Introduction
The statement “There is no health without mental health” is widely credited to Dr David Satcher, former US Surgeon General, made in the context of the landmark 1999 report from his office on the unmet mental health needs of the US population [1]. This statement reflects the multiple, intrinsic linkages between mental and physical health. Mental disorders and psychological distress are associated with increased burden of medical morbidity, including hypertension, diabetes, obesity, cardiovascular disease, and HIV/AIDS, and predict poor prognosis and premature death from these conditions [Reference Kelly, Boggs and Conley2–Reference Chang, Hayes and Perera5]. Health behaviors, including tobacco and alcohol use, poor diet, and physical inactivity, limited access to high-quality medical care, and the disconnect between the general medical and specialty mental healthcare sectors, contribute to this burden as well [Reference Katon and Unützer6,Reference Pincus, Houtsinger, Bachman and Keyser7].
The Substance Abuse and Mental Health Services Administration has sought to address the gap in clinical training necessary for successful integration of behavioral health and primary care through its Primary and Behavioral Health Care Integration Program [8]. However, there are few parallel programs to address training needs in the scientific research workforce. This lack of training impairs both scientific progress and clinical care. For example, in the proceedings from a 2014 international conference cosponsored by NIDDK and NIMH, leading scientists working on the intersection of depression and diabetes noted (emphasis added):
“Many researchers and practitioners currently work in single disease fields. It is critical that training moves to account for the complexity of multiple comorbid diseases that are the norm for real-world patients…. As in many fields, scientific advancement is stunted without a cadre of researchers that can span the translational chasms between the basic, applied, and population sciences [Reference Holt, de Groot, Lucki, Hunter, Sartorius and Golden9].”
While this quote was addressing the relationships between depression and diabetes specifically, this need for interdisciplinary and translational methodologic training applies across most mental and physical health conditions.
Because of the standard independent approaches to training and research in mental and physical health, knowledge gained in one area of science takes longer to inform research on other outcomes (e.g., inflammation is now thought to play a role in the etiopathology of both cardiometabolic disorders [Reference Björntorp and Rosmond10] and of depression [Reference Pearlman and Greenberg11]). Instead, findings from these parallel, rather than intersecting, lines of research present an incomplete picture of the role of shared risk factors (e.g., inflammation) as determinants of overall health and health disparities.
Situating the Intersection of Mental and Physical Health Within an Equity Framework
Numerous studies of the academic workforce have documented the underrepresentation of ethnic and racial minorities (URM) in all areas of higher education [Reference Rodriguez, Campbell, Fogarty and Williams12–Reference Guevara, Adanga, Avakame and Carthon14]. Despite recent commitments to address this gap [Reference Lewis15], university faculty in the health sciences are unlikely to ever reach parity representation of URM scholars without significant investments [Reference Matias, Lewis and Hope16]. There is no single solution to address this concern, however, lack of progression to promotion/tenure status is a major force behind the underrepresentation of racial/ethnic minority researchers in the National Institutes of Health (NIH) portfolio [Reference Valantine and Collins17,Reference Valantine, Lund and Gammie18]. One of the pivotal factors in retaining URM early-career researchers is the development of effective mentoring partnerships with senior investigators [Reference Mezuk, Tarraf, Johnson-Lawrence, Ilardo, Lichtenberg and Jackson19]. Mentoring is an essential tool for professional development in the academy [Reference Guise, Geller, Regensteiner, Raymond and Nagel20–Reference Byars-Winston and Dahlberg22], particularly for URM trainees who often acutely feel a sense of “impostor syndrome” early in their careers [Reference Vaa Stelling, Andersen and Suarez23,Reference Atkins, Dougan, Dromgold-Sermen, Potter, Sathy and Panter24].
Rationale for the Michigan Integrative Well-Being and Inequality (MIWI) Training Program
Disparities do not emerge solely at the level of individual behaviors; rather, they originate at the intersection of environmental, psychosocial, and biological contexts [Reference Mezuk, Concha, Perrin and Green25–Reference Braveman27]. However, few investigators have the skills needed to pose and test innovative hypotheses about this intersection, particularly among marginalized groups [Reference Valantine and Collins17,Reference Jones, Sauma and Bernard28]. The result is an incomplete, and potentially inaccurate, understanding of the drivers of health inequities [Reference Green and Darity29,Reference Mezuk, Del Toro and Gough Courtney30].
As illustrated by Fig. 1, training on integrative approaches to health and well-being should seek to meet two training objectives: The first objective is to provide a breadth of training resources on the methodological skills and analytic tools necessary to conduct interdisciplinary integrative health research. This objective involves providing training, consultation, and logistical support in both innovative approaches to study design, data collection, and data analysis, and best practices in rigor and reproducibility, including preregistration of data collection and analysis protocols, statistical coding and documentation, and data sharing [Reference Brito, Li and Moore31–Reference Christensen, Freese and Miguel33]. The second objective is to embed collaborative, interdisciplinary team science into research practice through a mentored, applied case-based training framework. Team science is a form of cooperative learning [Reference Faupel-Badger, Vogel, Austin and Rutter34,Reference Lindsell, Gatto and Dear35] in which scientists communicate with each other and work together in pursuit of a common objective, albeit from different points of emphasis. Interdisciplinary science, on the other hand, can be conceptualized as a form of methodological competition [Reference Tebes and Thai36–Reference Smaldino and O’Connor38] where each scientist brings their own methodological orientation and strengths, and through discussion and debate, the most promising approaches are selected to address a question. Collectively, interdisciplinary team science is a forum for best practices in rigor and reproducibility [Reference Guise, Geller, Regensteiner, Raymond and Nagel20].

Figure 1. Embedding rigor, reproducibility, and robustness in community-centered integrative health research through training on conceptual models, study designs, and analytic approaches.
To achieve these broad educational objectives, the MIWI Training Program aimed to attract three types of early-career researchers: Behavioral/social scientists studying mental health who are interested in learning how to incorporate and analyze biological/clinical measures; Clinical/health services researchers interested in learning how to assess mental disorders and related behavioral/psychological constructs; and Minority health researchers who want to employ a more comprehensive approach to studying health. These scientists have distinct training needs, but also bring unique foundational expertise to their research programs, as shown in Table 1.
Table 1. Conceptual framework of learner needs in integrative approaches to health research

Aims of This Program Evaluation
The goals of this paper are to describe the core design elements of the MIWI Training Program and to conduct a process evaluation of the first cohort of 15 trainees (called “Scholars”) to complete this program. We hope these insights can inform NIH efforts to train early-career scientists, particularly from underrepresented groups, working at the intersection of multiple disciplines and efforts to support the formation of research networks.
Methods and Materials
Structure and Components of the MIWI Training Program
Fig. 2 provides an overview of the 12-months of activities – before, during, and after the summer institute – which comprise the MIWI Training Program. These include (1) pre-institute orientation activities, (2) training and mentorship activities during the institute including (a) didactic sessions and (b) interactive small workgroups, and (3) matching scholars with resources and mentorship teams, including ongoing remote contact over the 9-months following the institute.
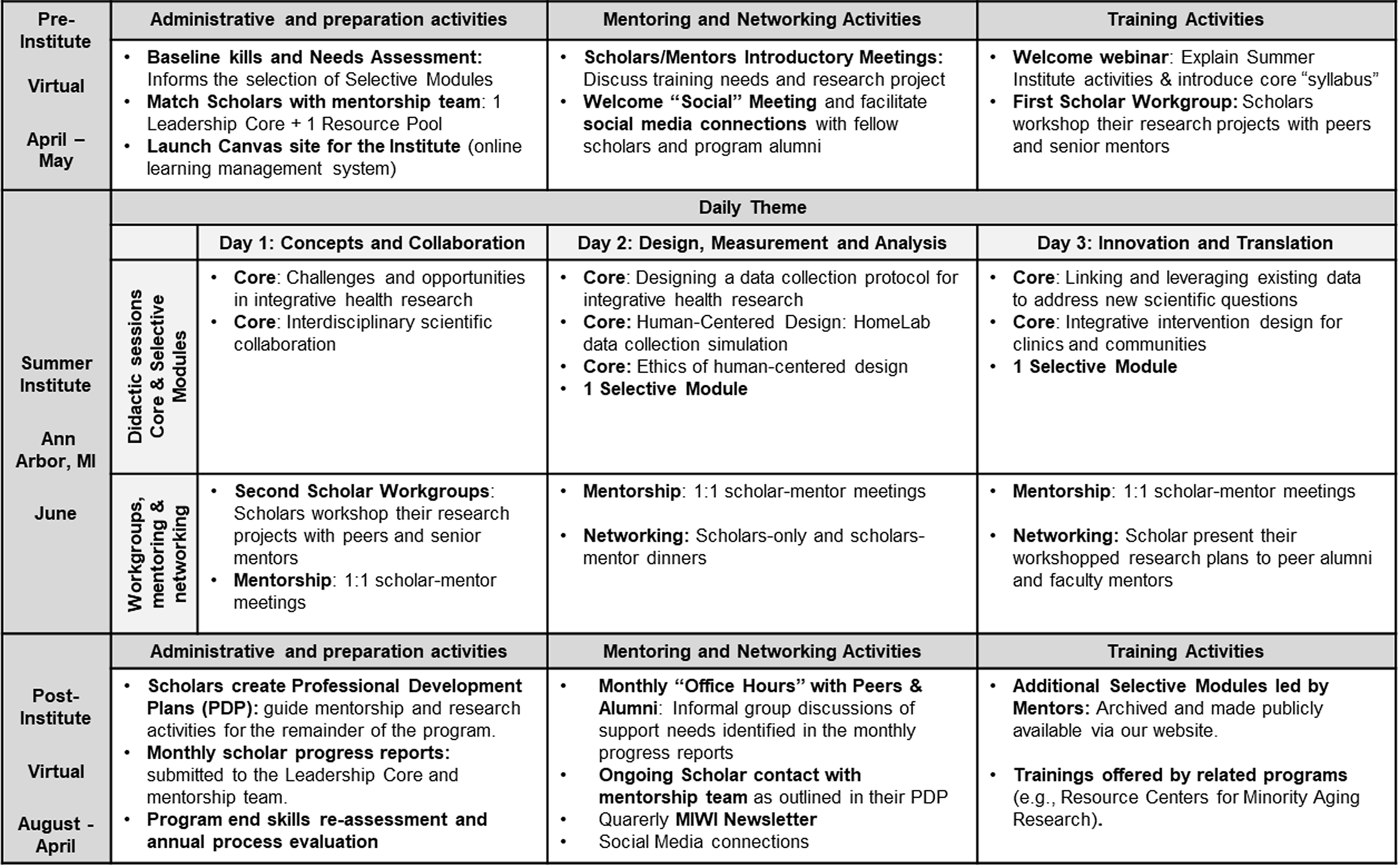
Figure 2. Annual components of the Michigan Integrative Well-Being and Inequality (MIWI) Training Program.
Didactic training sessions: The schedule and content of the Summer Institute were organized into themes: Day 1: Concepts and Collaboration, Day 2: Design, Measurement, and Analysis, and Day 3: Innovation and Translation. For each didactic session, we employ interactive, applied pedagogical approaches that draw on real-world case examples, which reflect pedagogical best practices for engaging adult learners [Reference Newman and Peile39]. The didactic sessions consist of Core Modules that are offered every year and which address issues we believe are central to the training needs of all three types of trainees (Table 1) including human-centered design, leveraging existing datasets, interdisciplinary scientific collaboration, collection of biological data, and responsible conduct of research. We also offer an array of Selective Modules, which address important skills (e.g., mixed methods, social network analysis, data science) but which cannot be comprehensively addressed in the time allowed. Our goal of offering the Selective Modules is to illustrate how these methods can inform research on the intersection of mental and physical health, engage our network of mentors in training, and provide flexibility to match the programing to the distinct interests of each cohort.
Small workgroups: All Scholars submitted a brief (2-page) research proposal as part of their application process; this document formed the basis for their small workgroup discussions. These workgroups, which lasted approximately 3 hours long, each consisted of 3–5 Scholars and their MIWI mentor teams. During the workgroups, each Scholar presents their research project for 10–15 minutes, which is followed by 30 minutes of group discussion. These discussions are framed by both the research proposal and the training needs of the Scholar. At the end of each Scholar’s time, the Scholar identifies 3–5 major challenges and an action plan for addressing them (e.g., rework their hypotheses, connect with a data resource). This mode of training is derived from principles of adult learning, which emphasize the importance of concrete, rather than abstract, applications of knowledge [Reference Ng, Cullum, Cheung and Friedman40].
Scholars went through this process twice during their time in the training program. For our first cohort, both small workgroups were held a day apart during the summer institute (which was entirely virtual due to COVID-19, as described below); currently, we conduct one workgroup virtually a few weeks before the institute and a second during the residential institute to give the Scholars more time to process the feedback they receive.
Resource pool and mentorship teams: The final component of MIWI is focused on mentorship. We recruited a cohort of highly-skilled, internationally-recognized scholars from across the country to serve in our mentor “Resource Pool.” The purpose of the Resource Pool is to provide a broad network of committed senior mentors (e.g., indicated by history of serving as a primary mentor to F- or K-awardees or involvement in training programs such as T32, R25, director of education programs, etc.) for Scholars. All Scholars were assigned a two-member mentorship team, one of which is a MIWI director/co-director, and the other is from the Resource Pool. The latter was matched based on the Scholar’s self-identified training needs and interests, as expressed in their application. Our goal is to provide matches that maximize common interests so that the secondary mentor will be able to augment the Scholar’s training experience with their own expertise. This is one of the core ways that MIWI responds to the training needs of interdisciplinary and URM investigators, who often report limited access to effective mentoring relationships and insufficient contact with senior scholars in their fields [Reference Smaldino and O’Connor38,Reference Newman and Peile39]. Employing a team-mentor approach is an effective way to support both the scientific and professional development needs of interdisciplinary scholars.
Scholars and Mentors were introduced prior to the summer institute, worked together in the small workgroups during the institute, and continued meeting after the institute as outlined in the Scholars’ Professional Development Plan (PDP). The PDP is created by the Scholar, in consultation with the mentorship team, and has three components: (1) overarching goals for their time in MIWI, (2) planned actions with a timeline, and (3) self-identified support needs. Goals typically reflect a mix of research milestones (e.g., submitting a grant) and skills development (e.g., learning network analysis). Each goal is then broken down into a timeline with an action plan of specific tasks that need to be accomplished to meet their goal. Finally, scholars reflect on their support needs for accomplishing their overarching goals, such as anticipated challenges and resources they may need. The PDP becomes “active” in August, approximately two months after the institute, and serves as a guide for interactions between the Scholars and their mentorship team for the following 9-months.
Progress on the PDP is monitored by Mentors MIWI program leadership by having Scholars submit monthly progress reports from September to the following April, when the program concludes. Mentors help Scholars develop their research skills, reflect on the feedback they received on their research projects in the workgroups, discuss issues related to navigating the academy, and support scientific collaboration. These types of “informal” interactions are an important element of many NIH-funded training programs [Reference Beech, Calles-Escandon, Hairston, Langdon, Latham-Sadler and Bell13,Reference Margherio, Horner-Devine, Mizumori and Yen41].
Process Evaluation: Data Sources
We used both quantitative and qualitative approaches for conducting this process evaluation, which focuses on the experience of our first cohort of 15 Scholars. These Scholars, applied in January/February 2020, were informed of their selection in early March 2020, participated in the summer institute in June 2020, and completed their formal engagement with the program in April 2021. As a process evaluation of an education program, this study was exempt from human subjects regulation.
Application materials and biographical data. Accepted Scholars were asked to report their race as part of the program admission process. We abstracted information regarding career stage (e.g., current position and institution, years since terminal degree) and disciplinary background (e.g., field of terminal degree) from curriculum vitae submitted as part of the application. We characterized the research projects that Scholars’ proposed in their application according to four dimensions: overall approach (i.e., quantitative, qualitative, or mixed methods), scientific orientation (i.e., hypothesis testing or hypothesis generating), data source (i.e., primary data collection, secondary data analysis, or a mix of both), and study design (i.e., observational or intervention/experimental).
Qualitative reflections on program experiences and processes. Scholars were asked to reflect on their experience via free-text responses to prompts (e.g., “What are the first five words that come to mind when thinking of your experience in MIWI?”). These reflections were collected using a web survey (i.e., Google form) three times: immediately post-institute, at the end of the 12-month program, and 24 months after program acceptance. The program director and coordinator also conducted informal “listening sessions” (via Zoom) with Scholars a few months after the institute to understand aspects of program implementation, including communication, learning systems technology, and experiences with various aspects of the program.
Quantitative skill assessments. We assessed Scholars’ methodological skill needs (pre-institute, April 2020) and skill growth (and the end of the program, April 2021) using a web survey. Skill needs assessments were conducted approximately 1 month before they attend the summer institute and again at the program conclusion. The survey assessed skills across six domains: conceptual/theoretical models, study design, data/analysis, competence working with marginalized groups, interdisciplinary team science, and broader professional development. The post-program survey asked Scholars to rate “To what degree has participating in MIWI improved your comfort level with…” and each item was assessed on a five-point scale ranging from one=No improvement to five=Greatly improved. The pre-program needs assessment asked for a smaller set of items in a related manner; this needs assessment instrument has been expanded over time, and not all items were assessed at this initial timepoint.
Metrics of connections among the cohort. On the post-program survey, we asked Scholars to what degree their participation in the program helped facilitate new collaborations. Scholars were asked to what degree their MIWI mentorship helped them (a) broaden and (b) diversify their professional network; the same two questions were then asked in reference to their fellow peer Scholars. Each of these four questions was scored on a five-point scale, ranging from one=Not at all to five=To a great degree. We then directly asked whether they had initiated any new scientific collaborations with fellow Scholars, with response options: one=Yes and it has produced an abstract/paper/grant/other product; two=Yes, but our collaborations has not yet produced a product; three=No, but I hope to start a collaboration in the next 3 months; and four=No, and I have no plans to start a collaboration.
We also used publicly-available data sources, including social network platforms (e.g., LinkedIn, Twitter), publication databases (e.g., Google Scholar, ORCIDs), and grant databases (e.g., NIH reporter) to identify connections and research collaborations among the cohort of 15 Scholars. We supplemented this data with annual web surveys of Scholars regarding research activities (e.g. presentations, grants submitted, papers in press) that are challenging to identify from these publicly-available sources. We created a relational database of elements to describe these connections (e.g., connections on LinkedIn, coauthored publications) among the cohort through March 2023.
Analysis
Descriptive statistics were used to characterize the cohort, including their career stage, disciplinary background, and research project. Self-evaluated skills were quantified using mean scores post-program and change since pre-institute where possible. Word clouds, in which the size of the word is proportional to its frequency, were used to visualize Scholars’ qualitative reflections on their experiences in the program. Finally, we created a graphical representation of the network of the cohort, in which each Scholar is a vertex (node) and the connections between them are illustrated by lines (edges) [Reference Barnes and Harary42]. The edges were estimated from a partial correlation matrix from the database of connection elements. In this network, the linear weight of each edge indicates the strength of the connection between the scholars, with the thinnest lines indicating weak connections (e.g., following each other on Twitter) and the thickest lines indicating research collaborations (e.g., coauthoring a paper(s)).
All descriptive analyses were conducted in STATA (v16). The network analysis was conducted using packages dplyr and igraph in R Version 2022.12.0 + 353.
Results
Recruitment, eligibility, and selection of trainees. Our first recruitment effort began in January 2020 through various social media and professional listservs. This included professional societies such as the Gerontological Society of America, the American Public Health Society, and the American Psychosomatic Society, among many others; the national networks of the Resource Centers for Minority Aging Research, Diabetes Translational Research Centers, among many others; and through the listserves of the Program for Research on Black Americans, the Spirit of 1848, and related special-interest networks. We also worked to get our recruitment flyer included on the Twitter and/or LinkedIn feeds of these organizations and in the newsletter of the NIH Office of Behavioral and Social Science Research.
To be eligible for the program, applicants needed to hold a doctoral degree (PhD, MD, etc.), and have demonstrated experience in health and/or health disparities research as evidenced by peer-reviewed scientific publications and/or participation in research grants. Complete applications consisted of three components: (1) a curriculum vitae, (2) a candidate statement describing their program of research and training needs, and (3) a two-page research prospectus that included specific aims and a description of the general approach or methodology used to address those aims. Applications were submitted via the program website: https://sph.umich.edu/mental-physical-health-training/.
We received 57 applications from across the US (24 states) and three international locations. Applicants held doctoral degrees in a wide range of fields, most commonly psychology, social work, and nursing. Nearly 60% of applicants completed their terminal degree within the last three years. We developed a rubric, modeled on NIH grant review criteria, to evaluate the applicants in terms of significance of research, evidence of productivity relative to career stage, and match between self-identified training needs and our program elements. Each applicant was independently reviewed by two raters (i.e., program directors and coordinator). Beyond the qualifications of each individual applicant, the program leadership also considered the overall composition of the cohort in terms of diversity of disciplines, overlapping research interests, career stage (i.e., postdoctoral fellow vs. early-career faculty), and methodological orientation (i.e., primarily qualitative vs. primarily quantitative). These application materials were also used to inform the creation of each Scholar’s mentorship team, as described above.
Characteristics of the First Cohort of MIWI Scholars
All 15 of the applicants who were invited to join the program were accepted, and even when the institute moved to fully remote, they all continued to participate. Table 2 describes the characteristics of this initial cohort. Nearly half (53%) identified as an URM, the majority were female, and most were within 2 years of completing their terminal degree. Most (73%) were from a social/behavioral science discipline, although there was substantial variation within that category and within the types of methods used in their research, as illustrated by the abstracted elements of their research prospectuses.
Table 2. Characteristics of the first cohort of MIWI scholars (n = 15, 2020–2021)

* All Scholars in this initial cohort proposed research projects directly relevant to either minority health or health disparities. Therefore, in this table and in Fig. 4 we categorize them using only their primary disciplinary background rather than according to the learner framework outlined in Table 1.
Process Evaluation
Fig. 3 illustrates the qualitative reflections of Scholars’ experiences of the program immediately after the virtual institute, at the end of the 12-month training period, and two years after they started the program. Across all three time periods, the most commonly-cited word is supportive, with terms such as community and collaborat[ive] also prominent. Table 3 summarizes the self-assessed skills of Scholars at the end of training period, with mean pre-institute values for those skills assessed at that time. Scholars reported skill growth in collecting and analyzing biological data and working as part of an interdisciplinary team, and high comfort in being an interdisciplinary scientist at the conclusion of the program. The lack of improvement in the skill of “Collaborate with community partners” may reflect the relatively high skill in this area that this cohort of scholars had pre-program (mean score: 3.27 out of 5).

Figure 3. Qualitative evaluation of cohort 1 experiences in the MIWI Training Program (2020–2022).
Word clouds created from anonymous responses from Scholars to the prompt “What are the first five words that come to mind when thinking of your experience in MIWI?” Panel A: Immediately following the virtual institute in June 2020 (n=15); Panel B: At program conclusion in April 2021 (n=15); Panel C: Two years after program acceptance in April 2022 (n=7).
Table 3. Skills development over the 12-month training period for cohort 1 (n = 15, 2020–2021)

Values are mean (SD) scores at the conclusion of the 12-month program period (April 2021) and at the pre-program needs assessment (April 2020).
Post-program items asked “To what degree has participating in MIWI improved your comfort level with…” each assessed on a 5-point scale ranging from 1=No improvement to 5=Greatly improved.
Pre-program/Needs assessment items asked “What is your comfort level with…” each assessed on a 5-point scale ranging from 1 = I am uncomfortable with this to 5 = I am very comfortable with his and could lead a class on it.
The needs assessment and program evaluation instruments have been expanded over time, and now all domains are assessed both pre- and post-institute.
Network Building
In the Spring 2021 post-program survey, Scholars reported that their MIWI mentorship team helped them broaden (mean = 4.0 on five-point Likert scale, SD = 1.2) and diversify (mean = 3.67, SD = 1.1) their professional networks; they also reported that their fellow peer Scholars helped them broaden (mean = 3.74, SD = 1.2) and diversify (mean = 3.8, SD = 1.1) their networks. All Scholars reported either wanting to or having already initiated a collaboration with fellow Scholars, including four (26.7%) that reported that their collaboration had already resulted in a conference abstract, paper, or grant. Fig. 4 illustrates the professional network among the Scholars through March 2023. The network illustrates (a) most Scholars are connected informally through social media, (b) scholars from clinical (blue boxes) and social/behavioral (yellow circles) disciplines are integrated into the network, and (c) there are several strong connections (i.e., the thickest edges indicate collaborative publications and/or grants) between Scholars from clinical and social/behavioral disciplines. We also note that none of the Cohort 1 Scholars had published with each other prior to 2020; we are unable to determine the date of social media connections using publicly-available data.

Figure 4. Network connections between Cohort 1 Scholars (through March 2023).
Edges are defined by via a summation of weighted attribute connections (1) Twitter or Linked-in, (2) Collaborative presentation, (3) Collaborative publication, and (4) Collaborative grant submission. The thicker the line, the more “collaborative” the connection between two individuals.
Discussion
In the first year of the MIWI Training Program, which coincided with the onset of the COVID-19 pandemic, we successfully launched a state-of-the-art, integrative methods training program, which attracted a diverse range of early-career scientists from across the US. We have learned how to effectively use virtual technology to maximize pedagogical flexibility while promoting meaningful trainee interactions. Scholars’ report gains in skills relevant to conducting integrative health research, including collecting biological data and working in interdisciplinary teams. Finally, these findings suggest that MIWI is seeding productive, interdisciplinary connections among Scholars.
While our program evaluation is ongoing, our experience with this first cohort of Scholars identified several strengths and opportunities for improvement. Strengths included the ability to create meaningful connections despite distance. The qualitative and network results are particularly striking given that they emerged during a time of intense social and economic disruption, characterized both by the pandemic and increased attention to police brutality, which disproportionately impacted minority groups in the US [Reference Williams and Cooper43,Reference Kiang and Tsai44]. Opportunities for improvement include the need to foster development of skills that Scholars can directly apply to their own research projects. The small workgroups are potentially useful vehicles for Scholars to apply the lessons from the didactic training in their own research, but that transfer of knowledge likely takes time to bear fruit [Reference Schwinn45]. In addition, we sought to ensure greater representation of Scholars from the clinical/health services disciplines, and our more recent cohorts reflect success in achieving this representation. We have used evaluations of specific didactic sessions to revise the offerings of core and selective modules during the summer institute in a manner that is responsive to trainee needs and interests. Finally, as part of our ongoing process evaluation, we continually identify training areas that require additional sessions (e.g., training on analysis of large data), as well as areas that are already strengths among each cohort, and refine the didactic offerings accordingly.
MIWI Scholars are conducting work relevant to the intersection of mental and physical health, with attention to how that intersection relates to minority health and/or health disparities; indeed, applicants who proposed research projects that solely focused on either mental health (e.g., stress as a risk factor for depression) or physical health (e.g., greenspace as a protective factor for diabetes) would not score highly in our review process. Instead, applicants that propose projects such as stress as a risk factor for diabetes or how factors related to the built environment shape depression risk are ideal candidates. Even if projects are not situated within a health equity framework [Reference Braveman27], as neither stress nor access to greenspace are randomly distributed in the population, these principles are relevant. MIWI is intentional about helping Scholars consider how those structural factors impact the framing of their scientific questions and/or the implications of their findings.
Learning How to Maximize Hybrid Training Programs
Even before COVID, MIWI was designed to be a hybrid training program that involved two components: a residential summer institute, followed by 9-months of ongoing team mentorship, professional development, and remote learning opportunities. However, as the pandemic unfolded, it became clear that holding the summer institute in Ann Arbor, Michigan in June 2020 was not an option. We decided that, rather than canceling our first year, we would host the inaugural summer institute entirely online. This required us to consider both the learning needs of our trainees and how to accommodate the challenges of their competing demands, including caregiving responsibilities and emotional stress from the pandemic and other social and political events of the summer.
Our pivot to a remote institute allowed us to identify how technology can enhance training programs in ways that we had not considered. Zoom meetings are now a regular part of work-life, but this was not the case in spring of 2020 when we made the decision to move the institute online. We worked to retain the essential structure of the institute in this new format: each day consisted of a mix of didactic seminars, small workgroup sessions to apply learning, and opportunities for mentor-scholar interactions. This began by asking Scholars about their technology resources (e.g., access to a webcam) and experience using a range of virtual communication programs in the needs assessment. We redesigned the seminars to involve a combination of asynchronous and synchronous components (e.g., readings, additional resources) to combat “Zoom fatigue.” We worked with institute faculty to ensure the didactic sessions were interactive (e.g., each hour-long session included 25–30 minutes for discussion). In addition to Zoom, we made use of two other technologies: The classroom management web platform Canvas, where we housed all learning materials (i.e., recorded seminars, and readings), and the communication platform Slack to facilitate informal, streamline communication between scholars. Having the institute in Canvas allowed us to easily transfer materials to future years, and to monitor which parts of the site Scholars use most frequently. For Slack, our institute workspace began with three channels (i.e., topics of discussion) focused on logistics and resource-sharing; the workspace remains active and now consists of 14 channels, most of them created by Scholars themselves (e.g., #writingtime, #resume-advice). We add new Scholars to it each year (versus developing a separate Slack workspace annually) to facilitate cross-cohort conversations. Collectively, these tools enhance the learning, resource-sharing, and network-building activities of the program and have allowed us to enhance the remote portion of our planned hybrid model in ways we had not anticipated.
Broadening the Reach of the MIWI Training Program
NIH strongly advocates that educational programs implement “Train the Trainer” models [46] to broaden the impact of these efforts. Beginning with the 2022 cohort, MIWI launched an Alumni Peer Mentor program with the goal of both broadening the reach of our training as well as facilitating ongoing learning of Scholars. Once Scholars complete this program, if they have met a threshold of seniority (e.g., receiving tenure or another leadership position) and demonstrated a commitment to mentoring, they can join MIWI as a Mentor. In addition, we use social media (@MIWI_Training) and recently launched a YouTube channel for disseminating relevant conferences, grant opportunities, calls for papers, and sharing news about Scholars and Mentors. We continue to develop the program website as a repository for evidence-based best practices, data sources, and links to related sites to support capacity building in the field.
Conclusion
This is an opportune time for strengthening methodological skills in integrative health research. Our understanding of the neurophysiologic correlates of psychosocial factors has increased substantially in the past two decades [Reference Miller, Chen and Cole47,Reference McEwen48]. Evidence is growing that many interventions originally pioneered for addressing psychosocial aspects of health (e.g., peer support for mental illness [Reference Castelein, Bruggeman, Davidson and van der Gaag49]) are also effective for a range of medical conditions including diabetes [Reference Fisher, Boothroyd and Elstad50] and cancer [Reference Delisle, Gumuchian and Kloda51]. Finally, the COVID pandemic has simultaneously demonstrated the necessity for interdisciplinary team science and lowered the (technological) barriers for such collaborations [Reference Adams, Light and Theis52].
A 2007 editorial in the Lancet argued: “The burden of mental disorders is likely to have been underestimated because of inadequate appreciation of the connectedness between mental illness and other health conditions [Reference Prince, Patel and Saxena53].” The MIWI Training Program fills a workforce developing gap to directly address these interactions, in a manner that is attentive to the fact that disease burden is not equally distributed across social groups.
Acknowledgments
We would like to thank Max Ansorge for their help preparing the tables for this manuscript, and Nebi Girma, Annalise Lane, and Abbi Crowder for their administrative support of the program. Finally, we are grateful for the mentorship and inspiration of our founding co-Director, Dr James S. Jackson (1940 – 2020), who contributed to the selection and mentorship of this first cohort of Scholars.
Funding statement
The MIWI Training Program is supported by the National Center for Complementary and Integrated Health (NICCH; R25-AT010664 to B. Mezuk).
Competing interests
The authors have no conflicts of interest to declare.









