Published online by Cambridge University Press: 15 September 2021
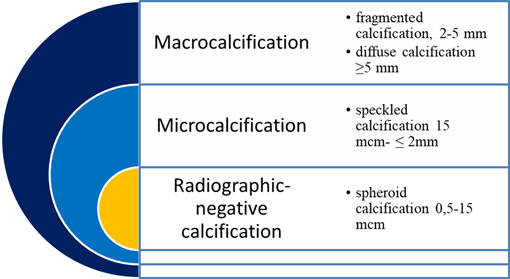
Ectopic calcification or pathological biomineralization correlates with morbidity and mortality from cardiovascular diseases. Aortas with atherosclerotic lesions and biomineralization were selected for the study. Thirty samples of mineralized abdominal aortas (group M) were examined by histology. Depending on the calcifications size, samples were separated into group M1 (macroscopic calcifications) and M2 (microscopic calcifications). Each group consists of 15 samples. Calcification 2 mm or less were considered as microscopic, >2 mm—macroscopic. Thirty samples of aortic tissue without biomineralization (group C) were used as a control group. Aortic tissue was examined by macroscopic description, histology, histochemistry, immunohistochemistry (IHC), scanning electron microscopy (SEM) with microanalysis, and transmission electron microscopy (TEM). The results of IHC showed the involvement of OPN in the formation and development of pathological biomineralization, but the obvious role of OPN in the differentiation of macro- and microcalcifications of atherosclerotic aorta was not revealed. SEM with X-ray microanalysis confirmed that the biomineral part of the aortic samples of the M1 group consisted mainly of apatites, which correspond to previous studies. The Ca/P ratio was less in the M2 group than in the M1 group. It means that microcalcifications can be formed by more defective (immature) hydroxyapatite.