The economic and social burden of non-communicable diseases attributable to poor diet is substantial( Reference Beaglehold, Bonita and Horton 1 ). Compelling evidence associates excess dietary Na with raised blood pressure( Reference He and MacGregor 2 ), a preventable major risk factor for CVD which accounts for 34 % of all deaths( 3 ). Almost a third of Australian adults have diagnosed hypertension (140/90 mmHg)( 4 ) but health risks increase before reaching this blood pressure threshold( Reference Neal 5 ).
Reducing blood pressure and the incidence of CVD around the world using programmes to lower population salt intake is a priority of the WHO( Reference Beaglehold, Bonita and Horton 1 ). As 75–80 % of dietary salt in most Western diets comes from processed foods( Reference Brown, Tzoulaki and Candeias 6 ), one component of many national strategies to reduce population salt intakes has been working with the food industry to reduce salt in processed foods( Reference Webster, Dunford and Hawkes 7 ) and many countries have implemented voluntary Na reduction targets for major food categories. The UK( 8 ), USA( 9 ) and Canada( 10 ), for example, have each established more than sixty food Na reduction targets. In Australia, the Australian Food and Health Dialogue (FHD), a joint government–industry–public health initiative( 11 ), has announced targets for seventeen food types in eight food categories.
Australians consume about 9 g salt/d (2800–4800 mg Na/d)( Reference Strazzullo, D'Elia and Kandala 12 , Reference Keogh and Clifton 13 ), which is much higher than physiological needs( Reference Brown, Tzoulaki and Candeias 6 , Reference He and MacGregor 14 ). Hidden sources of salt in processed foods make it difficult for consumers to follow dietary guidelines( 15 ) when much of the average Australian's diet is comprised of processed foods. Bread, cereal and cereal-based products provide 49 %, meat and meat products 21 %, milk products and dishes 5 % and savoury cooking sauces and condiments 8 %( Reference Webster, Dunford and Huxley 16 ) of salt intake from processed foods. Pasta sauces account for 75 % of all savoury cooking sauces sold in Australian supermarkets( 17 ).
The 2012 UK Na reduction target for pasta sauce products is a mean of 330 mg/100 g( 8 ), and responsibility for the target was transferred from the Food Standards Agency (FSA) to the Public Health Responsibility Deal for England (Responsibility Deal) in March 2011( 18 ). The USA( 9 ) and Canada( 10 ) have set sales-weighted reduction targets: 330 mg Na/100 g by 2014 in the USA and 320 mg Na/100 g with a maximum level of 520 mg Na/100 g for any individual pasta sauce product by 2016 in Canada. The FHD commitment for pasta sauces announced in April 2011 uses neither a sales-weighted mean nor a maximum target. Instead it has set an ‘action point’ of 420 mg Na/100 g and asks all manufacturers to voluntarily reduce the Na in any pasta sauce product with more than 420 mg/100 g in 2011 by 15 % by the end of 2014. In addition, for market leaders with leading products already below 420 mg Na/100 g, manufacturers are encouraged to ‘seek opportunities’ to further reduce Na levels( 19 ).
Monitoring Na reduction strategies is required to provide evidence that companies have reformulated their products and can be done by industry self-reports( 19 , 20 ), submission of sales data and recipes( 19 ) and use of food composition database(s)( 21 ). Recent studies, based on food composition tables, have analysed the Na content of foods available in Australia( Reference Dunford, Eyles and Mhurchu 22 – Reference Christoforou, Dunford and Neal 25 ) and have included foods such as bread( Reference Dunford, Eyles and Mhurchu 22 ) that are significant contributors of Na to the diet. None, however, report specifically on pasta sauce products or project the FHD commitment. The temporal nature of the FHD commitment for pasta sauces provided a window of opportunity to project the mean Na content of the FHD commitment for this food type. The last published mean Na content of Australian pasta sauces, which also included pesto products, was 499 mg/100 g in 2008( Reference Webster, Dunford and Neal 26 ). In comparison, 2009 data from the UK, for tomato pasta sauce products, showed a mean value of 320 mg Na/100 g( 27 ). The primary objective of the present study was to assess the change in Na levels of Australian pasta sauce products by comparing 2008 and 2011 Na content. A secondary objective was to project the mean Na content of these same products in 2014 using the FHD Na commitment and compare projections with the 2012 UK Na target for pasta sauce.
Methods
A systematic survey of the Na content of Australian pasta sauce products available in Australian supermarkets was undertaken in 2008 and 2011.
Products included
Pasta sauce products included were defined as ambient or fresh, where ambient products were those stored at room temperature and fresh products those requiring chilled storage. The definition included sauces that constitute a major part of a meal, and that are usually added to pasta, meat or vegetables and then heated.
Data collection
For each of the years 2008 and 2011, data were collected between July and September from the same five leading grocery stores (Coles, Woolworths, ALDI, IGA, Franklins) in Sydney, Australia. For each pasta sauce product, the manufacturer, brand and product name, as well as the Na content per 100 g were recorded. Data were obtained directly from the mandatory Nutrition Information Panel but where exactly the same product was for sale in more than one supermarket, it was recorded only once. Likewise, where the same product was presented in different pack sizes, only one entry was recorded. Data were entered into The George Institute's branded food composition database( 21 ) according to standardized methodology( Reference Dunford, Webster and Metzler 28 ). Data were screened to identify outliers and in each of the years a random selection of 5 % of the pasta sauce records was generated and data relating to Na content and brand were verified with the original Nutrition Information Panel. Outliers and missing values were identified and discrepancies were followed up with the manufacturer directly, on the manufacturer website, or by verification against the original Nutrition Information Panel data.
Grouping of manufacturers into types
Manufacturers were grouped by type using percentage volume share available in the 2009 edition of Retail World's Australasian Grocery Guide ( 29 ). The groupings of manufacturer type were: ‘supermarket own label’ (private label products with a total of 9 % volume share)( 29 ); ‘leading manufacturers’ (based on the top three national branded manufacturers who between them had almost 80 % volume share)( 29 ); ‘other manufacturers’ (included national branded manufacturers with approximately total 5 % volume share of pasta sauces)( 29 ).; and ‘boutique manufacturers’ (new, small, independent entrants to the pasta sauce category with an assumed small market share).
Data analysis
The mean, median, range and standard deviation for Na in pasta sauces (mg Na/100 g) were calculated overall, by type of pasta sauce, by manufacturer and manufacturer type for 2008 and 2011 using IBM SPSS Statistics Version 19·0. The means for ambient, fresh and total pasta sauces were compared between years using Student's unpaired t test and where the same products were present in both years using Student's paired t test. A two-sided P value of <0·05 was taken as significant. The percentage of products with Na levels greater than the ‘action point’ was identified for 2008 and 2011. Likewise, the percentage of products meeting the 2012 UK Na target for pasta sauces of 330 mg/100 g was also calculated.
A 2011 baseline was established upon which to project the FHD commitment. The products above 420 mg Na/100 g in 2011 were identified and the FHD target of a 15 % reduction was applied to project a 2014 mean (scenario 1). In addition, to assess the potential impact of the FHD commitment for market leaders to seek opportunities and reduce Na in leading products already below 420 mg Na/100 g, a reduction of 15 % was also applied to all products from leading manufacturers with less than 420 mg Na/100 g in 2011 (scenario 2). The projected mean Na values for the 2014 FHD commitment were compared against the 2012 UK Na target for pasta sauce.
Results
Na data were available for 124 pasta sauce products in 2008 and 187 in 2011. Of these, twenty-five were the same products present in both years with the remainder present only in one year or the other. The great majority of products in both years were classified as ambient pasta sauces (86 %). Of the 159 ambient products for sale in 2011, other manufacturers and boutique manufacturers provided approximately 15 % each, supermarket own label 24 % and leading manufacturers 43 %. Overall the data were normally distributed. The mean Na content for all pasta sauces in 2011 was 423 mg/100 g and in 2008, 451 mg/100 g (P = 0·16; Table 1), with a similar pattern observed for the ambient and fresh subsets. There were no significant differences in the mean Na content for products present in 2008 and 2011 (439 mg/100 g v. 435 mg/100 g; P = 0·83) or for products present in only 2008 or 2011 (454 mg/100 g v. 422 mg/100 g; P = 0·13).
Table 1 Changes in the sodium content of pasta sauces overall and by category in Australia between 2008 and 2011; data collected from five leading grocery stores in Sydney, Australia, in July–September of 2008 and 2011

*P value describing mean Na difference between 2008 and 2011 derived from two-sided unpaired t test.
†Food and Health Dialogue (FHD) action point of >420 mg Na/100 g.
‡UK Food Standards Agency (FSA) 2012 target (average) of 330 mg Na/100 g.
There were no detectable differences in the average Na levels between 2008 and 2011 for products produced by any of the different manufacturer types. The more detailed examination of modifications to the Na content of pasta sauces by individual manufacturers showed divergent patterns with Mars, for example, reducing mean Na levels by 16 % (P = 0·020) but Woolworths increasing by 94 % the mean Na content in its products from 265 mg/100 g to 513 mg/100 g (P < 0·0 0 1) over the same period. In contrast, the 2011 mean for Coles (287 mg Na/100 g) was almost half that of Woolworths.
Projected impact of the Food and Health Dialogue commitment to reduce Na in pasta sauce products and a comparison of the results with the 2012 UK target
When a 15 % reduction was applied to the ninety-seven pasta sauce products exceeding 420 mg Na/100 g (scenario 1), the projected total category mean for 2014 was 381 mg Na/100 g compared with the baseline of 423 mg Na/100 g (Table 2 and Fig. 1). This represents a projected overall 10 % Na reduction in pasta sauces from 2011 to 2014, but leaves Australian pasta sauces an average 51 mg/100 g (15 %) higher in Na than was proposed for UK pasta sauces in 2012. The projected mean was almost unchanged (375 mg Na/100 g) when an additional 15 % reduction was applied to the products of leading manufacturers with Na levels in 2011 already below the 420 mg Na/100 g action point (scenario 2). The projected range of Na levels for Australian pasta sauces in 2014 was 31–1020 mg/100 g.
Table 2 Projected sodium content (mean and range) for pasta sauces by manufacturer type and expectation that the UK 2012 pasta sauce target will be met by Australia in 2014
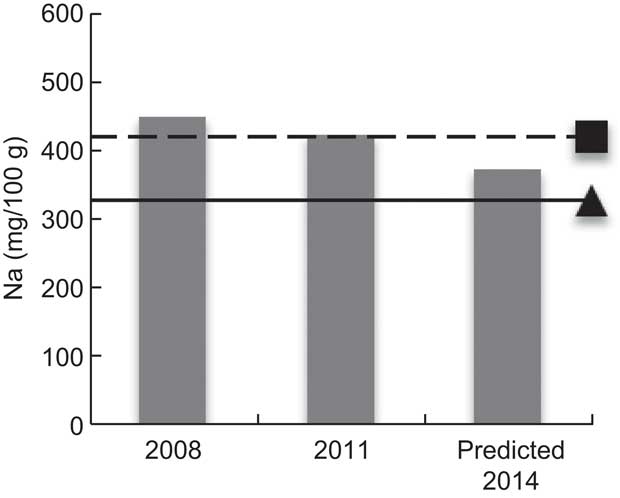
Fig. 1 Mean sodium content (![]() ) of all pasta sauces in five leading grocery stores in Sydney, Australia, in July–September of 2008 and 2011, and projection for 2014 measured against the Food and Health Dialogue (FHD) commitment of a 15 % reduction for 2014 (– – – ▪, FHD action point) and the 2012 UK target set by the Food Standards Agency (—— ▴)
) of all pasta sauces in five leading grocery stores in Sydney, Australia, in July–September of 2008 and 2011, and projection for 2014 measured against the Food and Health Dialogue (FHD) commitment of a 15 % reduction for 2014 (– – – ▪, FHD action point) and the 2012 UK target set by the Food Standards Agency (—— ▴)
In 2008 and 2011 almost three-quarters of products exceeded the UK target of 330 mg Na/100 g, and for Australian products to achieve the 2012 UK target by 2014 would require an across-the-board 22 % reduction from 2011 levels. Approximately half of Australian products that did meet the UK target in 2011 were supplied by boutique manufacturers and the 2011 mean Na value for this manufacturer type (325 mg/100 g) was already below the 2012 UK target (Table 2). The mean Na values for all three other manufacturer types were substantially higher.
Discussion
Na levels in Australian pasta sauces are high and the strategy to reduce them is projected to have little impact. Despite manufacturers responsible for 85 % of Australian market share participating( 19 ) and voluntarily signing up to the government's plan, it is projected that only a 10 % (42 mg Na/100 g) reduction will be achieved by 2014. As an Australian Federal Government initiative, the Executive of the FHD is chaired by the Parliamentary Secretary for Health and Ageing( Reference Appelqvist, Lundin and Margetts 30 ). Government leadership has been identified as one requirement for successful food reformulation initiatives( Reference Webster, Dunford and Huxley 16 ). Success, however, can be tempered by food industry lobbying to influence government-led voluntary food reformulation strategies in favour of food industry interests, which can include lack of transparency or rigour in target setting and monitoring( Reference Lawrence 31 , Reference O'Neill 32 ).
Target setting and monitoring
The FHD has adopted the principle of establishing salt reduction targets, but the method of implementation requires improvement. When done properly, a target-setting process can provide a much-needed level playing field for industry( Reference Webster, Dunford and Hawkes 7 ) and an indisputable benchmark against which progress can be tracked.
A level playing field requires absolute, quantitative targets, such as those introduced in the UK( 8 ) which encourage larger Na reductions in the saltiest products. On the other hand, the Australian approach of a single 15 % reduction for products above 420 mg Na/100 g before the end of 2014 allows the highest Na products to remain as such and creates an unfair competitive advantage based on taste, given the preference for a salty taste being a key driver of food choice( Reference Liem and Miremadi F & Keast 33 ). Our projections for 2014 show that the FHD commitment may deliver reductions that are only a fraction of those targeted for the UK and that those lesser reductions are likely to lag behind Na reduction efforts in the UK. There is a striking commonality between pasta sauce products in the UK and Australian markets, but Na reduction has been on the UK government agenda since 2003. The UK first introduced national voluntary targets in 2006, and other countries( 9 , 10 ) have drawn from the strengths of the UK strategy. The FHD commitment to Na reduction is more recent but may benefit by considering the strengths of other approaches. Multiple reductions of 10–15 % can re-set population levels of salt perception and largely go unnoticed by consumers( Reference Liem and Miremadi F & Keast 33 ). Reduction by stealth was exemplified by Project Neptune( 34 ), led by the Food and Drink Federation, in collaboration with government and public health, and targeted a 30 % Na reduction in UK ambient cooking and pasta sauces between 2003 and 2006 (10 % per year). Independent market research data (2006–2007) reported a 29 % reduction( 34 ). If the same 30 % reduction target, spread over three years, was adopted by the FHD, the overall projected mean Na value in 2014 would be 296 mg/100 g and directly comparable to the level already achieved by Australia's boutique manufacturers and Coles. In this way the food industry could continue to provide time-poor consumers lacking cooking skills or the inclination to cook( Reference Lang and Caraher 35 , Reference Caraher, Baker and Burns 36 ) with convenience products like pasta sauces without them being significantly detrimental to health.
Methods used to monitor reformulation strategies also differ between countries. However, inadequate rigour in the implementation of many monitoring systems weakens the evidence base and any subsequent conclusions that can be drawn from it. The UK FSA( 20 ) used a variety of monitoring methods including commitment tables, industry self-report against commitments, and food composition databases. Pledges and annual industry self-report are similarly used by the Responsibility Deal( 19 ), making it possible to see which companies have pledged to reduce Na and what percentage of their products meet the UK 2012 target. The FHD cites industry self-report and reporting of sales/recipes at pre-agreed intervals( 19 ), but to date( 11 , 19 ) has not published results in a way that would hold companies publicly accountable for the Na reduction commitment they have made to Australians.
Public health nutrition and profit
All companies need to be financially viable to be sustainable and provide employment. However, many people, including academics and health professionals( Reference He and MacGregor 14 , Reference Brownell 37 – Reference Moodie, Stuckler and Monteiro 39 ), are questioning the addition of large quantities of salt (along with saturated fat and sugar) as a mechanism for delivering profit at the expense of nutritional content and health outcome. Salt is required for processing, preservation and sensory perception( Reference Hutton 40 ) yet when used in excess, some argue, allows for cheaper ingredients and prolonged shelf-life, tactics that can reduce the cost of goods at the expense of health( Reference He and MacGregor 14 ). Our study provides no evidence to support or refute this argument. However, it does provide evidence that companies have not systematically reformulated to reduce the Na content of products between 2008 and 2011.
A comprehensive approach to target setting and strong government leadership has the potential to provide traction across the food supply and lower barriers to reformulation. Cost is one such barrier, and the cost to reformulate can vary widely but typically includes product development (labour, samples, testing, analysis) and labelling( 41 ). In our study the products with the lowest mean Na levels in 2011 were supplied by boutique manufacturers (325 mg/100 g) and Coles (287 mg/100 g), a supermarket own label producer. It is unclear why one of the large supermarkets and boutique manufacturers (often small enterprises) were able to reduce the Na content in their products more effectively than other manufacturer types, but it does demonstrate the feasibility of overcoming technical and consumer acceptance issues related to the preparation of lower Na products. The supermarket own label producers and leading manufacturers hold more than half of the Australian pasta sauce market volume share and it is primarily their actions that will determine the success or failure of the FHD commitment. Some leading manufacturers have made a start in Na reduction, with Mars and Simplot showing trends in the right direction. However, the increase in Na in Woolworths’ products between 2008 and 2011 is of concern and highlights the need for sector-wide action. Marked diversity in the approaches to salt reduction taken by manufacturers has previously similarly been demonstrated for breads( Reference Dunford, Webster and Barzi 23 ), fast foods( Reference Grimes, Campbell and Riddell 24 ) and ready meals( Reference Christoforou, Dunford and Neal 25 ).
On this basis, standardization of action should be considered in any future review of the FHD strategy that considers optimal ways of engaging the food industry to reduce Na in processed foods. Working with the food industry to address high Na intake is a priority for many countries and the UK has been a world-leader in the field. The UK has reduced population salt intake by about 10 % over the last decade primarily through salt reductions to processed foods( Reference Shankar, Brambila-Marcias and Traill 42 ). It is important that this momentum continues and that the pressure on the food industry is maintained now that the responsibility for Na reduction has been moved from the FSA to the Responsibility Deal.
A key strength of the present study is that data collection occurred within three months of the announcement of the FHD pasta sauce target and thereby provides a contemporary baseline to track future progress and upon which to make projections. Robust interim assessment should be possible for 2012 and 2014( 19 ) when Australian manufacturers agreed to report progress, and data are also independently monitored( 21 ). Data for 2009 and 2010 were excluded from the analysis and while including these data provides for more data points, including them did not alter the primary finding. Had our study also included other product types, such as processed meat products where the Na reduction target was announced at the same time as pasta sauces, it is possible we could have gained a richer and broader understanding of the implication of the FHD Na recommendations. That said, concentrating only on pasta sauce products provides for a focused analysis of one industry sector, as it is very likely that technical barriers and opportunities for Na reduction differ across sectors. Applying standards from other countries, in this case the UK, objectively describes how the Australian process stacks up against a directly relevant world-class model being considered by several other countries( Reference Campbell, Neal and MacGregor 43 ). Market share data for individual products were unavailable to us and appear unlikely to become available to public health over the next few years as the cost is prohibitive. Weighting of the analyses by sales will not therefore be possible and analyses based on means may result in over- or underestimation of effects. However, prior comparison between Na levels based on crude means and weighted data did not show markedly different findings( Reference Mhurchu, Capelin and Dunford 44 ). In projecting (scenario 2) we elected to reduce all products from leading manufacturers with a 2011 Na content less than the ‘action point’ by 15 %, although the FHD makes no specific recommendation. This reduction was chosen as consistent with the published criteria for products with Na levels above the ‘action point’ and was also in line with results from a recent dietary model that reported a 10 % or greater reduction would benefit consumers who were brand loyal( 45 ). A previous study( 46 ) identified inaccuracies in nutrition labelling, although the number of errors is likely to be low and the impact on the study conclusions small. Coverage of Australian pasta sauce products is unlikely to be complete although sampling from the flagship stores of leading Australian supermarket chains means that the analysis includes the majority of pasta sauce products likely to be consumed.
Conclusion
While some manufacturers have been proactive and reduced Na levels of their products over recent years, there is little evidence of a systematic effort by all manufacturers. The coming together of government, the food industry and public health groups to establish targets for salt as part of the FHD indicates wide-ranging commitment to tackle high salt consumption in Australia. However, our research clearly demonstrates that manufacturers will need to reformulate pasta sauce products well beyond the FHD commitment if changes are to contribute importantly to national Na reduction efforts. Government leadership to motivate and reduce barriers to reformulation, together with the implementation of targets to establish a level playing field and transparent systematic monitoring of salt levels in foods, are crucial ways to strengthen the FHD commitment outcome.
Acknowledgements
Sources of funding: H.T. completed this work as part of the requirements for a Master of Human Nutrition degree at Deakin University, supervised by Dr Mark Kestin. H.T. is supported by a National Health and Medical Research Council Postgraduate Scholarship. E.D. is supported by a Sydney Medical School Foundation scholarship, J.W. is supported by a National Heart and Stroke Foundation postdoctoral fellowship, B.N. is supported by an Australian Research Council Future Fellowship. Conflicts of interest: H.T. is a Research Assistant, E.D. is the Research Officer, J.W. is the Senior Project Manager and B.N. is the Chairman of the Australian Division of World Action on Salt & Health (AWASH). J.W. was previously responsible for implementing the UK FSA salt reduction strategy. Authors’ contributions: H.T. and E.D. designed the study and wrote the first draft of the paper. H.T. and E.D. were responsible for the collation of the data, H.T. did the data analysis. All authors provided input into subsequent drafts. Acknowledgements: The authors thank Anthea Christoforou for her help in reviewing the manuscript.





