The overall life expectancy of people who receive psychiatric treatment is lower than that of the general population. Reference Cubeddu1 This is attributed to factors such as comorbidity, increased cardiovascular risk and inadequate use of healthcare services. Reference Nose, Barbui and Tansella2 Iatrogenic causes such as the use of high-dose antipsychotics should also be taken seriously. Reference Abdelmawla and Mitchell3
The causative role of psychotropic drugs in the development of sometimes severe and even life-threatening arrhythmias has been extensively researched. Reference Sala, Vincentini, Brambilla, Montomoli, Jogia and Caverzasi4 It is now apparent that certain antipsychotics, both typical and atypical, have the propensity to prolong the QTc interval. This acts as a surrogate marker for the development of torsade de pointes, a polymorphic ventricular tachyarrhythmia that may cause sudden death. Reference Harrigan, Miceli, Anziano, Watsky, Reeves and Cutler5 The QTc interval can be measured by either Bazett's or Fridericia's method. Using Bazett's method, Reference Bazett6 a QTc interval of 430–450 ms in men and 450–470 ms in women is considered borderline. Values higher than this indicate a prolonged QTc interval. Furthermore, values above 500 ms have been accepted as indicating a increased risk of dangerous arrhythmias. Reference Glassman and Bigger7-Reference Malik and Camm9
Factors implicated in the prolongation of the QTc interval may be pharmacological or non-pharmacological. Drugs such as thioridazine, pimozide and sertindole may have a considerable effect on QTc intervals, Reference Taylor, Kerwin and Paton10 and intravenous administration can increase that risk substantially. Other factors have been implicated such as the use of high doses of antipsychotics, polypharmacy (use of two or more drugs from the same class) and the use of drugs that act on the cytochrome P450 isoenzyme system. Non-pharmacological risk factors such as age, electrolyte imbalance, ischaemic heart disease, central nervous system disease, endocrine dysfunction and congenital long QTc syndrome are also associated with pathological prolongation of the QTc interval. Reference Taylor, Kerwin and Paton10
The aims of this work were two-fold: first, to assess trainee psychiatrists’ knowledge of QTc issues pertinent to psychiatry through the use of a brief survey; and second, to investigate the monitoring of QTc intervals in electrocardiograms (ECGs) on four in-patient wards through examining patient notes.
Method
Survey 1: monitoring junior doctors’ knowledge of QTc
We recruited 53 psychiatric trainees (pre-MRCPsych part 2) in four inner-city mental health trusts in London. The first junior doctor was selected because he worked on our ward. Other participants were selected using the snowball method, in which existing participants identify other potential recruits from their associations. Reference Salganik and Heckathorn11 The survey comprised three questions.
-
• Do you know what the QTc interval means?
-
• What is its significance in psychiatry?
-
• Above what value would you be concerned?
The criteria for marking the questions are listed in Box 1. Answers that were not consistent with our defined criteria were marked as incorrect.
Box 1. Survey of QTc knowledge: marking criteria
-
• Question 1: the QTc interval is a measure (in ms) of the distance betweenthe Q and T wave corrected for heart rate on the ECG
-
• Question 2: prolongation of the QTc interval by certain psychotropic medications may cause arrhythmias and lead to sudden death
-
• Question 3: 500 ms
Survey 2: monitoring of clinical practice of ECG
The second survey involved analysis of the case notes of 82 persons who had been in-patients for more than 1 week on four acute psychiatric wards in a National Health Service (NHS) hospital. The analysis recorded whether an ECG had been done, and if so whether the QTc interval had been documented. Notes were also investigated to reveal any of the risk factors for QTc prolongation mentioned earlier.
The standards chosen were combined from the Royal College of Psychiatrists report The Association Between Antipsychotic Drugs and Sudden Death (CR57), which was superseded in 2006 by College Report CR138 Consensus Statement On High-Dose Antipsychotic Medication; 12 the Maudsley 2005–2006 Prescribing Guidelines; Reference Taylor, Kerwin and Paton10 and the Medicines and Healthcare products Regulatory Agency (MHRA) recommendations Pharmacovigilance Working Party Public Assessment Report on Neuroleptics and Cardiac Safety, 13 and ranked by the authors (Box 2).
Results
Survey 1
There was a 100% response rate. Results for each of the three questions were 86%, 11% and 87% respectively incorrect.
Box 2. Standards for assessing ward practice in relation to measuring the QTc interval of high-risk individuals
Patients with one or more of the following risk factors were considered to be at risk of developing a prolonged QTc interval and therefore required an ECG.
-
• High-dose antipsychotic (dose above recommended British National Formulary values)
-
• More than one antipsychotic
-
• More than one psychotropic drug (antidepressants or mood stabilisers)
-
• Other significant drugs (non-psychotropic medication known to prolong QTc interval)
-
• Taking illicit drugs
-
• Diabetes
-
• Ischaemic heart disease
-
• Hypertension
-
• Other physical conditions known to predispose to torsade de pointes
Survey 2
The survey of clinical practice showed that of 82 patients, 15 patients (18%) were receiving high-dose antipsychotics – above levels recommended in the British National Formulary (BNF) 14 – and 26 patients (32%) were receiving more than one antipsychotic: 24 were receiving two antipsychotics and 2 patients were taking three antipsychotics. A total of 29 patients (35%) were receiving two psychotropic drugs (non-antipsychotics) and 3 patients (4%) were receiving three drugs, 2 patients (2%) were receiving four drugs and 1 patient (1%) was receiving five psychotropic drugs. It was also found that 6 patients (7%) were receiving one other non-psychotropic drug which has been considered significant in the causation of torsade de pointes, 3 patients (4%) were receiving two such drugs, and 2 patients (2%) were receiving three such drugs. Nine patients (11%) also tested positive for illicit drugs.
With regard to non-pharmacological risk factors for QTc prolongation, 6 (7%) patients had diabetes, 23 patients (28%) had ischaemic heart disease and 13 patients (16%) were found to have other medical conditions (i.e. not either of the former disorders) (Table 1).
Table 1. Prevalence of risk factors for the prolongation of the QTc interval in 82 psychiatric patients
| Risk factor1 | Patients, n (%) |
|---|---|
| High-dose antipsychotic | 15 (18) |
| More than one antipsychotic | 26 (32) |
| More than one psychotropic | 35 (43) |
| Other significant drugs | 11 (13) |
| Taking illicit drugs | 9 (11) |
| Diabetes | 6 (7) |
| Ischaemic heart disease | 10 (12) |
| Hypertension | 13 (16) |
| Other physical conditions | 13 (16) |
The results of this study divided the patients into four groups (Fig. 1): group A (n=41, 50%) consisted of patients who needed an ECG based on their risk factors (according to the above guidelines) yet did not receive one; group B (n=13, 16%) consisted of patients who had risk factors and were given an ECG; group C (n=5, 6%) consisted of patients who did not have any risk factor and received an ECG; group D (n=23, 28%) consisted of patients who did not have any risk factor and who also did not have an ECG. We found that only 7% (n=6) of the patients who received an ECG had a documented QTc measurement.
Discussion
Survey 1 revealed that junior doctors were lacking in knowledge regarding the QTc interval. This could be a potential cause of the inadequate monitoring of ECGs in high-risk patients on four acute psychiatric wards noted in Survey 2. Survey 1 revealed that the level of knowledge regarding the measurement of the QTc interval and its implications was unsatisfactory. With the exception of question 2, the majority of junior doctors surveyed did not know the implications of QTc.
Survey 2 showed that half of the studied patients who had an increased risk of developing a prolonged QTc interval had not had an ECG. One factor accounting for this might be that 86% of the doctors did not know what QTc was, although the majority knew the significance of a prolonged QTc in relation to psychotropic medication and specifically to antipsychotics. However, a cross-sectional survey cannot determine that there is a direct correlation with the knowledge of junior doctors or some other cause, e.g. poor or unavailable ECG service. There may also be other factors such as shortage of time for doctors to do an ECG, the unavailability of ECG machines on a psychiatric unit or ECGs being postponed owing to uncooperative patients. Similar findings have been reported by Warner et al, who conducted a survey of junior doctors in the UK and found that fewer than 20% were able to identify a prolonged QTc interval on an ECG. Reference Warner, Gledhill, Connell and Coghlan15
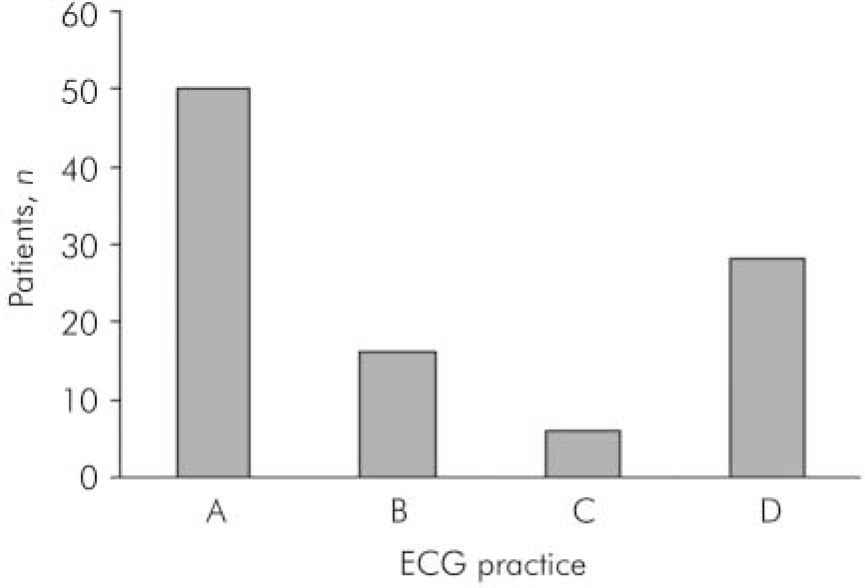
Fig. 1. Number of electrocardiograms (ECGs) performed on acute psychiatric wards. Group A required an ECG and did not get one; group B required an ECG and got one; group C did not require an ECG but still got one; group D did not require an ECG and did not get one.
Psychiatric patients have an increased risk of developing serious arrhythmias due to antipsychotic medication and other comorbidities such as ischaemic heart disease. Reference Cubeddu1 The QTc interval may be prolonged due to both pharmacological and non-pharmacological reasons. Prevention is the best strategy, and reducing the risk of QTc-associated arrhythmias must be set against the benefits of certain medications. It is important to note that there was a degree of overlap between different risk factors, introducing a spectrum of risk. For example, one patient was taking five psychotropic drugs including pipotiazine palmitate (maximum dose), quetiapine (above BNF recommended dose), haloperidol (therapeutic dose) and two mood stabilisers, but did not receive an ECG.
Recommendations
We found that the practice of monitoring ECGs in the four wards was inadequate. We must also be mindful of the potential legal implications of such practice. We have therefore outlined a series of recommendations, based on College Report CR138, the Maudsley 2005–2006 Prescribing Guidelines and MHRA recommendations, Reference Taylor, Kerwin and Paton10,12,13 to aid clinicians in the practice of monitoring patients at high risk of developing QTc interval prolongation.
-
• We recommend that all in-patients have a routine ECG, whether or not they have the documented risk factors outlined above, although careful assessment of their history and physical state should highlight those specifically at risk.
-
• Patients who are prescribed antipsychotics, having had a baseline ECG, should have a repeat ECG if doses are in the higher ranges or if they have other physical risk factors.
-
• If the QTc approaches 500 ms and continues to increase, specialist cardiological review should be obtained just as one would do if the patient were experiencing symptoms of cardiac ischaemia.
-
• There should be education for junior doctors on ECG interpretation.
-
• Clinicians should be aware that the risk of torsade de pointes following QTc prolongation is small, Reference Taylor16 thus a prolonged interval does not warrant an immediate withdrawal of therapy. However, it should serve to promote discussion between the patient and all parties involved in the patient's care, in which the risks and benefits of the treatment are examined.
-
• Many ECG machines do not measure the QTc interval, thus it is recommended that it should be calculated manually through the use of Bazett's formula: QTc=QT/√RR. Reference Bazett6 Although Bazett's formula is most commonly used, it is well understood that the QTc value is artificially prolonged at heart rates above 60 beats/min and reduced at heart rates below 60 beats/min. In addition, if the T waves are flat, broad or notched, the QTc interval can be difficult to calculate.
Limitations of our study
The results of this study may not generalise as we did not randomly select the studied doctors. In addition, they may not reflect practice in all UK hospitals as we used a convenience sample (the wards where we work). The authors’ subjective interpretation of the answers to the questions in the survey could potentially be viewed as biased. However, we believe that our criteria for assessing the responses to the survey were specific enough to rule out such bias. The number of patients taking illicit drugs, which is an independent risk factor for the prolongation of the QTc interval, may not reflect the actual numbers as not all of them had a urine drug screen. It is also important to note that electrolyte imbalance was not examined, although it is a significant risk factor.
Overall, we found that the monitoring of patients at high risk of developing potentially fatal tachyarrhythmias was inadequate. We suggest that these recommendations would increase the number of ECGs routinely conducted on patients in general psychiatric wards, and that this should be tested by a subsequent study. Our study implies that there need to be robust arrangements for ECG monitoring and that adherence to protocols could be monitored by a clinical pharmacist.
Declaration of interest
None.





eLetters
No eLetters have been published for this article.