Introduction
Urinary symptoms in women are common, often tolerated or ignored for many years after childbirth (Peake et al., Reference Peake, Manderson and Potts1999; Li et al., Reference Li, Low and Lee2007), with a negative impact on general and mental health (Coyne et al., Reference Coyne, Wein, Tubaro, Sexton, Thompson, Kopp and Aiyer2009). This study was developed following research on urinary incontinence in older women (Wagg et al., Reference Wagg, Barron, Kirby and Corlett2007a), which used a validated symptom questionnaire, female urinary symptom score (FUSS) to identify women who despite symptoms had not sought help (Wagg et al., Reference Wagg, Barron, Kirby, Stott and Corlett2007b). Results demonstrated that women often experienced urinary incontinence from childbirth but took no action. Simple treatment was offered and proved effective; however, some women declined the invitation, being unconvinced that an issue existed (Wagg et al., Reference Wagg, Barron, Kirby and Corlett2007b). These findings have been supported by other research (MacArthur et al., Reference MacArthur, Lewis and Bick1993; Mason et al., Reference Mason, Glenn, Walton and Hughes2001; Hunskaar et al., Reference Hunskaar, Lose, Sykes and Voss2004; Brown et al., Reference Brown, Gartland, Perlen, McDonald and MacArthur2015).
Stress incontinence is defined as ‘the complaint of involuntary urinary leakage on effort or exertion, or on sneezing or coughing’ (Abrams et al., Reference Abrams, Cardozo, Fall, Griffiths, Rosier, Ulmsten, van Kerrebroeck, Victor and Wein2003: 38). Women may also experience urgency (a sudden compelling desire to pass urine which is difficult to defer), leading to urge incontinence, or a mixture of the two (Abrams et al., Reference Abrams, Cardozo, Fall, Griffiths, Rosier, Ulmsten, van Kerrebroeck, Victor and Wein2003). The pelvic floor acts as a sling for the pelvic organs, and anatomical and physiological changes in pregnancy affect function of the lower urinary tract and pelvic floor (Freeman, Reference Freeman2002). Pressure of the enlarging uterus pushes the bladder down and can increase the bladder neck mobility causing stress incontinence and sphincter dysfunction can result in urge incontinence (Freeman, Reference Freeman2002).
It is well known that women frequently take no action regarding urinary symptoms (Ashworth and Hagan, Reference Ashworth and Hagan1993; MacArthur et al., Reference MacArthur, Lewis and Bick1993; Peake et al., Reference Peake, Manderson and Potts1999; Shaw, Reference Shaw2001; Mason et al., Reference Mason, Glenn, Walton and Hughes2001; Koch, Reference Koch2006; Li et al., Reference Li, Low and Lee2007). The body of literature on this remains small in the female population, particularly postnatally. A systematic review (Thom and Rortveit, Reference Thom and Rortveit2010) found the prevalence of incontinence, particularly stress, remained high up to a year after delivery, doubling for those who had a vaginal delivery. A pooled prevalence of 33% at three months was identified. A large study in Sweden investigating incontinence 20 years after delivery, found the prevalence of incontinence was 67% higher in those who experienced a vaginal delivery and identified that persistent problems remained three times higher in those women (Gyhagen et al., Reference Gyhagen, Bullarbo, Nielsen and Milsom2012). Issues with standardisation remain; there are no standard guidelines for assessing symptoms or identifying those at risk. Some research, evaluating methods, has shown some studies to be of poor quality and difficult to assess (Martin et al., Reference Martin, Williams, Abrams, Turner, Sutton, Chapple, Assassa, Shaw and Cheater2006). Until standardised tools and timescales are used it is impossible to state with any certainty the true prevalence of urinary symptoms in women within any age group or time span.
Health policy in England and Wales including National Service Framework for Children, Young People and Maternity services [Department of Health (DH), 2004], Modernising Maternity Care (DH, 2006), and Routine Postnatal Care of Women and their Babies [National Institute for Health and Care Excellence (NICE), 2006a] take little account of women’s enduring health after the immediate postnatal period. However, general continence guidance available (NICE, 2006b) includes clear detail on initial assessment and forward management. This guidance has been updated regularly in the light of new drugs, treatment or evidence (NICE, 2013; NICE, 2015). The International Continence Society (ICS) has published comprehensive fact sheets (www.ics.org), including recommended bladder diaries, symptom questionnaires and assessment guidance.
A systematic review, undertaken before this study, identified that unassisted pelvic floor muscle exercises (PFME) may be effective in reducing antenatal and postnatal urinary incontinence, particularly with intensive intervention, but benefits may not be maintained over time (Wagg and Bunn, Reference Wagg and Bunn2007), this was also the conclusion of a more recent review (Morkved and Bo, Reference Morkved and Bo2013). However, the body of literature was small and interventions and measurement intervals varied widely. Recent reviews remain unclear on the best treatment for effective pelvic floor management, with some evidence that frequent appointments helped but no evidence of maintained improvement after treatment (Hay-Smith et al., Reference Hay-Smith, Herderschee, Dumoulin and Herbison2011). More research is needed as PFME are offered so widely in practice (NICE, 2015).
From the literature, it was clear interventions offered could be viewed negatively and in addition symptoms were not seen as medically significant (Koch, Reference Koch2006). Women often seemed to consider urinary symptoms ‘normal’ after childbirth despite considerable effects both physical and psychological (Mason et al., Reference Mason, Glenn, Walton and Hughes2001; Shaw, Reference Shaw2001; Koch, Reference Koch2006). Healthcare professionals appear unwilling to discuss urinary symptoms (Strahle and Stainton, Reference Stamler2006) and may lack knowledge to impart useful information (O’Connell et al., Reference O’Connell, Hanna, Bailey, Walsh and Prosser2002). This study aimed to explore, describe and enhance understanding of the experiences and beliefs of women experiencing urinary symptoms in pregnancy and postpartum, and to explore the attitudes, beliefs and knowledge of health professionals regarding these issues.
Methods
Design
A qualitative approach was chosen to obtain the views of the women and health professionals. Careful consideration was necessary to find a match between the research questions and a theoretical perspective to underpin this research. An approach that would identify explanations of behaviour, the hidden meanings and the constraints of social relations, by seeking the views of the users, was needed. Grounded theory was selected as developed by Glaser and Strauss (Reference Glaser and Strauss1967), using the adapted version by Charmaz (Reference Charmaz2006), which allowed for some prior sensitisation.
Grounded theory seeks to examine social processes and attempts to understand the variations that different interactions produce (Heath and Cowley, Reference Heath and Cowley2004). It is also one way of giving women a voice regarding the conflict that often exists between caring activities and personal health issues (Crooks, Reference Crooks2001). The methods of grounded theory specify analytic strategies not data collection methods, thus allowing the use of multiple data collection method (Charmaz, Reference Charmaz2000).
Participants
Ethics approval for the study was obtained from the local ethics committee (ref EC02580). The study including interviews, focus groups and observation, was undertaken in 2008. The interviews and focus groups were conducted by a female researcher (the first author, a practice nurse) as part of a PhD. Training and experience were accessed during a Masters degree in research and evaluation. Although the grounded theory approach cannot determine sample size as such it was hoped to interview around 20 women based on previous qualitative studies and expert information (Morse, Reference Morse2000; Elliot, Reference Elliot2010; Meng et al., Reference Meng, Xiuwei and Jiang2011).
The selected population were all women who had given birth ~12 weeks earlier in one large general practice in Hertfordshire. Recruitment was by letter or personal invitation. Women who had experienced a stillbirth or delivered a child with physical problems were excluded as were women who had personally experienced health problems. Letters were either posted or given to women when they attended the postnatal clinic. Initial response was poor (two interviewees from 30 letters). Additional verbal ethics committee approval was obtained to attend postnatal groups locally; this was more successful. Difficulty was experienced recruiting ethnic minority groups and teenage mothers. Although personal invitation was employed for these groups, it was only possible to recruit one mother from an ethnic minority to be part of the study. No teenage mothers agreed to take part.
The health professionals recruited included general practitioners, nurses and the midwives who attended the practice. Local continence nurses were also invited. Invitation was by personal invitation and a short explanatory leaflet. No health professional refused to attend the groups.
Data collection
For the women, theoretical sampling was employed, recruiting by convenience initially and then in relation to emerging themes. Semi-structured individual interviews were conducted using a short topic guide which enlarged as new information emerged (Box 1). Care was taken to ensure the interview did not become too structured as the guide enlarged. A pilot interview was undertaken and analysed with the second author. The interviews were undertaken in the privacy of home and recorded for later analysis. A consent form was signed and a FUSS questionnaire completed. The women were scored as mild (0–8), moderate (9–18) or severe (>19).
Box 1 Topic Guide: Women
The following demographic information will be obtained; Age number of pregnancies Ethnicity type of delivery Occupation Breastfeeding? Smoker or not?
Thank you very much for agreeing to take part. Explain and obtain consent, discuss confidentiality, recording and storage of tapes, opt out at any time, in total or from recording. The following subject headings will be used if necessary, but the women will be encouraged to lead the conversation.
The definition of leakage How common it is causes treatment, knowledge and opinion talking about it; with a) family b) friends c) health professionals Effect on lifestyle Future issues Accessing help Where and when should it be?
Anything else you would like to add?
Thank you very much for taking part, your contribution is very valuable and I really appreciate the time you have spared, particularly when you have a new baby to look after. I hope that if you do ever have any urinary symptoms you will feel you can ask for help.
The women were informed that confidentiality would be maintained and tapes stored safely away from the surgery. Admission of the sensitive issue of continence symptoms may be embarrassing and upsetting and the researcher was ready to abandon the interview if necessary, to deal with the distressed woman (Clark, Reference Clark2006).
Two observation sessions of 2 h were undertaken; one at an antenatal clinic, one at a postnatal mothers group. At the antenatal clinic verbal consent to the presence of the researcher was obtained on arrival at reception with the opportunity to be consulted alone offered. Confidentiality was assured; the researcher was a staff member in the practice. The researcher made notes and memos and later discussed the clinic with the midwife in accordance with ethics approval. For the postnatal mothers group, again verbal consent was obtained, the researcher explained the purpose of her presence and the study and offered to leave if anyone objected.
For the health professionals, two multi-disciplinary focus groups of five were held (Box 2), with a time limit of 1 h. One general practitioner was interviewed separately as work pressure precluded attendance at the group.
Box 2 Topic Guide: Focus groups
Members of group; Facilitator Co facilitator (1st group only) Practice nurse Health visitor General Practitioner Midwife Continence nurse Family planning Nurse
Introduction;
Discuss ground rules One hour maximum time as staff have given up lunchtime to be here. Explain about tapes, storage, note taking, confidentiality, respect others opinions, term continence to be used.
Introduce myself; clinical role as practice nurse, interest in women’s urinary problems have found from previous research (FUSS) that older ladies are not keen to have treatment, symptoms often start with pregnancy, so aiming to look at why women do not come forward by asking them nearer to the time they start.
Ask participants to introduce themselves and say why they decided to take part. Possible topics; ask group if they do not arise as part of the conversation;
What involvement do you all have at present with women who might have problems with continence; First thoughts when someone consults with symptoms? What is your experience, do they come forward? What encourages people to come forward for help? Why not? How common do you feel it is from personal experience? How would you as a health professional find out what help is available? What do you know about the different types of continence problems? Do you think health professionals’ opinions have changed over time with regard to continence issues? Looking back what memories do you have of women with continence symptoms? How do you think society views women with continence issues? Anything else anyone would like to add?
Thank you for giving up your time today.
Analysis
Analysis followed the hybrid model demonstrated by Charmaz (Reference Charmaz2006). Recordings were transcribed after each interview to allow for analysis using constant comparison. The average length of interview was 45 min. Analysis was conducted manually, by the primary researcher alone other than the pilot interview which was also analysed by the second researcher. Emerging codes were listed and grouped into concepts using original text between each interview, using the advanced coding process (Norton, Reference Norton1999). Subsequent interviews were guided by emerging themes from previous interviews (Tuckett, Reference Tuckett2004). Memos, thoughts noted down by the researcher regarding data or other areas to pursue, further aid analysis (Charmaz, Reference Charmaz2006), and were also part of the process. Interviewing continued purposively, sampling for different types of delivery, parity and age and allowing for emerging themes until data saturation was reached (ie, same issues repeated and no new information coming forward). Saturation was confirmed between the researcher and her supervisors through revision of transcripts.
The two focus groups of health professionals were recorded and analysed similarly. As they took place on consecutive days it was not possible to fully analyse the recording from the first group, before the second took place, but some memos were made from listening to the recording. The two observation sessions were not recorded, but the researcher made notes and memos.
Evaluation can reduce the criticism sometimes levelled at qualitative research with regard to validity (Watson, Reference Watson2003); consequently, methods for enhancing rigour in research were utilised (Chiovitti and Piran, Reference Chiovitti and Piran2003, adapted from Beck, Reference Beck1993) (Table 1). This included asking the women to read the transcripts for verification and using the women’s own words in the theory. The health professionals received a copy of the transcript from the focus groups.
Table 1 Eight methods of research practice for enhancing standards of rigour

Source: Chiovitti and Piran (2003), adapted from Beck (1993).
Findings
Introduction
Data from 15 women (Table 2) and 10 health professionals (Table 3), and two observation sessions were analysed. Concepts and categories were formed leading to a core category which encompassed all data. From the findings within the women’s interview data three categories emerged from 30 concepts and from the health professional’s data five categories emerged from 17 concepts. Observational data were used to verify emerging concepts. The completed symptom scoring questionnaires were totalled. This was related to the interview data adding insight into women’s perceptions of the bother of urinary symptoms.
Table 2 Demographic information of participants
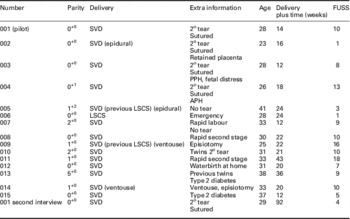
FUSS=female urinary symptom score; SVD=spontaneous vaginal delivery; PPH=postpartum haemorrhage; APH=antepartum haemorrhage; LSCS=lower segment caesarean delivery.
Table 3 Health professional participants of the focus groups
Health professionals
Clarifying pathways of care
The first category uncovered issues regarding knowledge of treatment and its effectiveness, accessing care and the national policies which impinged upon delivery. Everyone knew PFME were important but knowledge of performance and effectiveness differed.
I didn’t realise about the exercises because I thought the pelvic floor exercise was clenching the muscles and releasing but I didn’t realise you also had to do it and hold for 10 seconds. (HV1)
Weakness of the pelvic floor immediately after delivery and compliance with exercise was discussed. Continuing exercises was not always emphasised, however, the general practitioner reported that they advised women to take up Pilates.
It needs to be pushed to carry on the exercises forever … Some of the women I see late in life have no muscle tone and if they had just carried on with exercises. (GP1)
There was confusion about where to refer women with continence issues, this varied, depending on local service packages. Midwives admitted to using shortcuts to access care for women with continence issues. Continence nurses were keen to educate women and staff but were seldom contacted. National changes to midwifery-led care and amalgamation of midwifery units meant changes in education, this was perceived as an opportunity to effect change. Media influence was considered important; often negatively, encouraging pads rather than help seeking. This category identified a desire to do the ‘right thing’ but a lack of clarity as to what that was and who would be responsible for it.
Clarifying education
The second category ‘clarifying education’ revealed a lack of understanding of the educational requirements and provision for the women.
One health visitor stated:
I see a lot of mums with new babies. … it wasn’t actually anything I’d thought about until you brought the subject up and then I found I was interested. (HV1)
Conversely, the practice nurse was already asking women about symptoms and was keen to refer on. Attitudes of other health professionals were often coloured by poor educational knowledge, for example, giving pads as a quick solution. This was seen by the groups as negative and disempowering for the women.
I think generally there is only a small number of people that would be horrible to someone who had wet themselves unintentionally … but negative in that they go for pads easily. (CN1)
In addition, some had personal issues about preparedness for the education role relevant to postnatal women, particularly with regard to updating knowledge. This was frustrating and disempowering for the health professional and will have consequent effects on the women.
Education sessions organised by continence nurses had been cancelled due to poor bookings. This could lead to inappropriate referrals without prior investigation. Both midwives discussed the pelvic floor postnatally, but found little time in the antenatal period. Antenatal classes were prepared by individual midwives following discussion with the women. The continence nurses expressed frustration that women were too pre-occupied in the postnatal period when they spoke to groups and a brief leaflet in the discharge package was old and often ignored. While there is National Health Service (NHS) information that should be provided to all women it appears that this does not always happen.
Improving communication
The third category ‘improving communications’ identified a desire to ensure that two-way communication was enabled, by asking clear direct questions which could not be misinterpreted and would generate the knowledge required by the health professional to facilitate direction for women if necessary, to suitable care. However, other than the continence nurses few seemed to have a structured approach to continence. Some health professionals were unsure of the scale of the issue. Statements such as ‘they don’t really say’ indicated they were not asking.
Yes she goes to the toilet, the midwife she say are you weeing alright, she say yes but she didn’t know when she stopped. (MW st)
Some members of the group related personal experience; not knowing what was normal and when to seek help. It was clear everyone knew women had inadequate information, however, not everyone was asking the right questions. In addition, communication between health professionals could improve. A health visitor was unaware of current immediate postnatal care with handover limited to comments in the baby’s record.
Understanding actions
The fourth category ‘understanding actions’ identified that women were known to be reluctant to disclose symptoms and often delayed seeking help until the children were older or on return to work. Issues such as being pre-occupied meant concentration was poor and time was limited which may have led to inadequate performance of PFME. According to one of the midwives difficulties dealing with continence issues at work were a major trigger for seeking help. One continence nurse also said:
it’s usually when the children are about 5, just going to school and Mum gets back to normal, going to the gym etc. and finds there is a problem. (CN2)
It was suggested that regular reminders regarding exercises and enquiring about symptoms would be empowering and reduce barriers. In practice, however, this did not always seem to happen. The general practitioner was concerned that women did not consult and ‘put up with symptoms for ages’.
There was discussion around the taboo nature of incontinence, one of the clinical nurse specialists opined:
they talk about drugs, sex and sexually transmitted diseases and whatever else but we don’t talk about pooing and weeing. (CN2)
There was concern for those who had raised the issue but received a negative response; for example, ‘what do you expect you’ve had a baby’, would they ever ask again? Not doing the exercises was a major concern; women often could not do them immediately, and gave up.
Serious issues
The last small category raised the serious complications that can occur. Retention of urine can cause lifetime problems, the continence nurse spoke of a woman who catheterises daily following mismanagement in labour. Staffing problems can be an issue here:
you’ve got a midwife that’s looking after 2 or 3 women which happens and one is a bit more complicated, so eventually get to one and say have you been to the loo and she won’t have thought about it cos she’s in pain (MW2)
Faecal incontinence can occur and is distressing and difficult to with. It was assumed that women were more likely to consult however:
They’re much more likely to mention that.(MW1)
Yes it does tend to get reported.(CN1)
The midwives expressed concern regarding changing guidelines about suturing tears and the possible effect on the pelvic floor muscles.
To summarise, education of women seems erratic, there is misapprehension about areas of treatment and care and no standardised antenatal education programme. Importantly, it appeared that many health professionals expected the women to disclose problems, otherwise assuming there were none. It is unsurprising that the message received by women was at times unclear, and the findings from the women’s interviews are now explored.
The women
Messages women receive
The findings revealed that both antenatally and postnatally women may or may not be provided with information about PFME, which are external messages. However, the presentation, and the interpretation the women place upon this information indicated the internal message received could be different to that intended or perceived by the health professional. Lack of clear understanding or confusion may affect performance and confidence in the exercises, which could be disempowering.
Information was often unhelpful or not emphasised;
just said when you’ve got 5 mins do them. (FUSS Score 1, mild)
I do recall getting a leaflet but I don’t, it was more there’s some paperwork have a look at it not in like do you understand the importance of this. (FUSS Score 18, moderate)
Several could not do them to begin with:
you can’t hold it, you pull in and they’ve gone and they don’t actually say in the leaflet that that might happen. (FUSS Score 1, mild)
Some admitted not doing the exercises, whereas others did if symptoms increased:
Not as often as I should. (FUSS Score 10, moderate)
Hadn’t done them properly, noticed an improvement within about a week. (FUSS Score 10, moderate)
Guilt was experienced at not doing them:
I do forget, and I’m lying in bed thinking oh my God I didn’t do them again. (FUSS Score 10 moderate)
Some were doing them incorrectly:
I normally do my exercise when I’m there in the toilet. (FUSS Score 16 moderate)
Others kept going for a long time without seeking help:
it’s almost 6 months now and I’m thinking well how long …. (FUSS Score 10, moderate)
Women were often unclear about the purpose or effectiveness of the exercises or the importance. Most did not remember being asked about continence after delivery. Possibly the right questions were not asked in the right way; this could lead to women not disclosing concerns. Several women declared they would answer direct questions but would not volunteer information. Part of this was being unaware what was normal, not wanting to make a fuss or be told to get on with exercises.
Seeking and understanding information
The findings indicated that at times women sought clarity from other sources. Several different mechanisms were used to access further information. This could mean receiving disturbing messages from relatives. These messages were not necessarily correct but could have a profound effect on the women, causing uncertainty and reducing confidence in the effectiveness of the exercises:
‘it’ll never be the same after you have the baby’ and ‘after having babies it happens and it’s got worse with age’.
Perceptions and experiences of urinary symptoms in relations or peers were worrying and implied that incontinence was inevitable and permanent. Television was a powerful influence:
‘I get paranoid just seeing the advert you know for Poise’ (FUSS Score 16, moderate) and
‘programmes like Loose Women are good, talking things through openly’. (FUSS Score 7, mild)
Three women already wore pads all the time, none had sought help, thin pads were preferred as they were easily available and not obvious:
even just walking around I permanently wear like a panty liner, I’m always sort of leaking. (FUSS Score 13 moderate)
Some bought books but found that the postnatal period was given little significance:
it didn’t really do afterwards at all apart from scar care. (FUSS Score 7 mild)
One woman preferred to ring NHS Direct, whereas others gathered information opportunistically, for example, several asked the researcher questions. The continence nurse assumed women used the internet for information; one woman had done so.
Symbolic language such as ‘how are your waterworks’ is open to misinterpretation. The women were asked to interpret this, several thought it referred to infections, one was unsure and only four felt it referred to leakage. None of the women had sought clarification and just said ‘ok’ if unsure. The health professionals did not appear to be creating a suitable environment for discussion. The next category discusses how the women responded to the information received.
Responding to the messages
This category reflects the reactions of the women to the messages received, whether internal or external. Responses to external messages from information on PFME and possible results of not doing them may be influenced by interpretations placed on the information and the concerns experienced as a result of these interpretations. In particular, comments by friends and relatives may encourage normalisation of the symptoms, unbeknown to the health professional. Most women opted to see a general practitioner or practice nurse if help was needed. Reasons for not seeking help included fear of examination:
don’t want to be fiddled about with anymore. (FUSS Score 9, moderate)
Or embarrassment:
it’s too embarrassing to walk into the Health Centre and say I’m having trouble with my bladder. (FUSS Score 10, moderate)
Some were unsure about the legitimacy of their concerns:
you don’t know how bad it is compared to somebody else. (FUSS Score 13, moderate)
Certain life events would trigger action:
I will go and see someone, I can’t possibly have this when I am teaching. (FUSS Score 4, mild)
Justification for doing nothing was often related to the exercises, not doing them enough, or no other help was available. Symptoms were often minimised:
it’s only a little bit, not like oh I’ve wet my pants. (FUSS Score 16, moderate)
Concern was raised if symptoms did not go away, and how to cope:
the boys like me to play football with them, won’t be able to do that. (FUSS Score 9, moderate)
It was clear that it was not any easy subject to talk about, and it took time to develop relationships in the antenatal classes. Some women preferred to discuss with a close relative, some a close friend. There was a strong feeling that ‘getting on with it’ was the required programme:
It’s a problem we’ve got to deal with ourselves and just get on with it, another burden like periods and things like that. (FUSS Score 10, moderate)
Friends who had enduring symptoms tended to joke about them as did most of the women when asked.
The core category: overcoming barriers to facilitate empowerment
The core category (Figure 1) embodies the previous categories, the issues discussed have highlighted barriers to knowledge, understanding and consequent action, caused at times by inadequate or infrequent information due to either poor communication or education. This may be influenced by poor knowledge of the process or the role of others within postnatal care on the part of health professionals. In addition, stereotypical symbolic language sometimes used may be misinterpreted. Powerful messages may be internally conveyed by friends and relatives, encouraging normalisation of symptoms. These issues create barriers and lead to disempowerment for both women and health professionals. The discussion will focus on the four main areas: knowledge, communication, barriers and empowerment.

Figure 1 Applying the core category. W=women; HP=health professional
Discussion
This study drew on grounded theory to explore the aims and objectives. The core category has enabled a new understanding of the experiences of urinary symptoms in women in the postnatal period to be reached and is therefore central to developing new ways to empower both women and health professionals to approach this issue. In particular, it was clear there were barriers to communication leading to disempowerment and normalisation of symptoms. The first component of the core category, knowledge, needs to be evidenced, current and available. In the United Kingdom, government policies provide relevant current knowledge to health professionals, are readily available digitally, and do contain information for the public (NICE, 2014; 2015; 2016; NHS England, 2015). Internationally, other guidelines have been produced, for example, Europe (Lucas et al., Reference Lucas, Bedretdinova, Berghmans, Bosch, Burkhard, Cruz, Nambiar, Nilsson, Tubaro and Pickard2015) and United States (Syan and Brucker, Reference Syan and Brucker2016). However, there is a lack of consensus and clarity in some areas, uncertainty of long-term maintenance of improvement internationally as well as within the United Kingdom (Hay-Smith et al., Reference Hay-Smith, Herderschee, Dumoulin and Herbison2011; Bo and Hilde, Reference Bo and Hilde2013), and a small body of comparable research due to variation in measurement tools and research populations (Morkved and Bo, Reference Morkved and Bo2013). It can be seen therefore that it may be difficult for the health professional to reach a clear understanding of the correct advice. The ICS works collaboratively with many countries to standardise definitions and diagnostic and care pathways including patient advice and information (https://www.ics.org, Rosler et al., Reference Rosler, Ridder, Meijlink, Webb, Whitmore and Drake2012).
Antenatal advice is for women to be taught PFME at booking (although ability to instruct is not a required competence) and referred for further evaluation if symptoms do not resolve (NICE, 2014; 2016). Evidence for competencies necessary to identify and manage urinary symptoms was unclear (NICE, 2015), however, Martin et al. (Reference Martin, Williams, Abrams, Turner, Sutton, Chapple, Assassa, Shaw and Cheater2006) did identify that most simple diagnostic tests could be undertaken in primary care, although interpretation was difficult due to the number of diagnostic tests and symptom scoring tools available. This may leave the health professional unconvinced and ill prepared to instruct women (Strahle and Stainton, Reference Stamler2006). None of the mothers interviewed had accessed any government documents. Advice on ‘postnatal self-care’ at 36 weeks gestation is not clarified and the content of the postnatal examination is unclear (NICE, 2016). Interestingly, no research regarding frequency of assessment or informational needs of women on urinary incontinence was found (NICE, 2006b). This muddled picture is not conducive to good communication.
The knowledge to aid pelvic floor health needs to be imparted effectively to women. The Pregnancy book (DH, 2007) is given to first-time mothers and discusses pelvic floor exercises and how to perform them, and Emma’s diary (Royal College of General Practitioners, 2007) is issued with each pregnancy and contains limited information. However, none of the women spoke of these publications as a primary source of information. Information is there to be imparted, albeit with some reservations regarding strength of the evidence, but women are not always receiving clear messages to access it. There was some confusion; the women did not always connect urinary incontinence with the pelvic floor and other research confirmed this (O’Connell et al., Reference O’Connell, Hanna, Bailey, Walsh and Prosser2002), also women were unsure how long to continue (Chiarelli et al., Reference Chiarelli, Murphy and Cockburn2003).
From the findings, it was evident that a significant barrier to help seeking was the fact that urinary symptoms were largely communicated as being normal. One woman had sought help for urinary symptoms, and had received no constructive assistance. Women experienced powerlessness if a help-seeking encounter was unsatisfactory (Haaglund and Ahlstrom, Reference Haaglund and Ahlstrom2007). The fact that it is not often discussed confuses the women; do health professionals not want to talk about it or is it normal? The findings confirmed inconsistency in the programme for antenatal classes; content usually being at the midwife’s discretion. At times education is uncertain, brief, limited and not reinforced by discussion with a health professional. This has been found by other authors (Mason et al., Reference Mason, Glenn, Walton and Hughes2001; Herron-Marx et al., Reference Herron-Marx, Williams and Hicks2007). Women often did not attend classes or read booklets in subsequent pregnancies. However, researchers have attempted to improve physical outcomes by intensive programmes and have found no evidence of maintained effectiveness (MacArthur et al., Reference MacArthur, Winter, Bick, Knowles, Lifford, Henderson, Lancashire, Braunholtz and Gee2002; Reid et al., Reference Reid, Glazener, Murray and Taylor2002; Lumley et al., Reference Lumley, Watson, Small, Brown, Mitchell and Gunn2006).
The messages the women received from unofficial sources were much more powerful and disturbing, including negative information from friends and family and personal contact with elderly relatives. This was worrying and upsetting but paradoxically did not necessarily prompt performance of exercise; instead it created a climate for normalisation. Advertisements for pads reinforced this. The internet can be helpful by offering anonymous treatment, more often accessed by women (Powell et al., Reference Powell, Inglis, Ronnie and Large2011) and is thought to help with access to care and can be empowering (Bjork et al., Reference Bjork, Sjostrom, Johansson, Samuelsson and Umefjord2014). However, only one woman reported searching the internet, although they all had easy access to it. Interestingly, it appeared that the women interviewed would be prepared to discuss continence but wanted the heath professional to raise the subject. Needing to be sure first that the symptoms were abnormal was creating a barrier to help seeking. Women’s educational needs vary and individual assessments may be necessary to ensure women have the knowledge required to enable empowerment (Stamler, Reference Strahle and Stainton1998). Understanding the reasons for undertaking pelvic floor exercises and achieving effective performance could also be empowering for the women.
Strengths and weaknesses
The study was conducted in the researcher’s usual area of work, with continual appraisal of the effect of personal knowledge and experience to maintain a reflexive approach (McGhee et al., Reference McGhee, Marland and Atkinson2007). The use of semi-structured interviews with open questions increases depth, encourages new concepts, allows participants to share personal experiences (Dearnley, Reference Dearnley2005) and the constant comparative approach of grounded theory permits new knowledge to be further explored. The use of the actual words of the interviewee increases rigour giving a true reflection of the opinion of the interviewee (Chiovitti and Piran, Reference Chiovitti and Piran2003). It also gave women permission to talk about personal issues rather than family considerations (Crooks, Reference Crooks2001).
However, the slow recruitment prolonged the data collection period and it was disappointing that no teenage girls and only one woman from an ethnic minority background agreed to be interviewed. Valuable cultural insight may have been missed. On reflection, it would have been better to use personal invitations only rather than letters. Interviewees sometimes asked for advice due to the researcher’s profession. This conflict is not unusual (Carolan, Reference Carolan2003).
Conclusion
In summary, from this study it is evident that women have different needs depending on symptoms and personal knowledge and attitudes towards them and some key issues have been identified. In particular, the power of the influence of friends and relatives has emerged as a much stronger issue than previously realised in the literature; it is far more complex than merely accepting symptoms as normal. However, the belief that urinary symptoms were ‘normal’ after pregnancy was firmly embedded in the cultural experience of childbirth. The symbolic interaction underlying how some women behave is key to understanding the lack of action at times. The meaning of the symptoms to the women may preclude action as they may feel impelled to comply with the accepted norm and fear rejection by other women if they have the temerity to ask for help. Also, emerging as a strong concept was the disinclination to undergo further examination in the postnatal period as a deterrent for help seeking. At times women were prepared to lie about symptoms to evade examination. Empowerment for women therefore about postnatal urinary symptoms means being able to believe that looking after the pelvic floor is normal and not accepting urinary symptoms after childbirth as normal. An intervention is unlikely to be successful unless it has empowerment as a basic premise, I would propose that there is no right intervention, only several care pathways that enable choice and the appropriate outcomes for women as defined by themselves.
Implications for practice
Referral or treatment must be initiated in general practice, therefore all general practitioners, practice nurses, health visitors and family planning nurses need to be aware of the guidelines, available services and treatment. The pelvic floor needs to be given more importance around pregnancy, too often it is left out of discussions. The health professional has an important role in facilitating care before the symptoms are normalised, therefore every opportunity should be utilised to ask about urinary symptoms from an early age, and symptom scoring tools are invaluable here. Increasing knowledge for woman and health professional will help communication, reduce barriers and increase empowerment.
Acknowledgements
The researcher would like to thank the Health Centre involved for supporting the project and particularly the women for agreeing to talk about sensitive issues. Funding received was for protected time only and had no influence on the study. Great care was taken to ensure confidentiality and no woman can be identified by any part of the article.







