Introduction
Recently, the psychosis phenotype has been widely characterized by psychotic experiences that are temporally and phenomenologically continuous with psychotic disorder. Supporting the notion of this extended psychosis phenotype, subclinical expressions of psychotic symptoms are prevalent in the general population (Linscott & van Os, Reference Linscott and van Os2013) and associated with an increased risk for developing a psychotic disorder (Fusar-Poli et al., Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rössler, Schultze-Lutter and Yung2013; Linscott & van Os, Reference Linscott and van Os2013). There is further evidence that subclinical psychotic experiences are associated with a family history of psychotic disorder (McGrath et al., Reference McGrath, Saha, Al-Hamzawi, Alonso, Bromet, Bruffaerts and Kessler2015), suggesting this extended phenotype reflects in part the distributed familial psychosis liability, which is often used as a proxy for genetic risk (although confounded by socio-environmental factors) (van Os, Rutten, & Poulton, Reference van Os, Rutten and Poulton2008). In recent years, studies have implicated a variety of different putative, psychological mechanisms that may be involved in the development and persistence of psychotic experiences in individuals with increased liability to psychosis (EU-GEI, 2014; Freeman & Garety, Reference Freeman and Garety2014; Garety, Bebbington, Fowler, Freeman, & Kuipers, Reference Garety, Bebbington, Fowler, Freeman and Kuipers2007; Howes & Murray, Reference Howes and Murray2014; Murray, Reference Murray2017; van Os, Kenis, & Rutten, Reference van Os, Kenis and Rutten2010; van Os et al., Reference van Os, Rutten and Poulton2008).
Elevated stress sensitivity is a psychological mechanism that has been widely studied in daily life using the Experience Sampling Method (ESM; Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007; Myin-Germeys et al., Reference Myin-Germeys, Oorschot, Collip, Lataster, Delespaul and van Os2009, Reference Myin-Germeys, Kasanova, Vaessen, Vachon, Kirtley, Viechtbauer and Reininghaus2018; Oorschot, Kwapil, Delespaul, & Myin-Germeys, Reference Oorschot, Kwapil, Delespaul and Myin-Germeys2009). Stress sensitivity has been conceptualized as increased negative affect and psychotic experiences in response to minor stressors in daily life and has been found in both individuals with an increased familial and psychometric risk for psychosis as well as individuals diagnosed with a psychotic disorder (Collip et al., Reference Collip, Nicolson, Lardinois, Lataster, van Os and Myin-Germeys2011; Lataster et al., Reference Lataster, Wichers, Jacobs, Mengelers, Derom, Thiery and Myin-Germeys2009; Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007; Myin-Germeys, van Os, Schwartz, Stone, & Delespaul, Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001; Palmier-Claus, Dunn, & Lewis, Reference Palmier-Claus, Dunn and Lewis2012; Reininghaus et al., Reference Reininghaus, Gayer-Anderson, Valmaggia, Kempton, Calem, Onyejiaka and Morgan2016b, Reference Reininghaus, Kempton, Valmaggia, Craig, Garety, Onyejiaka and Morgan2016c; van der Steen et al., Reference van der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons, Lardinois and Myin-Germeys2017). Also, several models propose that the effects of stress on psychotic experiences are partly mediated through experiences of affective disturbance (Garety et al., Reference Garety, Bebbington, Fowler, Freeman and Kuipers2007; Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007). Elevated emotional reactivity to minor stress was associated with more intense psychotic experiences in daily life in a group of patients with a first episode of psychosis when compared to healthy controls (Reininghaus et al., Reference Reininghaus, Kempton, Valmaggia, Craig, Garety, Onyejiaka and Morgan2016c; van der Steen et al., Reference van der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons, Lardinois and Myin-Germeys2017). Also, independently of stress, affective disturbance has been associated with psychotic experiences across different levels of psychosis liability (Bentall et al., Reference Bentall, Rowse, Shryane, Kinderman, Howard, Blackwood and Corcoran2009; Fowler et al., Reference Fowler, Hodgekins, Garety, Freeman, Kuipers, Dunn and Bebbington2012; Kramer et al., Reference Kramer, Simons, Wigman, Collip, Jacobs, Derom and Wichers2014; Thewissen et al., Reference Thewissen, Bentall, Oorschot, à Campo, van Lierop, van Os and Myin-Germeys2011; Varghese et al., Reference Varghese, Scott, Welham, Bor, Najman, O'Callaghan and McGrath2011). Elevated levels of negative affect, for instance, have been found to precede the experiences of paranoia in individuals with psychotic disorder, in individuals with increased psychometric risk (Thewissen et al., Reference Thewissen, Bentall, Oorschot, à Campo, van Lierop, van Os and Myin-Germeys2011) as well as in a general population twin sample (Lataster et al., Reference Lataster, Wichers, Jacobs, Mengelers, Derom, Thiery and Myin-Germeys2009).
However, to date, little data have been published on the reverse of the above suggested pathway. Psychotic experiences themselves may be seen as a source of distress and are commonly linked to disturbances in affect (Kelleher et al., Reference Kelleher, Wigman, Harley, O'Hanlon, Coughlan, Rawdon and Cannon2015; Klippel et al., Reference Klippel, Viechtbauer, Reininghaus, Wigman, van Borkulo, Myin-Germeys and Wichers2017b; van der Steen et al., Reference van der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons, Lardinois and Myin-Germeys2017). Affective disturbance may then be driving the appraisal of daily events, experiences and contexts as stressful. Psychotic experiences may, therefore, as well be seen as preceding, rather than being merely a consequence of, momentary stress. In line with this, recent work by Rapado-Castro, McGorry, Yung, Calvo, and Nelson (Reference Rapado-Castro, McGorry, Yung, Calvo and Nelson2015) suggests a link between subclinical psychotic experiences and distress in at-risk individuals. This, in turn, has been found to be associated with an increased risk of transition to psychosis (Kramer et al., Reference Kramer, Simons, Wigman, Collip, Jacobs, Derom and Wichers2014).
Although the body of literature on the link between minor daily stress, affective disturbances and psychotic experiences is growing, and several integrated models have been proposed (Howes & Murray, Reference Howes and Murray2014; Morgan, Charalambides, Hutchinson, & Murray, Reference Morgan, Charalambides, Hutchinson and Murray2010), to date, only little attention has been paid to how these processes combine in the formation of psychotic experiences in daily life. Using cross-sectional multilevel mediation models, a recent study by our group showed that minor daily stress increases psychotic experiences via pathways through affective disturbances (Klippel et al., Reference Klippel, Myin-Germeys, Chavez-Baldini, Preacher, Kempton, Valmaggia and Reininghaus2017a). This indirect effect was greater in individuals with an at-risk mental state and individuals with a first-episode psychosis than in healthy control subjects. In another recent study, we applied the network approach to psychopathology to elucidate the dynamic interplay of momentary experiences, contextual factors and psychotic experiences longitudinally (Klippel et al., Reference Klippel, Viechtbauer, Reininghaus, Wigman, van Borkulo, Myin-Germeys and Wichers2017b). Findings implied that affective disturbance had an intermediary position between minor daily stress and psychotic experiences.
The aim of the current study was twofold. First, we sought to investigate cross-sectionally how momentary stress and affective disturbance combine to increase the intensity of psychotic experiences in daily life, and vice versa, thereby aiming to replicate our previous findings (Klippel et al., Reference Klippel, Myin-Germeys, Chavez-Baldini, Preacher, Kempton, Valmaggia and Reininghaus2017a) in another population of individuals with increased familial liability to psychosis. Second, we attempted to test these pathways longitudinally, applying multilevel cross-lagged panel models. We used the ESM in three groups varying in their familial liability to psychosis: individuals with psychotic disorder, first-degree relatives of individuals with psychotic disorder and healthy control individuals. Specifically, the current study tested the following main hypotheses: in all three groups, (i) the cross-sectional effect of momentary stress on psychotic experiences is mediated by affective disturbance; (ii) the cross-sectional effect of psychotic experiences on momentary stress is mediated by affective disturbance; (iii) the longitudinal effect of momentary stress on psychotic experiences is mediated by affective disturbance; and (iv) the longitudinal effect of psychotic experiences on momentary stress is mediated by affective disturbance. We further hypothesized that all these indirect effects are greater in (a) individuals with psychotic disorder than in controls, (b) relatives than in controls and (c) individuals with psychotic disorder than in relatives.
Methods
Samples
We used data from six different studies (Collip et al., Reference Collip, Nicolson, Lardinois, Lataster, van Os and Myin-Germeys2011; Lataster et al., Reference Lataster, Collip, Ceccarini, Haas, Booij, van Os and Myin-Germeys2011a, Reference Lataster, Myin-Germeys, Wichers, Delespaul, van Os and Bak2011b; Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001; Thewissen, Bentall, Lecomte, van Os, & Myin-Germeys, Reference Thewissen, Bentall, Lecomte, van Os and Myin-Germeys2008; van der Steen et al., Reference van der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons, Lardinois and Myin-Germeys2017) included in the pooled Maastricht MERGE database (release number 4.5; see online Supplementary Table S1 for in- and exclusion criteria of these studies) that all used a similar ESM protocol. Participants were classified either as (i) ‘healthy’ control individuals (i.e., neither a personal diagnosis nor a family history of psychotic disorder/symptoms), (ii) first-degree relatives of individuals with a psychotic disorder or (iii) individuals with a psychotic disorder.
All studies included in this paper were approved by the local medical ethics committee. All further procedures and analyses were performed according to the ethical standards formulated by this committee.
Experience Sampling Method
In all studies, ESM (a structured diary technique) was used to study minor stress in everyday life (see Table 1) (Myin-Germeys et al., Reference Myin-Germeys, Kasanova, Vaessen, Vachon, Kirtley, Viechtbauer and Reininghaus2018). Individuals received a diary and a wristwatch, which was programmed to beep 10 times a day (between 7:30 h and 22:30 h) for 5 [Aripiprazol study (Lataster et al., Reference Lataster, Myin-Germeys, Wichers, Delespaul, van Os and Bak2011b)] or 6 days (remaining studies) at semi-random intervals (random within 90 min time frames). Thus, the time lag between the measurements was, on average, approximately 90 min. Further information on the ESM procedure and the variables used in the current study are presented in Table 1.
Table 1. ESM procedurea and measures of stress, negative affect and psychotic experiences
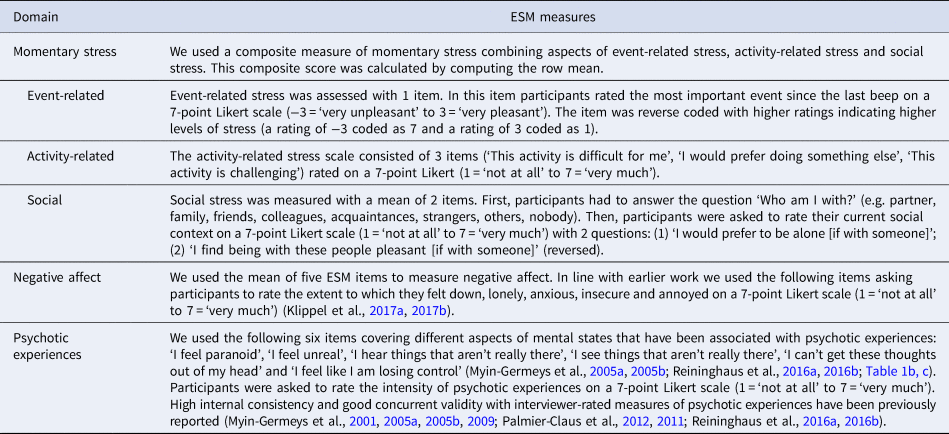
a ESM procedure: Over a period of six consecutive days, participants were equipped with a diary and a wristwatch which was programmed to give a signal 10 times a day. Participants were explained to stop their activity and respond to the above items when prompted by the beep signal as part of a comprehensive diary questionnaire assessing activities, feelings, thoughts, behaviours, social situations and surroundings in daily life. The assessment period started on any day of the week as selected by the participant and they were asked to note the time they filled out the ESM questionnaire. Participants also noted the time of the assessment. Reports completed later than 15 min after the signal were excluded from the analysis. In order to maximize the number of observations for every participant, participants were contacted at least once during the assessment period to assess instruction adherence, identify any concerns associated with the method and help participants with any problems in completing the ESM questionnaire. The participants' reactivity to and compliance with the method was assessed in a debriefing session at the end of the assessment period. In order to be included in the analysis, participants had to provide valid responses to at least one-third of the beep signals.
Statistical analysis
Data from ESM studies have a hierarchical structure with multiple observations nested within subjects. We therefore fitted multilevel moderated mediation models in Mplus, Version 7 (Muthén & Muthèn, Reference Muthén and Muthèn1998–2017), to control for within-subject clustering of multiple observations. We did this using the MLR and MLF estimators, which allowed us to use all available data under the relatively unrestrictive assumption that data are missing at random if all variables associated with missing values are included in the model (Preacher, Reference Preacher2015; Preacher, Rucker, & Hayes, Reference Preacher, Rucker and Hayes2007). We used a two-level model, where multiple observations (level-1) were treated as nested within subjects (level-2).
Cross-sectional multilevel moderated mediation models
The total effect of momentary stress in daily life (level-1) on the intensity of psychotic experiences (level-1) was apportioned into direct and indirect effects through negative affect using the product of coefficients strategy. With this strategy, we can quantify the point estimate of the indirect effect as the product of the coefficient of the independent variable on the mediator variable (path a) and the coefficient of mediator variable on the dependent variable (path b). Given its advantages over other methods in the context of multilevel mediation models, we used an R package by Selig and Preacher for computing Monte Carlo confidence intervals and assessing the statistical significance of indirect effects (Preacher & Selig, Reference Preacher and Selig2012; Preacher et al., Reference Preacher, Rucker and Hayes2007). Group (patients, relatives, controls) was used as the moderator variable (level-2) of direct and conditional indirect effects in all analyses. We did this based on a multilevel moderated mediation approach, where the moderator variable is the predictor of the a and b paths (see Fig. 1) and the strength of the indirect effect of the level-1 independent variable depends on the level-2 moderator variable (Bauer, Preacher, & Gil, Reference Bauer, Preacher and Gil2006; Preacher et al., Reference Preacher, Rucker and Hayes2007). By doing this, we could test whether conditional indirect effects were greater in (a) patients than in controls, (b) relatives than in controls and (c) patients than in relatives by computing differences in conditional indirect effects using the model constraint command in Mplus (Muthén & Muthèn, Reference Muthén and Muthèn1998–2017) and calculating respective Monte Carlo confidence intervals (Bauer et al., Reference Bauer, Preacher and Gil2006; Preacher & Selig, Reference Preacher and Selig2012; Preacher et al., Reference Preacher, Rucker and Hayes2007). Further, we calculated the proportion mediated, a widely used measure of effect size in mediation literature (MacKinnon, Fairchild, & Fritz, Reference MacKinnon, Fairchild and Fritz2007; Shrout & Bolger, Reference Shrout and Bolger2002), as the ratio of the indirect effect to the total effect.
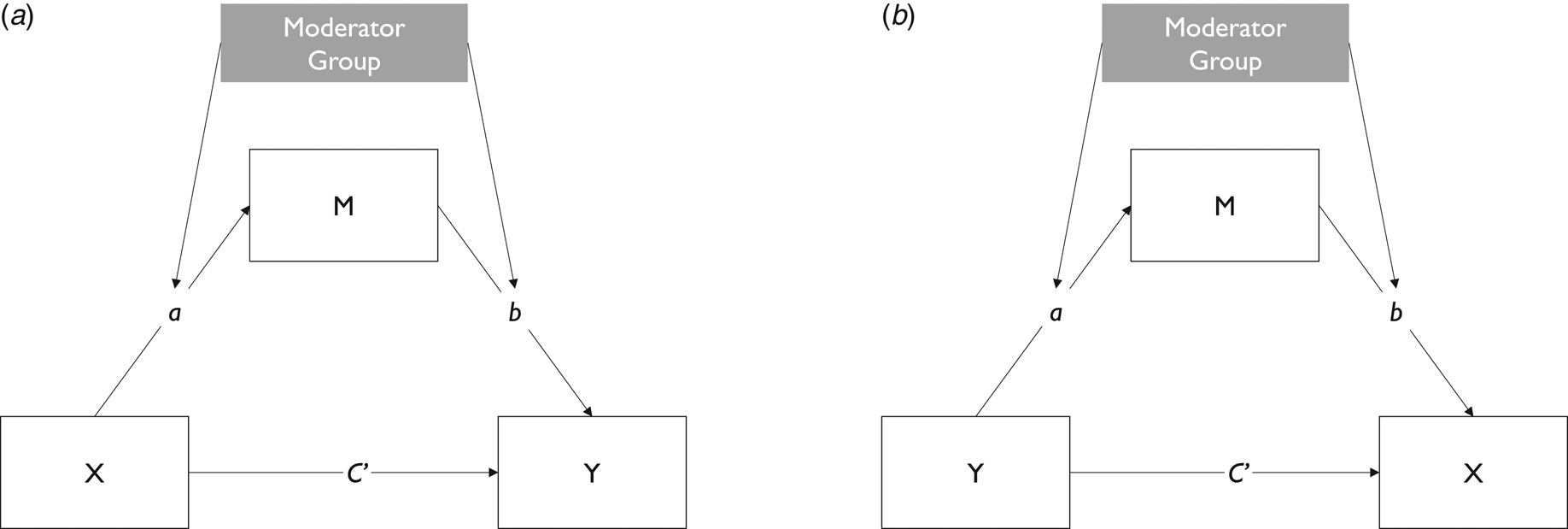
Fig. 1. Schematic display of cross-sectional moderated mediation models. Display of pathways tested within each group: (a) momentary stress (X) on psychotic experiences (Y) via negative affect (M); (2) psychotic experiences (Y) on momentary stress (X) via negative affect (M). All models were controlled for age and gender.
Longitudinal multilevel moderated mediation models
In a first step, we fitted an autoregressive model to estimate autoregressive effects of momentary stress at t−1 on momentary stress at t, negative affect at t−1 on negative affect at t and psychotic experiences at t−1 on psychotic experiences at t. In order to assess longitudinal mediation, we fitted a multilevel moderated cross-lagged panel model for a half-longitudinal design (CLPM) as proposed by Preacher (Reference Preacher2015) and estimated all covariances between random intercepts and random slopes. In a half-longitudinal design, an indirect effect of an independent variable (X) on a dependent variable (Y) via a mediator variable (M) is estimated using data of two measurement occasions (see Fig. 2). The total effect of momentary stress at t−1 on psychotic experiences at t was apportioned into direct and indirect effects of negative affect at t, again, using the product of coefficients strategy. Using this strategy, we can quantify the point estimate of the indirect effect as the product of the coefficient of the independent variable on the mediator variable (path a) and the coefficient of mediator variable on the dependent variable (path b). For example, the point estimate of the indirect effect of momentary stress (Xt −1) on psychotic experiences (Yt) through negative affect (Mt) is quantified as the product of the coefficient of momentary stress (Xt −1) on negative affect (Mt) (path axm, in Fig. 2c) and the coefficient of negative affect (Mt −1) on psychotic experiences (Yt) (path bmy, in Fig. 2c). In the same model, we proceeded likewise with the effect of psychotic experiences at t−1 on momentary stress at t via negative affect at t. Monte Carlo confidence intervals were computed for indirect effects according to the above-mentioned procedure (Preacher & Selig, Reference Preacher and Selig2012; Preacher et al., Reference Preacher, Rucker and Hayes2007). Group (patients, relatives, controls) was used as the moderator variable (level-2) of direct and conditional indirect effects in the analyses. Differences in conditional indirect effects between groups were subsequently computed using the model constraint command in Mplus (Muthén & Muthèn, Reference Muthén and Muthèn1998–2017). Prior to running this comprehensive model, we fitted two separate models: one with pathways from momentary stress to psychotic experiences through negative affect (Fig. 2a) and another one including pathways from psychotic experiences to momentary stress via negative affect (Fig. 2b).
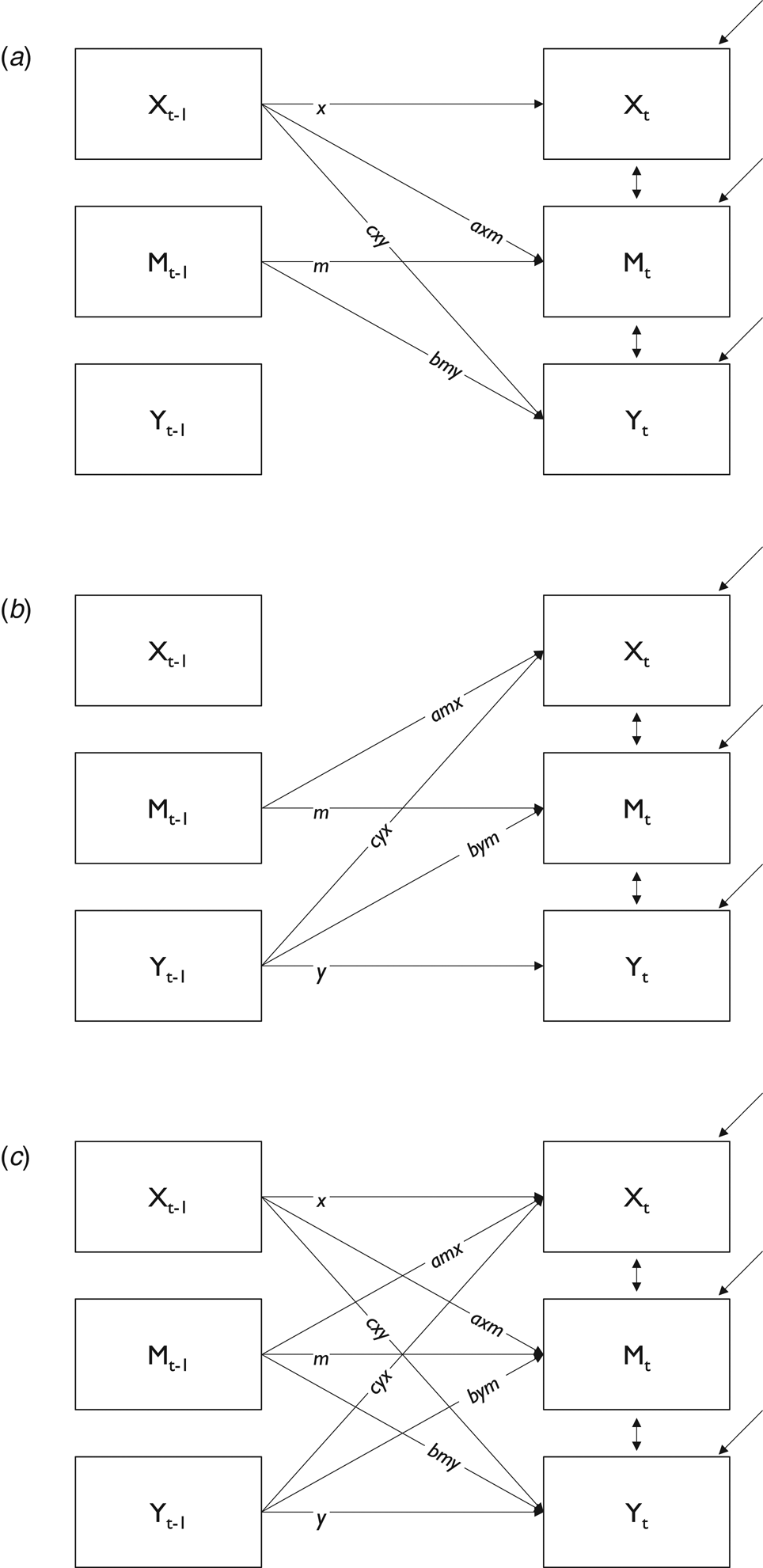
Fig. 2. Schematic display of cross-lagged panel models. Display of pathways tested within each group: (a) momentary stress at t−1 (Xt −1) on psychotic experiences at t (Yt) via negative affect at t (Mt); (b) psychotic experiences at t−1 (Yt −1) on momentary stress at t (Xt) via negative affect at t (Mt); (c) all pathways tested in one comprehensive model. All models controlled for age and gender.
Results
Basic sample characteristics
Basic sample characteristics and aggregate ESM scores for momentary stress, negative affect and psychotic experiences are presented in Table 2. Both patients and relatives differed significantly from controls in aggregate ESM scores for momentary stress, negative affect and psychotic experiences. Interestingly, aggregate momentary stress scores of relatives were similar to those of patients, whereas their aggregate scores of negative affect and psychotic experiences were more similar to controls.
Table 2. Sample characteristics and aggregate ESM scores for momentary stress, negative affect and psychotic experiences in patients, relatives and controls
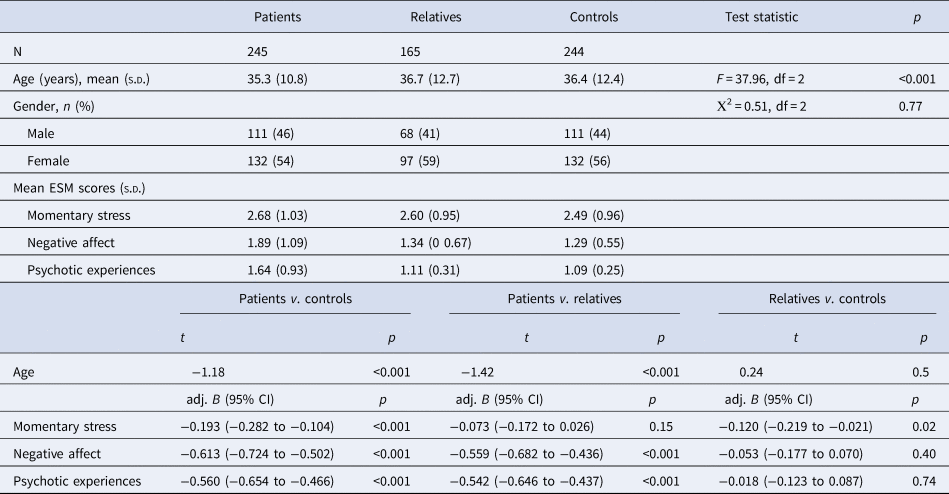
s.d., standard deviation; v., versus; CI, confidence interval.
Cross-sectional multilevel moderated mediation models
To examine pathways from momentary stress to psychotic experiences via negative affect and the reverse from psychotic experiences to momentary stress via negative affect, we fitted two separate multilevel moderated mediation models (Table 3). The indirect effect of momentary stress on the intensity of psychotic experiences via negative affect was statistically significant at conventional levels (p < 0.05) in all groups. This indicated that an increase in stress was associated with higher levels of negative affect, which, in turn, was associated with more intense psychotic experiences. The relative contribution of this indirect effect was larger than the contribution of the direct pathway from momentary stress to psychotic experiences, as indicated by the proportion mediated, which showed that the indirect effect of negative affect accounted for 69–86% of the total effect in patients and controls [PM exceeds 1.0 in relatives as direct effect is opposite in sign to the indirect effect (Shrout & Bolger, Reference Shrout and Bolger2002)]. Further, this indirect effect was significantly greater in patients than in controls [adj. B = 0.001; 95% CI (0.000–0.002)], weaker in relatives than in controls [adj. B = −0.014; 95% CI (−0.016 to −0.012)] and greater in patients than in relatives [adj. B = 0.015; 95% CI (0.013–0.017)].
Table 3. Total, direct and conditional indirect effects of cross-sectional multilevel moderated mediation models of stress, negative affect and psychotic experiences, vice versa a
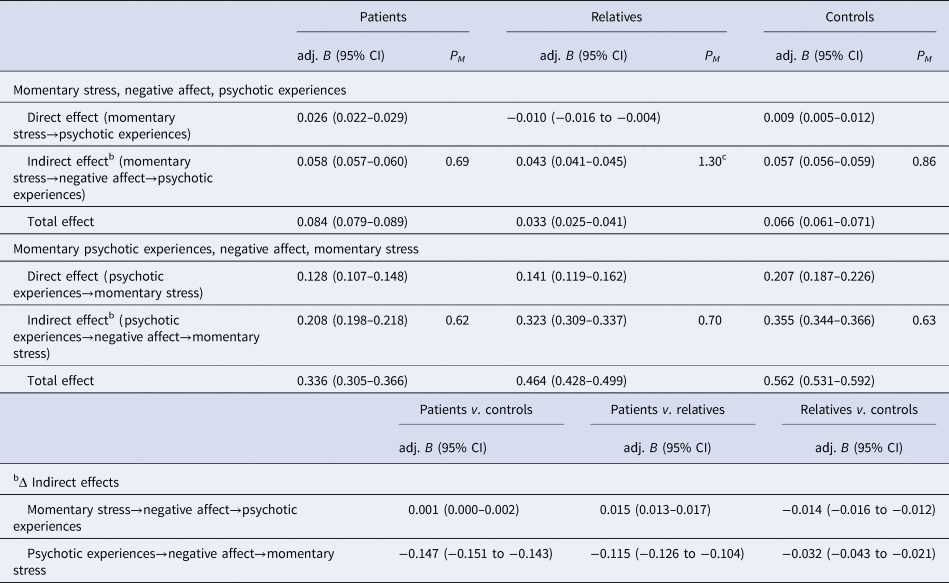
s.d., standard deviation; v., versus; CI, confidence interval; PM, proportion mediated.
a Adjusted for age and gender.
c Exceeds 1.0 in case of suppression effects [i.e., if direct effect is opposite in sign to the indirect effect (Shrout & Bolger, Reference Shrout and Bolger2002)].
Turning to the findings of psychotic experiences on momentary stress, there was evidence that the effect of psychotic experiences on momentary stress was significantly mediated by levels of negative affect in all three groups. Overall, the magnitude of these indirect effects was greater than those of reverse pathways (i.e., effects of stress on psychotic experiences via negative affect). The indirect effect was greatest in controls [adj. B = 0.355; 95% CI (0.344–0.366)], followed by relatives [adj. B = 0.323; 95% CI (0.309–0.337)] and then patients [adj. B = 0.208; 95% CI (0.198–0.218)]. Again, the relative contribution of this indirect effect was greater than the contribution of the direct effect from psychotic experiences to momentary stress, as this indirect effect accounted for 62–70% of the total effect. The indirect effect of psychotic experiences on momentary stress via negative affect followed a gradient across the three groups, i.e., it was weaker in patients than in controls [adj. B = −0.147; 95% CI (−0.151 to −0.143)], weaker in relatives than in controls [adj. B = −0.032; 95% CI (−0.043 to −0.021)] and weaker in patients than in relatives [adj. B = −0.115; 95% CI (−0.216 to −0.104)].
Longitudinal multilevel moderated mediation models
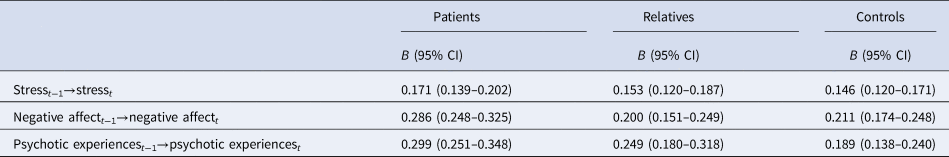
Model fit statistics are presented in online Supplementary Table S2. The comprehensive cross-lagged panel model showed a significantly better fit to the data than the autoregressive model or separate cross-lagged panel models. Results of the autoregressive model can be found in Table 4. Levels of momentary stress, negative affect and psychotic experiences at t−1 were significantly associated with levels at t (all p = 0.000).
Table 4. Autoregressive effects (t−1→t) of momentary stress, negative affect and psychotic experiences in patients, relatives and controls
When we examined the indirect effects of momentary stress on psychotic experiences, and vice versa, the indirect effects of psychotic experiences on momentary stress simultaneously in one longitudinal cross-lagged panel model with two time points, there was no evidence that the effect of momentary stress on psychotic experiences was mediated by negative affect in any of the three groups (Table 5).
Table 5. Total, direct and conditional indirect effects of longitudinal multilevel moderated mediation models of stress, negative affect and psychotic experiencesa
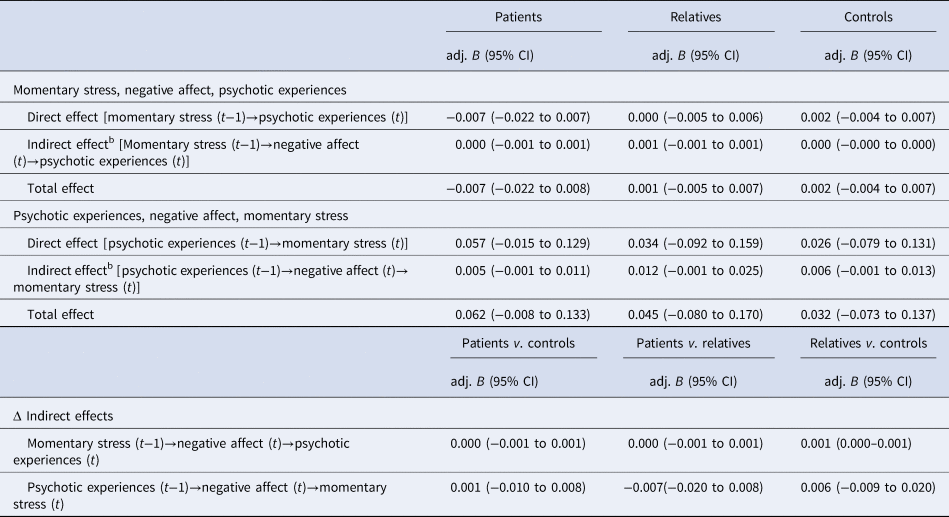
s.d., standard deviation; v., versus; CI, confidence interval.
a Adjusted for age and gender.
Discussion
Principal findings
It was the central aim of the current study to investigate how stress and affective disturbances combine to increase the intensity of psychotic experiences and to establish a temporal order thereof. We found that, cross-sectionally, an increase in stress was associated with higher levels of negative affect, which, in turn, was associated with more intense psychotic experiences consistently across the three groups. There was evidence of greater indirect effects of momentary stress on psychotic experiences in patients than both relatives and controls, with the weakest effects being evident in relatives. Cross-sectional modelling of data further indicated that the effects of psychotic experiences on momentary stress were mediated by the levels of negative affect in all three groups. The strength of this indirect effect differed significantly in all three groups, with the strongest effects being evident in controls, closely followed by relatives and, then, albeit weaker, patients. Hence, there was no consistent evidence from cross-sectional models that indirect effects increased as liability to psychosis increased. Longitudinal modelling of data, however, provided no evidence of temporal priority of stress and affective disturbances over psychotic experiences, or, vice versa, an indirect effect of psychotic experiences on stress by affective disturbances.
Methodological considerations
The current findings should be viewed in the light of potential limitations. First, longitudinal models in the current study did not yield evidence for longitudinal effects across two measurement occasions. As has been proposed by Shiffman, Stone and Hufford, in ESM research, it is important that assessment schemes fit the phenomenon of interest and the estimation of how rapidly it is expected to vary (Shiffman, Stone, & Hufford, Reference Shiffman, Stone and Hufford2008). In our study, lags between measurements were on average 90 min. Possibly, the effects of stress on psychotic experiences, and vice versa, may have been too transient to be lingering from one moment to the next. Another possibility is, that lag duration in the current study was too long to detect changes, that, in fact, may be there. One study by Vaessen et al. (Reference Vaessen, Viechtbauer, van der Steen, Gayer-Anderson, Kempton, Valmaggia and Myin-Germeys2019) showed that particularly patients in the early stages of psychosis may take longer to recover from stress. It would therefore be of interest to investigate whether reducing or increasing the duration of lags (i.e., the time between measurement occasions) would produce different findings. Future studies may further investigate the temporal interplay between stress, affective disturbances and psychotic experiences by systematically manipulating the time that passes between assessment points (Reininghaus, Depp, & Myin-Germeys, Reference Reininghaus, Depp and Myin-Germeys2016a). The results by Vaessen et al. (Reference Vaessen, Viechtbauer, van der Steen, Gayer-Anderson, Kempton, Valmaggia and Myin-Germeys2019) further beg the question whether findings from the current study would replicate in individuals with early psychosis.
Second, the magnitude of indirect effects of negative affect was comparable to previous studies (Klippel et al., Reference Klippel, Myin-Germeys, Chavez-Baldini, Preacher, Kempton, Valmaggia and Reininghaus2017a) and suggests evidence of partial mediation. This implies that there may be other unmeasured factors that are relevant in the pathways to psychosis.
Third, in the current study, we employed cross-sectional models as well as cross-lagged panel models of two measurement occasions to investigate how momentary stress and negative affect combine to increase psychotic experiences, and vice versa. Although fitting full cross-lagged panel models of three measurement occasions as described by Preacher (Reference Preacher2015) would have been a natural next step, we deem it unlikely that these models would have yielded evidence on temporal order given there was no evidence on this in cross-lagged panel models of two measurement occasions and the magnitude of indirect effects was very small and, for some, even trivial. However, this may be an important extension in the modelling strategy for future research.
Fourth, despite a number of benefits, pooling data from six different ESM studies may possibly entail disadvantages and may have produced a certain heterogeneity within the three groups of our sample. However, study protocols, in- and exclusion criteria were reviewed carefully before combining the six datasets. All studies employed comparable ESM protocols, using watches and booklets, on six (in one study five) consecutive days. Also, the in- and exclusion criteria for patients, relatives and controls (see also online Supplementary Table S1) were comparable across the combined studies. We therefore believe that the heterogeneity has been kept to a minimum in the current study and may not provide a problem.
Fifth, ESM measures are based on subjective reports of participants and may therefore be less reliable, since for example, not all subjects may interpret questions in the same way. In addition, ESM data collection can be very time-intensive and possibly be associated with assessment burden. Previous research, however, has shown that the ESM is a feasible, reliable and valid assessment method in a variety of different populations (Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001, Reference Myin-Germeys, Oorschot, Collip, Lataster, Delespaul and van Os2009, Reference Myin-Germeys, Kasanova, Vaessen, Vachon, Kirtley, Viechtbauer and Reininghaus2018; Palmier-Claus et al., Reference Palmier-Claus, Dunn and Lewis2012; Rauschenberg, van Os, Goedhart, Schieveld, & Reininghaus, Reference Rauschenberg, van Os, Goedhart, Schieveld and Reininghaus2020; Reininghaus et al., Reference Reininghaus, Kempton, Valmaggia, Craig, Garety, Onyejiaka and Morgan2016c). Also, in all of the combined six studies, participants were extensively briefed on the ESM by a trained researcher prior to start of data collection, to ensure correct interpretation of the employed items and proper use of the data booklet and preprogrammed watch (Collip et al., Reference Collip, Nicolson, Lardinois, Lataster, van Os and Myin-Germeys2011; Lataster et al., Reference Lataster, Myin-Germeys, Wichers, Delespaul, van Os and Bak2011b; Lataster, Valmaggia, Lardinois, van Os, & Myin-Germeys, Reference Lataster, Valmaggia, Lardinois, van Os and Myin-Germeys2013; Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001; Thewissen et al., Reference Thewissen, Bentall, Lecomte, van Os and Myin-Germeys2008; van der Steen et al., Reference van der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons, Lardinois and Myin-Germeys2017).
Comparison with previous research
In recent years, elevated reactivity to momentary stress has been suggested to reflect an important putative underlying mechanism in psychotic disorders (Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007; Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001; Palmier-Claus et al., Reference Palmier-Claus, Dunn and Lewis2012; Reininghaus et al., Reference Reininghaus, Kempton, Valmaggia, Craig, Garety, Onyejiaka and Morgan2016c). In line with this, individuals with an increased risk for psychosis have been found to experience elevated levels of reactivity to minor stressors in daily life (Collip et al., Reference Collip, Nicolson, Lardinois, Lataster, van Os and Myin-Germeys2011; Devylder et al., Reference Devylder, Ben-David, Schobel, Kimhy, Malaspina and Corcoran2013; Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001; Palmier-Claus et al., Reference Palmier-Claus, Dunn and Lewis2012). This has previously been coined the affective pathway to psychosis (Kramer et al., Reference Kramer, Simons, Wigman, Collip, Jacobs, Derom and Wichers2014; Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007). When turning to stress in more general terms, different models of psychosis have posited that the effects of stress are mediated by affective disturbance (Garety et al., Reference Garety, Bebbington, Fowler, Freeman and Kuipers2007; Howes & Murray, Reference Howes and Murray2014; Morgan et al., Reference Morgan, Charalambides, Hutchinson and Murray2010). A recent study by our group provided new evidence for this proposition and found that the cross-sectional effects of momentary stress on psychotic experiences were indeed mediated by affective disturbances in daily life across different stages along the psychosis continuum (Klippel et al., Reference Klippel, Myin-Germeys, Chavez-Baldini, Preacher, Kempton, Valmaggia and Reininghaus2017a). Our findings from cross-sectional models replicate these earlier findings suggesting that the effect of stress on psychotic experiences is mediated through affective disturbance, but, in contrast to what we hypothesized, there was no evidence that this indirect effect increased as familial liability to psychosis increased. What is more, in the reverse model, there was a gradual increase of the indirect effect of psychotic experiences on momentary stress via affective disturbance as familial liability decreased, with patients showing the weakest indirect effect. This may in part reflect the effects of illness chronicity or long-term exposure to antipsychotic medication on how strongly psychotic experiences impact the appraisal of events, activities and social situations as stressful via low mood. Finally, there was no evidence from longitudinal cross-lagged panel models that the indirect effects of momentary stress on psychotic experiences were mediated via affective disturbance.
It has been proposed that psychotic experiences themselves may be distressing (Kelleher et al., Reference Kelleher, Wigman, Harley, O'Hanlon, Coughlan, Rawdon and Cannon2015; van der Steen et al., Reference van der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons, Lardinois and Myin-Germeys2017; Wigman et al., Reference Wigman, Vollebergh, Raaijmakers, Iedema, van Dorsselaer, Ormel and van Os2011; Yung et al., Reference Yung, Buckby, Cotton, Cosgrave, Killackey, Stanford and McGorry2006), and in many cases, it is the experience of distress with symptoms that leads individuals to contact mental health services (Freeman & Garety, Reference Freeman and Garety2003). In the current study, we investigated whether psychotic experiences are associated with affective disturbance, which in turn are linked to increases in the experiences of momentary stress. To our knowledge, so far, there is no study that examined this pathway in its entirety in daily life. We found that the effects of psychotic experiences on momentary stress were mediated by negative affect, but these indirect effects did not increase as psychosis liability increased, with patients and, in fact, controls showing the largest effects. Interestingly, the magnitude of indirect effects in this cross-sectional pathway was considerably larger than those of the reverse pathway (from momentary stress to psychotic experiences via affective disturbance). This may tentatively suggest a greater impact of psychotic experiences on stress via negative affect than of stress on psychotic experiences through negative affect. Based on our findings, we can hypothesize that the occurrence of psychotic experiences may alter the appraisal of stress in daily life via experiences of affective disturbance. We believe that this pathway should receive more attention in future ESM studies in order to improve our understanding of the momentary impact that psychotic experiences may have on the individual.
The present work also aimed to investigate whether momentary stress takes temporal priority in exerting its indirect effects on psychotic experiences via affective disturbances to test recently proposed affective pathways to psychosis. As we did not find evidence on indirect temporal effects of momentary stress on psychotic experiences via affective disturbances, or vice versa, these findings suggest that, consistent with Kramer et al. (Reference Kramer, Simons, Wigman, Collip, Jacobs, Derom and Wichers2014), the temporal interplay of stress, affective disturbance and psychotic experiences may be more complex still than was hypothesized and modelled in the current study. Hence, the role of mediating and synergistic effects (and, in fact, mediated synergy) needs to be investigated jointly with other relevant aetiological factors as an important next step. Investigating temporal interplay in daily life is important as a basis for real-time and real-world interventions, such as Ecological Momentary Interventions (EMI; Heron & Smyth, Reference Heron and Smyth2010; Myin-Germeys, Klippel, Steinhart, & Reininghaus, Reference Myin-Germeys, Klippel, Steinhart and Reininghaus2016; Myin-Germeys et al., Reference Myin-Germeys, Kasanova, Vaessen, Vachon, Kirtley, Viechtbauer and Reininghaus2018; Reininghaus, Reference Reininghaus2018). Relatives of patients with a psychotic disorder have an increased risk for developing the disorder themselves (Kendler & Diehl, Reference Kendler and Diehl1993) and have been reported to show increases in the intensity of subtle psychotic experiences and affective disturbance in response to momentary stress (Myin-Germeys, Delespaul, & van Os, Reference Myin-Germeys, Delespaul and van Os2005a; Myin-Germeys, Marcelis, Krabbendam, Delespaul, & van Os, Reference Myin-Germeys, Marcelis, Krabbendam, Delespaul and van Os2005b). The findings of the current study may, however, point towards a certain resilience in relatives of patients. Both relatives and patients showed similar aggregate levels of momentary stress that were higher than those experienced by controls. However, when looking at aggregate levels of negative affect and psychotic experiences, these were similar in relatives and controls and significantly lower than those of patients. Furthermore, relatives showed the smallest magnitude of indirect effects when compared to the other two groups. Based on these findings, we may speculate that, although relatives experience levels of momentary stress similar to those of patients in everyday life, these are linked to a smaller increase in negative affect and psychotic experiences. Our findings do not support the hypothesis that familial liability modifies how stress impacts psychotic experiences via affective disturbance, which has been proposed previously (Lataster, Collip, Lardinois, van Os, & Myin-Germeys, Reference Lataster, Collip, Lardinois, van Os and Myin-Germeys2010; Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007; Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001).
Conclusion
Taken together, we found no evidence to support the temporal priority of momentary stress over affective disturbance and psychotic experiences, vice versa. However, findings from cross-sectional models may tentatively suggest a rapid vicious cycle of stress impacting psychotic experiences, and vice versa, via affective disturbances. This, in turn, highlights the importance of investigating reciprocal effects between these aspects in future studies. The question, then, remains, whether more rapid cycling of stress, affective disturbances and psychotic experiences may contribute to the persistence of psychotic experiences over time. This would, in turn, open new avenues for identifying and targeting the dynamics of these basic psychological dimensions in daily life and allow for clinical translational research using novel, personalized EMI (Myin-Germeys et al., Reference Myin-Germeys, Klippel, Steinhart and Reininghaus2016; Reininghaus et al., Reference Reininghaus, Depp and Myin-Germeys2016a) for targeting these dynamics in the early stages of developing psychotic experiences to prevent their transformation into full-blown psychotic symptoms.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720004894.
Acknowledgements
We would like to thank all researchers that substantially contributed to the conception and design of the included experience sampling studies and/or contributed to compile and check the data in this combined ESM dataset. In alphabetical order: M. Bak, D. Collip, N. Nicolson, I. Myin-Germeys, N. Geschwind, C. Henquet, N. Jacobs, M. Janssens, M. Lardinois, J. Lataster, T. Lataster, C. Menne-Lothmann, M. van Nierop, M. Oorschot, C.J.P. Simons, V. Thewissen and M. Wichers. We also thank all research personnel that provided general administrative support in preparing the ESM dataset, in particular T. Driesen.
Financial support
Ulrich Reininghaus was supported by a DFG Heisenberg professorship (no. 389624707). Annelie Klippel was supported by an ERC consolidator grant to Inez Myin-Germeys (ERC-2012-StG, project 309767 – INTERACT). Inez Myin-Germeys was supported by an FWO Odysseus grant (G0F8416N). Thomas Vaessen was supported by an FWO junior postdoctoral fellowship (ZKD6724).
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.










