou et al. (Reference Chiou, Magazzini, Pammolli and Riccaboni8) expect failures to be “particularly informative under conditions of high uncertainty among multiple plausible research lines.” Dahlman (Reference Dahlman14) found that the failure of competitors had a significant impact on the decision to exit a project, especially news from compounds with the same target mechanism of action and indicated for the same disease area. However, besides the signaling effect of failed efforts, exactly how failure influenced the decision making of innovators is unclear. It remains challenging to empirically estimate these patterns, partly due to incomplete information and data on the project-level decision-making process (Reference Dahlman14;17;Reference Magazzini, Pammolli, Riccaboni and Rossi20).
Policy Approaches and Implications
Despite the positive societal value of information from failed R&D efforts, information about the reason for failure was typically not consistently disclosed (Reference Chiou, Magazzini, Pammolli and Riccaboni8). Supplementary Table 1 presents six examples of different levels of disclosure from the initial public announcement of companies to discontinue their innovation efforts and follow-on dissemination activities. Possible explanations for the partial disclosure include: (i) the lack of regulatory requirements or their enforcement, (ii) strategic considerations by innovators either to repurpose the failed candidate compounds for other indications or to withhold information from competing researchers (Reference Trajtenberg and Shalem21;Reference Magazzini, Pammolli and Riccaboni22), and (iii) a view that this is information the company generated using its own resources and no one else has a right to it. In existing market structure, the information could be shared via a few private channels including: (i) economies of scope for companies with wide R&D portfolios, internalizing knowledge spillovers as best they can (Reference Magazzini, Pammolli and Riccaboni22); (ii) venture capitalists who invest in multiple biotechnology firms; (iii) mergers and acquisitions; and (iv) research labor mobility (Reference Krieger19). However, these will likely yield incomplete sharing.
How can we incentivize more information-sharing from failed R&D efforts for greater social welfare? In this section, we identify a few market-based and nonmarket-based approaches, discussing advantages, disadvantages, and implementation challenges.
Creating a Market to Trade Failure Information
Given the economic value of information of failed R&D efforts, standard economic theory suggests that a well-designed market trading mechanism could enable interested parties to trade, thereby allowing the externality to be appropriated. As far as we know, no such trading platform currently exists in the marketplace. Trajtenberg and Shalem (Reference Trajtenberg and Shalem21) showed that a market trading mechanism is theoretically feasible in a competitive patent race model under the assumptions of a well-established patent system and a third party to verify the quality of the failure information. However, it could be challenging to implement in practice. Failure is easy to generate: innovators can generate low-quality failure information by exerting less effort, which could be of lower value to potential purchasers. Moreover, it can be difficult to monitor the use of failure information. This is partly because interested parties purchase failure information to avoid it, rather than apply it. The existence of a failure market might also result in less effort by the innovator who anticipates benefitting from failure information generated by other competitors. Although this will improve efficiency in principle, it may lead to aggregate underinvestment. Trajtenberg and Shalem (Reference Trajtenberg and Shalem21) discussed these and other challenges and potential solutions. A standard economic approach will not, however, be easy to implement, and we explore some nonmarket or quasi-market solutions below.
Promoting Open-Science Collaboration
Open-science collaboration models are quasi-market solutions that are being experimented with in multiple countries (Reference Magazzini, Pammolli and Riccaboni22;Reference Henderson and Cockburn23;Reference Chesbrough and Chen28). Chesbrough (Reference Chesbrough and Chen28) described four public–private partnerships in the U.S. and UK where participants can work together to repurpose abandoned compounds, with clarity as to who owns intellectual property (IP) rights and responsibilities to develop and market repurposed drugs. Bountra et al. (Reference Bountra, Lee and Lezaun7) argued that open-science models have the potential to change the paradigm and improve the declining productivity of R&D effort by facilitating “the sharing of data and know-how in the earliest and riskiest stages of the drug discovery process,” reducing duplication of effort. They cite four precompetitive R&D consortia and three open-source initiatives. Notable challenges in implementing this approach include: establishing success metrics, coordinating R&D cost-sharing among participating members, and defining the property rights and an accompanying profit-sharing structure if the compounds succeed. The model that Bountra et al. (Reference Bountra, Lee and Lezaun7) propose “to push the threshold of precompetitive and open-source drug discovery down the development pathway” can, we believe, be better exploited by the use of innovation partnerships that respect IP rights and pool know-how and learnings from successes and failures with drug candidates in phase 1 and, possibly, phase 2. The challenges identified by Krieger (Reference Krieger19) could, however, also arise in this model.
Promoting Public Policies to Incentivize Information-Sharing
In the absence of clear market incentives, government agencies can use both “carrot” and “stick” policy instruments to encourage more complete disclosure of failure information and more collaborative R&D efforts.
Regulatory agencies such as the Food and Drug Administration (FDA) and research funders such as the National Institutes of Health (NIH) can require more consistent and higher quality information disclosure from innovators for failed R&D efforts. This can be especially relevant for R&D projects that have benefited from knowledge generated from publicly funded research in the preclinical stage (Reference Laplane and Mazzucato24;Reference Piller25). Although both the European Medicine Agency (EMA) and the FDA require the trial results of unapproved products to be electronically available in public registries, these requirements have not been strictly enforced and violators have not been publicly identified. Currently, compliance rates with such requirements are low, and the data reports are inconsistent (26;Reference Mazzucato and Li27;Reference Goldacre, DeVito and Heneghan29).
To incentivize more information-sharing of failed R&D efforts through open-science collaboration efforts (discussed above), government could use policy instruments such as providing additional tax incentives for drugs developed via open-science collaboration models, or for innovators who take the effort to publish the trial results (Reference Bountra, Lee and Lezaun7).
Governments could also seek to support a market to trade failure information, perhaps even directly rewarding innovators who share information that has generated significant social value.
Encouraging Academic Publication
Journals and academic institutions can improve information-sharing by encouraging articles, conference presentations, and other forms of dissemination using failed R&D efforts. For example, the Journal of Negative Results in Biomedicine offers an avenue for researchers to distribute failure knowledge that will lead to more success in the future(Reference Magazzini, Pammolli and Riccaboni15).
Increasing Rewards to “Winners”—More Money in the Pot
Increasing the total reward for successful products is one way to stimulate more R&D and compensate for the underinvestment arising from nondisclosure of failure information and from other scientific knowledge spillovers for which the knowledge creator is not compensated. A higher reward will incentivize investment from well-diversified investors in more risky R&D efforts (i.e., those who have a lower probability of success or require more upfront investment costs): hence, more information will be available to share. This broad general subsidy—although administratively simple—could, however, be less efficient than directly compensating knowledge creators.
Future Areas of Research/Limitations
In this article, we argue that scientific knowledge from failed R&D efforts generates valuable information that could benefit concurrent and subsequent innovation efforts. We find that this is an understudied field, with literature suggesting that due to the lack of market incentives and strict enforcement of regulatory requirements, information behind failed attempts is usually only partially disclosed if at all. We discuss several policy instruments—both market-based and nonmarket-based—that could incentivize more information-sharing from failed R&D efforts and improve both returns to investment and social welfare.
Future research should include: (i) exploring the specific channels through which failed R&D efforts affect other innovation efforts—including whether and how failure ultimately leads to more success; (ii) modeling the impact of complete information disclosure on social welfare using a general equilibrium approach, which explicitly models how the different markets (e.g., health and nonhealth sectors) in an economy interact to create a balance in demand and supply in the aggregate; and (iii) comprehensive evaluation of different policy solutions.
Disclosures
R.Z.X. holds the position of HEOR Manager at the Innovation and Value Initiative (IVI), a 501(c)(3) nonprofit research organization whose members include pharmaceutical companies, patient advocacy organizations, and health systems. A.T. has a part-time contract of employment with the Office of Health Economics (OHE), a UK not-for-profit and registered charity and Independent Research Organization. L.P.G. is Professor Emeritus in The Comparative Health Outcomes, Policy, and Economics (CHOICE) Institute in the School of Pharmacy at University of Washington. L.P.G. and A.T. are independent consultants who have received financial support from IVI for their contribution to this research. This specific project was supported by funding from the Innovation and Value Initiative. A.T. and L.P.G. have also received consulting and speaking fees from a number of pharmaceutical companies and nonprofit entities unrelated to this work.
Funding Statement
This project was supported by the Innovation and Value Initiative (IVI).
Conflicts of Interest
Richard Z. Xie is an employee of IVI and an author of this article. The co-authors received comments from IVI colleagues on earlier drafts, but they have the final word on the content of the manuscript.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/S0266462322000150.