Introduction
Carcinoid tumours commonly arise from the digestive tract, bronchi and lungs, but rarely from the middle ear.Reference Sahan, Yildirim, Arslanoğlu, Karslioğlu and Kazikdasş1 Middle-ear carcinoid tumours are now considered potentially malignant based on some reports of regional nodal involvement and distant metastasis.Reference Fundakowski, Chapman and Thomas2,Reference Salzman, Stárek, Tichá, Skálová and Kučera3 In particular, patients with local relapses occurring a long time after the first surgery are likely to experience nodal involvement, suggesting that long-term observation is necessary.Reference Salzman, Stárek, Tichá, Skálová and Kučera3
Here, we report a case of middle-ear carcinoid tumour that metastasised to the parapharyngeal space and the parotid gland 20 years after the initial surgery. To the best of our knowledge, this is the first report of metastasis to the parapharyngeal space.
Our report highlights the need for attention to be paid to the parapharyngeal space on computed tomography (CT) scans in patients with middle-ear malignant tumours, associated with the lymphatic drainage of the middle-ear mucosa towards the parapharyngeal space. Because of difficulties in performing fine-needle aspiration to lesions in the parapharyngeal space, detailed medical history-taking and magnetic resonance imaging (MRI) are recommended to distinguish carcinoid tumour metastasis from benign tumours, such as neurinoma and low-grade malignant parotid tumours with metastasis.
Case report
A 35-year-old woman with a history of multiple surgical procedures for middle-ear tumours was referred to our hospital with tumours in the parapharyngeal space and the parotid gland on the right side.
At the age of 15 years, she underwent the first stage of tympanoplasty because of the suspicion of a benign tumour located in the middle ear. An intra-operative rapid pathological diagnostic examination suggested a benign tumour; however, the pathological examination indicated carcinoid tumour.
After a year, a whitish tumour recurred and extended from the facial recess to the antrum, as observed in the second stage of tympanoplasty. The intra-operative rapid pathological diagnosis was carcinoid tumour; therefore, mastoidectomy with canal wall down was performed following complete removal of the tumour, and the ossicular chain was finally reconstructed. Subsequently, regular follow-up CT was undertaken twice a year.
Local relapse was suspected on CT four years after the second surgery. During surgery, it was observed that the middle ear was filled with the tumour, extending anteriorly to the Eustachian tube and posteroinferiorly to the tympanic sinus. Removal of the posterior, inferior and anterior walls of the external ear canal exposed the whole tumour, which was completely resected with a stapes superstructure. However, early local relapse around the cochlea was detected during the planned tympanoplasty within six months. The tumour, which extended close to the jugular bulb and carotid canal, was resected by carefully drilling the temporal bone extensively. As a result of early planned surgery, no local recurrence has occurred since then.
After 15 years, unexpectedly, a regular CT scan revealed a well-circumscribed tumour with a diameter of 17 mm in the parapharyngeal space and multiple smooth-marginated tumours in the parotid gland (Figure 1). T1-weighted and T2-weighted MRI scans showed isointense and heterogeneous hypointense signals in these tumours. These elastic, hard tumours, with good mobility, did not cause pain or facial palsy. The fine-needle aspiration specimen of the parotid tumour was insufficient for a definitive diagnosis, necessitating an open biopsy. Based on the above findings, metastatic recurrence of carcinoid tumour or low-malignant parotid tumour with metastasis to the parapharyngeal space was suspected.
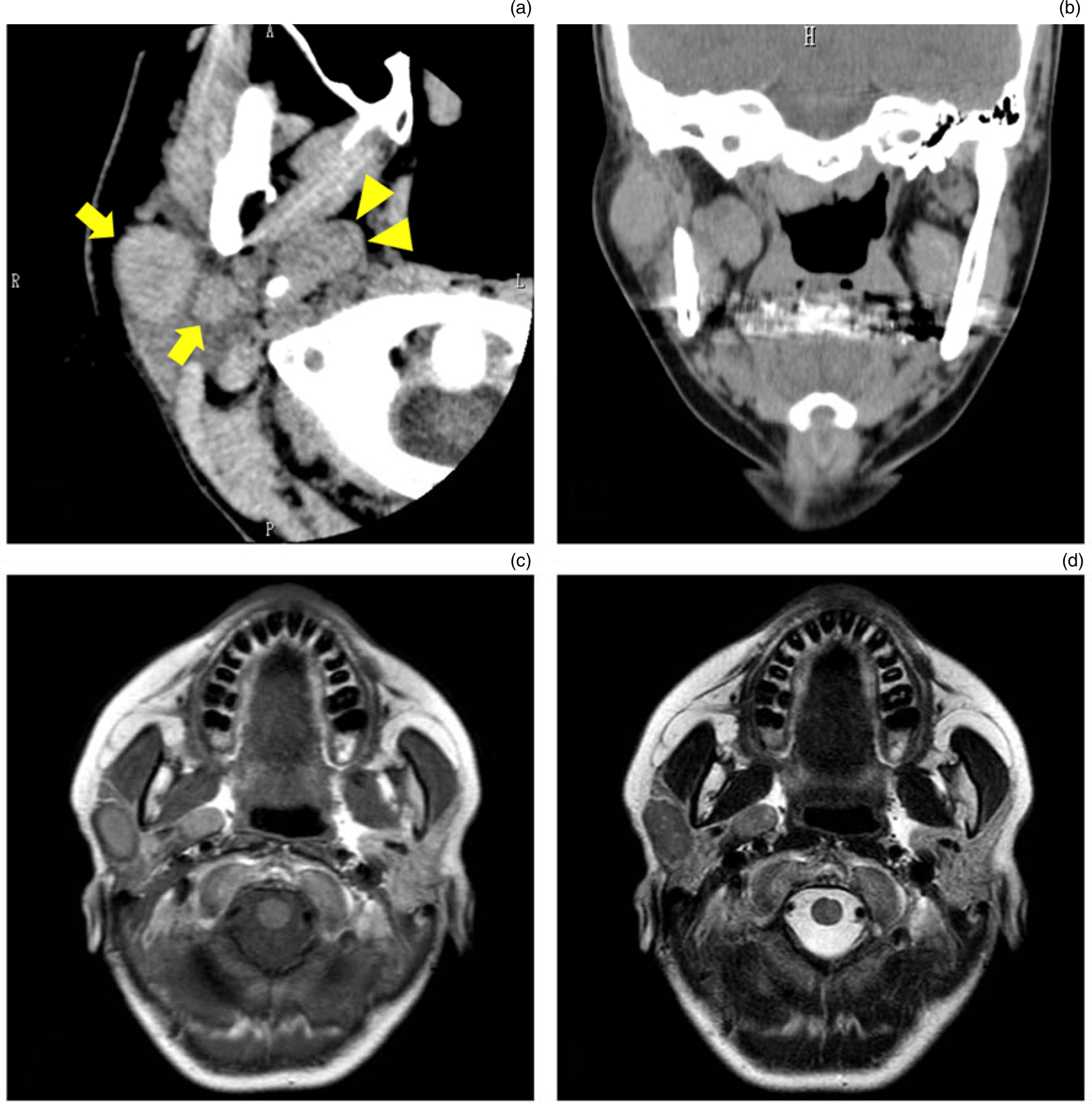
Fig. 1. Plain axial computed tomography (CT) image (a) showing a single tumour in the parapharyngeal space (arrowheads) and multiple tumours in the parotid gland (arrows). In the coronal CT image (b), an oval-shaped tumour adjacent to the medial pterygoid muscle is observed in the parapharyngeal space. On T1-weighted and T2-weighted magnetic resonance imaging scans (c & d), these tumours show isointense and heterogeneous hypointense signals, respectively. A = anterior; R = right; L = left; H = head
After obtaining informed consent, we planned a subtotal parotidectomy to preserve the facial nerve, and elective neck dissection (levels II and III). The intra-operative rapid pathological diagnosis of a level III lymph node showed no malignancy. The tumour in the superficial parotid was revealed as carcinoid tumour; thus, a planned range of neck dissections were performed prophylactically. Subtotal parotidectomy with preservation of all facial nerve branches using a nerve integrity monitoring system (Medtronic Xomed, Jacksonville, Florida, USA) was also performed as planned.
Overall, there were four tumours within the parotid gland. A cervico-parotid approach was used to reach the parapharyngeal space. After the stylomandibular ligament was cut and the mandibular angle was raised, a yellowish tumour was exposed and removed, to avoid damaging the glossopharyngeal nerve, the pharyngeal branch of the vagus nerve, and facial nerve (Figure 2). As there were no complications except temporary facial palsy of House–Brackmann grade III, the patient was discharged 5 days post-surgery. The facial palsy completely recovered within two months.

Fig. 2. Tumour extracted from the parapharyngeal space (a). The digastric muscle was pulled out (yellow string). The blue arrowhead indicates the facial nerve, and the green arrowheads indicate the tumour. (b) Image after removal of the tumour. The specimens are shown in (c). The yellow arrow indicates the tumour excised from the parapharyngeal space.
Histopathological examination of the parapharyngeal space and parotid gland tumours showed proliferation of mildly atypical cells arranged in trabecular and ribbon patterns on haematoxylin and eosin staining. Immunohistochemical analysis showed that these cells were positive for cytokeratin AE1/AE3 and synaptophysin, but negative for chromogranin A, indicating carcinoid tumour (Figure 3). The Ki-67 index was 0.6 per cent, and no invasion into the surrounding structures was found. A total of 22 cervical lymph nodes excised by neck dissection showed no malignancy. No adjuvant therapy was administered, and no relapse occurred during the nine months after surgery.

Fig. 3. (a) Mildly atypical cells are arranged in trabecular and ribbon patterns on haematoxylin and eosin staining (×200). These cells showed no signs of necrosis or mitotic activity. Cells are strongly positive for AE1/AE3 (×400) (b) and positive for synaptophysin (×400) (c), but negative for chromogranin A (×400) (d).
Discussion
We report a case of middle-ear carcinoid tumour metastasising to the parapharyngeal space and parotid gland. Approximately 55 cases of middle-ear carcinoid tumour have been reported.Reference Liu, Chen, Li and Liu4 Based on both clinical aspects of an indolent course and historical aspects of the lack of necrosis and significant mitotic activity, middle-ear carcinoid was previously considered to be benign; however, regional and distant metastases have been reported in eight cases, suggesting that the carcinoids should be classified as having a low-grade malignancy.Reference Fundakowski, Chapman and Thomas2 The mean duration between initial diagnosis and metastasis was 14.1 years.Reference Liu, Chen, Li and Liu4
To the best of our knowledge, this is the first report of metastasis to the parapharyngeal space, based on the search results for the key words ‘carcinoid tumour’ and ‘metastasis’ in the PubMed database. According to a systematic review by Riffat et al.,Reference Riffat, Dwivedi, Palme, Fish and Jani5 approximately 80 per cent of tumours in the parapharyngeal space are benign and 20 per cent are malignant. These lesions commonly originate from the parotid gland and neurons.Reference López, Suárez, Vander Poorten, Mäkitie, Nixon and Strojan6 Although metastasis to the parapharyngeal space is rare, the spread of cancer of the pharynx and the thyroid has occasionally been reported.Reference Teshima, Otsuki, Shinomiya, Morita, Furukawa and Morimoto7,Reference Otsuki, Nishikawa, Iwae, Saito, Mohri and Nibu8 As the parapharyngeal space contains numerous lymphatics, including drainage of the middle-ear mucosa, this can be a site of metastasis from a middle-ear tumour.Reference Batsakis and Sneige9 Physicians should be aware that solitary lesions emerging in the parapharyngeal space could be mistaken for benign tumours such as neurinoma.
During surgery, the approach to the parapharyngeal space is also important, and should be determined depending on the age and condition of the patient, and on the size and location of the tumour.Reference Prasad, Piccirillo, Chovanec, La Melia, De Donato and Sanna10 In this case, the cervico-parotid approach was selected because the patient was a younger woman with a 17 mm tumour in the pre-styloid compartment of the parapharyngeal space, and subtotal parotidectomy was necessary.
Surgical management of parapharyngeal space tumours is subject to residual or metastatic relapse. In our case, at first, residual recurrence could be suspected in terms of carcinoid tumour extending close to the carotid canal at the last local relapse; however, the likelihood appeared to be low based on the imaging findings of a well-circumscribed tumour apart from the carotid canal, and with no previous bone invasion. Therefore, the parapharyngeal space tumour was considered metastatic and was removed to reduce complications. Neck dissection was planned for levels II–V of the malignant parotid tumour if the intra-operative rapid pathological diagnosis of level III lymph nodes had revealed malignancy. The examination showed no malignancy, leading to the decision to perform neck dissection only for levels II and III.
According to a previous report, regional metastasis of a middle-ear carcinoid tumour is likely to occur in patients with local recurrence after a long period following tumour resection.Reference Salzman, Stárek, Tichá, Skálová and Kučera3 Thus, careful, complete tumour removal is important to prevent metastasis. Nevertheless, the middle ear has a complicated small space containing blind spots (such as the facial recess and tympanic sinus) and has important organs (such as the inner ear and facial nerve), suggesting that tumour resection with adequate surgical margins is difficult.Reference Sato, Saito, Fujita, Seo and Doi11 Indeed, the surgical recurrence rate is 18–22 per cent.Reference Torske and Thompson12,Reference Pellini, Ruggieri, Pichi, Covello, Danesi and Spriano13 If the ossicular chain is involved and not removed, recurrence is much more likely.Reference Knerer, Matula, Youssefzadeh, Ulrich and Swoboda14 Therefore, radical mastoidectomy should have been selected during the second surgery. Conversely, recurrence has been reported even after radical tympanomastoidectomy, and a patient in one case finally underwent extended subtotal petrosectomy for complete removal of the lesions.Reference Knerer, Matula, Youssefzadeh, Ulrich and Swoboda14 A better way to prevent recurrence may be radical mastoidectomy with endoscopy, securing adequate vision. The resulting hearing loss can be improved using bone-anchored hearing aids or middle-ear implants.
• Middle-ear carcinoids may metastasise to the parapharyngeal space
• Solitary lesions in the parapharyngeal space may be carcinoid metastasis
• Metastatic carcinoid lesions in the parapharyngeal space should be removed to avoid complications
• Radical mastoidectomy should be the planned initial surgery for middle-ear carcinoid tumours to prevent relapse and metastases
• A planned second surgery within a year may be useful
Although the period between primary surgery and local recurrence is reported to range from 15 to 33 years, some cases recur within a year,Reference Liu, Chen, Li and Liu4,Reference Ramsey, Nadol, Pilch and McKenna15 as in our case. A planned second-stage tympanoplasty that narrows the interval may be required to lower the possibility of residual recurrence. Staged surgery after six months was effective for local control of the carcinoid in our case, whereas long-term observation was required in preparation for metastasis. Staged surgery performed within at least a year may be recommended to properly manage a middle-ear carcinoid tumour.
An indicator of metastasis has not been reported to date. In the pathological examination of Ki-67 immunoreactivity, an indicator of the ability of tumour proliferation, the majority of small-cell carcinomas show higher than 25 per cent immunoreactivity;Reference Aslan, Gulbahce, Pambuccian, Manivel and Jessurun16 however, Ki-67 immunoreactivity of middle-ear carcinoid tumours is generally very low, as in the case of our patient (0.6 per cent).Reference Aoki, Mizuta, Ueda, Yamada, Ito and Kato17 Further studies on the genetic analysis of metastatic factors should be conducted in the future.Reference Warth, Herpel, Krysa, Hoffmann, Schnabel and Schirmacher18,Reference Kim, Yi, Jun, Ahn, Ahn and Lee19
Competing interests
None declared





