The worldwide prevalence of overweight and obesity among adults is increasing( Reference Ogden, Yanovski and Carroll 1 ). However, the overall success of behavioural interventions to treat overweight and obesity is moderate( Reference Perri and Corsica 2 ). Successful behavioural weight-loss interventions generally achieve the greatest weight loss after 6 months of treatment (5 % to 10 %)( Reference Perri and Corsica 2 ). However, weight loss is typically followed by gradual regain of lost weight( Reference Levy, Finch and Crowell 3 ). At 2 years post-treatment weight generally stabilises at 5 % less than the pre-treatment weight( Reference Levy, Finch and Crowell 3 ) and after 5 years more than half of participants will have regained back to their pre-treatment weight, or greater( Reference Wadden, Crerand and Brock 4 ). Therefore, there is a need for treatment strategies that not only promote initial weight loss, but also facilitate long-term maintenance of lost weight.
Web-based weight-loss interventions have emerged in recent years as an alternative or adjunct to traditional treatment mediums. Recent systematic reviews highlight the potential of web-based treatments in achieving significant weight loss( Reference Arem and Irwin 5 – Reference Weinstein 8 ). However, they have also found that most studies fail to follow up participants beyond the intervention period( Reference Neve, Morgan and Jones 6 ), so it is not known whether participants who successfully lose weight with web-based programmes can maintain the lost weight.
Currently, commercial programmes are the most accessible web-based weight-loss programmes for consumers( Reference Krukowski, West and Harvey-Berino 9 ). However only one has been rigorously evaluated in two randomised controlled trials (RCT)( Reference Womble, Wadden and McGuckin 10 , Reference Gold, Burke and Pintauro 11 ), and neither study followed up participants beyond the intervention period. A small number of other commercial weight-loss programmes have evaluated long-term outcomes( Reference Tsai and Wadden 12 ) and demonstrated results similar to other lifestyle interventions( Reference Gosselin and Cote 13 – Reference Wolfe 16 ). However, sampling bias is evident in all studies, demonstrated by inclusion of only those participants who successfully lost weight( Reference Lowe, Kral and Miller-Kovach 14 – Reference Wolfe 16 ) or only evaluating results for women( Reference Gosselin and Cote 13 ). Therefore, studies to date may misrepresent commercial weight-loss programmes’ overall success due to study populations not being representative of all programme participants. There is a need for ongoing research to determine the long-term effectiveness of commercial and web-based weight-loss programmes in groups who are representative of all enrolees.
Previous research has identified behavioural factors that are associated with long-term weight-loss maintenance. These include consistent self-monitoring (e.g. of weight, eating habits and/or physical activity)( Reference Butryn, Phelan and Hill 17 – Reference Wing and Hill 20 ), a physically active lifestyle( Reference Elfhag and Rössner 18 – Reference Catenacci, Grunwald and Ingebrigtsen 21 ), healthy eating habits such as consuming less dietary fat and regular breakfast consumption( Reference Wyatt, Grunwald and Mosca 22 ), limiting the number of meals from fast-food restaurants( Reference Kruger, Blanck and Gillespie 19 ) and appropriate levels of dietary restraint and emotional eating( Reference Elfhag and Rössner 18 ). The National Weight Control Registry (NWCR) is the primary study to explore behavioural characteristics associated with weight-loss maintenance( Reference Hill, Wyatt and Phelan 23 ). However, as the NWCR recruits participants who have lost at least 30 lb (13·6 kg) and maintained that weight loss for at least 1 year( Reference Hill, Wyatt and Phelan 23 ), it identifies the behavioural factors associated with successful weight loss and/or weight-loss maintenance only in a cohort of initially successful individuals, not all individuals who attempt weight loss or seek treatment. The identification of behavioural factors that are associated with successful weight loss, among all individuals who seek treatment, is imperative to the development of evidence-based strategies to incorporate into obesity treatments or to introduce at the end of weight-loss treatments in order to improve their overall impact in the long term.
Therefore, the aims of the current study were to: (i) examine the prevalence of successful weight loss 15 months post-enrolment in a commercially available web-based weight-loss programme; and (ii) determine behavioural factors associated with successful weight loss 15 months post-enrolment.
Experimental methods
Participants and setting
The commercial web-based weight-loss programme (The Biggest Loser Club Australia) was a 12-week programme, but participants could choose to subscribe for a longer duration to assist with further weight loss and/or maintenance. The programme has been described in detail previously( Reference Neve, Collins and Morgan 24 ). Briefly, the web-based platform developed by SP Health Co. incorporated key evidence-based weight-management strategies with features that align with the key elements of social cognitive theory( Reference Bandura 25 ) including self-management, social support, self-efficacy, outcome expectations and expectancies, and perceived barriers/facilitators. Enrolees were aged 18–75 years and had a BMI ≥ 22 kg/m2, based on self-reported height and weight. Enrolees purchased subscription plan(s) of 1, 3, 4 or 12 months’ duration. In 2007/08 a subscription cost $AUD 16·50–79·95 per month, and was dependent on the number of months a participant subscribed. Participants could subscribe to more than one subscription plan over time and it did not have to be consecutive to the previous subscription. Participants were eligible for inclusion in the current study if they paid for their first subscription between 15 August 2007 and 31 May 2008 and agreed at enrolment to being contacted for possible participation in future research.
Of the 11 341 individuals who paid for their first subscription, 5625 agreed to participate in research and were invited to participate in the online survey (Fig. 1). These individuals were significantly older, had a higher BMI at enrolment and had a lower Index of Relative Socioeconomic Advantage and Disadvantage (IRSAD) than those who did not agree to participate in further research (P < 0·001). A higher proportion of eligible participants were of Anglo-Saxon descent and a lower proportion was from major cities of Australia (P < 0·001).
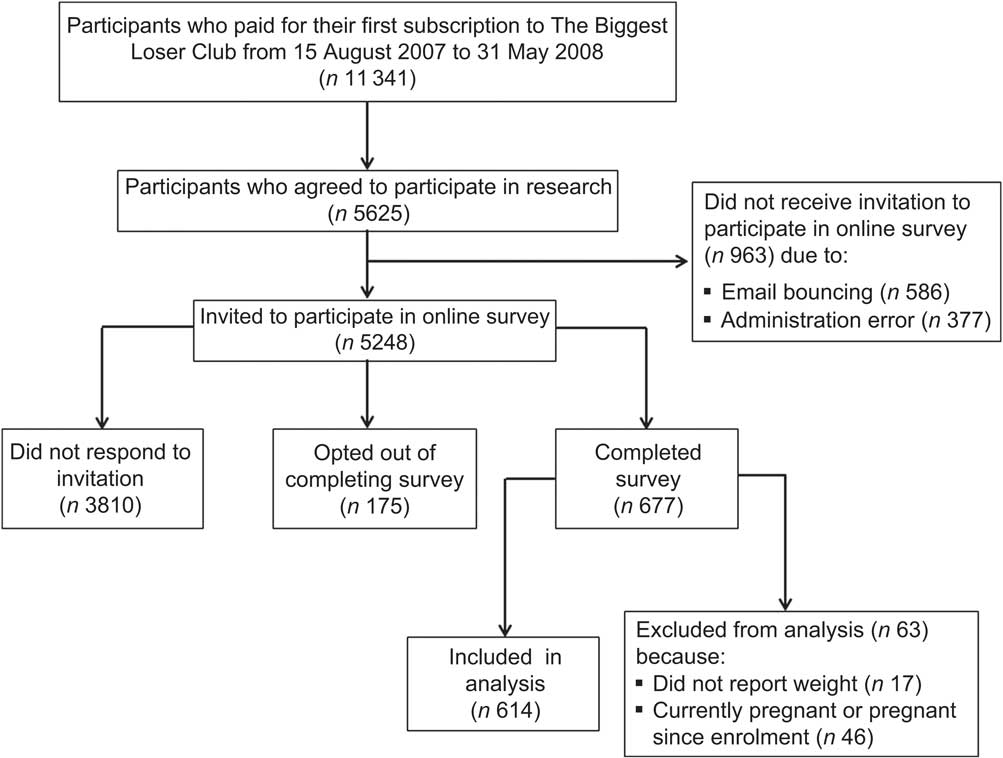
Fig. 1 Participant flow in the study
Recruitment
Eligible participants (n 5625) were invited to participate in an online survey via a personalised email from SP Health Co. sent 15 months after the participants’ initial enrolment. The invitation email provided a link to complete the online survey or to opt out if they did not wish to participate. Participants who did not respond to the initial invitation within 2 weeks were sent weekly email reminders for up to 3 weeks. Participants who completed the survey received a free calorie counter valued at $AUD 7·95.
Twelve per cent (n 677) of eligible participants completed the survey. Sixty-eight per cent did not respond to the survey invitation, 17 % did not receive the email invitation to participate, and 3 % reported they did not wish to complete the survey. Sixty-three participants were excluded from the analysis as they did not report their weight in the online survey (n 17) or because they were or had been pregnant (n 46) since joining the programme (Fig. 1).
Table 1 describes pre-treatment sociodemographic characteristics by survey response/non-response. Those who completed the survey had a higher baseline BMI and a higher proportion was Anglo-Saxon. It was intended that the survey be completed 15 months post-enrolment (i.e. ∼450 d). On average the survey was completed 486 d after enrolment, and ranged from 447 to 538 d. Most survey completers (41 %) subscribed to the programme for 3 months or less.
Table 1 Pre-treatment characteristics of a commercial web-based weight-loss programme cohort by survey completion status, Australia, 2007–2008
| Completed | Did not complete | ||||
| (n 614) | (n 5011) | ||||
| Median or % | IQR or n | Median or % | IQR or n | P value | |
| Age (years)* | 38·3 | 32·0, 36·2 | 35·2 | 29·0, 41·7 | <0·001† |
| Gender | |||||
| Female | 88·0 | 540 | 87·4 | 4381 | 0·71† |
| Male | 12·1 | 74 | 12·6 | 630 | |
| BMI (kg/m2)* | 32·7 | 29·0, 38·1 | 32·4 | 28·5, 37·6 | 0·07† |
| Ethnicity | |||||
| Anglo-Saxon | 73·1 | 449 | 63·1 | 3164 | <0·001‡ |
| European | 11·2 | 69 | 14·9 | 746 | |
| Other | 2·9 | 18 | 3·2 | 161 | |
| Did not wish to respond | 12·7 | 78 | 18·8 | 940 | |
| Socio-economic status (IRSAD) | |||||
| 1–2 | 6·7 | 40 | 6·6 | 327 | 0·687‡ |
| 3–4 | 9·3 | 56 | 10·1 | 496 | |
| 5–6 | 20·5 | 123 | 18·9 | 931 | |
| 7–8 | 30·7 | 184 | 29·2 | 1442 | |
| 9–10 | 32·8 | 197 | 35·2 | 1736 | |
| Remoteness (ARIA) | |||||
| Major city | 73·0 | 438 | 74·3 | 3665 | 0·356‡ |
| Regional/remote | 27·0 | 162 | 25·7 | 1268 | |
IQR, interquartile range; IRSAD, Index of Relative Socioeconomic Advantage and Disadvantage; ARIA, Accessibility/Remoteness Index of Australia.
*Data are presented as median and IQR.
†Wilcoxon rank-sum test.
‡χ 2 test.
Data collection
All data were collected by SP Health Co. and provided to the researchers in de-identified form. Data were collected predominantly from the online survey which included thirty-two questions related to the participant's weight status, eating and activity behaviours, weight control practices and intervention satisfaction. The survey took participants approximately 10 min to complete. The survey was pilot-tested in a convenience sample of adults (n 10) and refined prior to commencement to ensure that there was clear and consistent understanding of the questions by respondents, the survey had a logical flow of questions, the administration and data collection were accurate, and to determine the average time taken to complete the survey. Additional data utilised for the study included responses from a pre-treatment survey completed during enrolment to the programme, which included self-reported anthropometric and demographic data. Data regarding the membership history of each participant within the initial 15 months of membership (e.g. date of enrolment, date membership ceased and the type of subscription plans held) were also collected.
Ethics approval for the study was obtained from the University of Newcastle Human Research Ethics Committee.
Weight-loss success
Weight change (absolute and percentage) achieved at 15 months post-enrolment was calculated by subtracting the participants’ weight reported in the online survey from their pre-treatment weight. Participants were categorised as successful if they achieved a percentage weight loss of ≥5 % from enrolment to 15 months. A weight loss of ≥5 % was selected as it has previously been recommended as the criterion to evaluate weight-management programmes( Reference Thomas 26 ), and has also been shown to be associated with improvements in weight-related morbidity, particularly reduced incidence of type 2 diabetes mellitus( Reference Womble, Wadden and McGuckin 10 , Reference Knowler, Barrett-Connor and Fowler 27 , 28 ).
Behavioural factors
The online survey included short dietary questions, previously developed and validated as part of the Australian National Nutrition Survey( Reference Rutishauser, Webb and Abrahan 29 , Reference Marks, Webb and Rutishauser 30 ), to ascertain frequency and/or quantity of current intake of key foods and food groups (breakfast, takeaway food, restaurant meals, soda, fruit and vegetables). Participants were also asked if they currently partook in specific eating habits (i.e. Do you do any of the following? Please tick all that apply. Fry foods; Use butter in cooking; Drink tea or coffee with sugar; Use low-fat products where possible; Skip meals; Keep snack foods in the house; Drink 6 or more glasses of water per day).
Responses to two questions regarding current frequency and quantity of alcohol consumption categorised usual alcohol intake related risk( 31 ). Alcohol intake was defined as ‘low risk’ if a maximum of one to two drinks were consumed on any drinking occasion, as ‘moderate risk’ if three to four drinks were consumed on any drinking occasion, as ‘high risk’ if more than four drinks were consumed on any drinking occasion, or as ‘no risk’ if the participant did not consume alcohol.
Dietary restraint, emotional and uncontrolled eating were assessed using the Three Factor Eating Questionnaire-R18, and scores were calculated as previously described by Karlsson et al. ( Reference Karlsson, Persson and Sjostrom 32 ).
Physical activity level was estimated using the validated International Physical Activity Questionnaire (IPAQ) short format( Reference Craig, Marshall and Sjöström 33 ). Responses were categorised as low, moderate or high levels of physical activity based on the estimated time spent walking or in moderate or vigorous intensity activity in the previous 7 d( 34 ). The number of minutes participants reported sitting per day was used as a marker of sedentary behaviour. Current frequency of self-monitoring of weight, food and exercise were independently assessed on a 7-point Likert scale ranging from never to several times daily.
Confounders
Sociodemographic characteristics from the pre-treatment survey included anthropometric (weight and height) and demographic (age, gender and postcode) data. Self-reported height and weight were used to calculate BMI (weight (kg)/[height (m)]2). Reported postcodes were assigned an IRSAD category (1–10)( 35 ) as an indicator of socio-economic status, as well as an Accessibility/Remoteness Index of Australia (ARIA)( 36 ) to classify the level of remoteness of the area in which the participant lived.
The total number of different weight-loss strategies used in the previous 15 months, other than the website, were calculated (e.g. other commercial programmes, meal replacements, fad diets, diet books or manuals, other web-based programmes, surgery, medications, consultations with health professionals). Satisfaction with the commercial web-based weight-loss programme was also assessed using a 5-point Likert scale ranging from extremely satisfied to extremely dissatisfied.
Data analysis
Data analysis was undertaken using the STATA statistical software package version 11·0 (StataCorp, College Station, TX, USA), with P values less than 0·01 considered statistically significant due to the large number of comparisons being made. Basic descriptive statistics (median and interquartile range (IQR) for continuous variables, percentages for categorical variables) were used to describe participants’ sociodemographic characteristics at enrolment, weight change from baseline to 15 months, programme-related factors and behavioural factors. Categorical variables were collapsed to a smaller number of responses if a low number of participants responded in the extremes of the response range. Differences in sociodemographic characteristics at enrolment of survey responders/non-responders, as well as differences in behavioural factors and potential confounders between successful and unsuccessful participants, were tested using the two-sample t test for normally distributed or the Wilcoxon rank-sum test for non-normally distributed continuous variables and the χ 2 test for categorical variables. Differences in weight change (absolute and percentage) from baseline to 15 months by length of membership in the programme (≤6 months, >6 to ≤12 months, >12 months) were tested using the Kruskal–Wallis test for equality of populations for continuous variables and the χ 2 test for categorical variables. Univariate logistic regression was conducted to assess the association of behavioural factors with successful weight loss. Behavioural factors with P < 0·2 were tested for inclusion in the multiple logistic regression model using a stepwise approach. Sociodemographic and programme-related factors found to be significantly associated with weight-loss success in the univariate analysis were also included in the multiple logistic regression model due to potential confounding as well as known confounders (baseline BMI, age, ethnicity, gender). If any two behavioural or confounding factors were found to be significantly correlated (P < 0·05, r > 0·7), the factor most significantly associated with successful weight loss from the univariate analysis was included in the model. Self-monitoring of food and self-monitoring of exercise had a significant association (r = 0·80), as did the total number of membership days and the number of days since enrolment (r = 0·79). Therefore, self-monitoring of exercise and the total number of membership days were tested in the multivariate model.
Participants who completed the online survey but did not report their weight (n 17), or who reported that they were currently pregnant or had been pregnant in the previous 15 months (n 46), were excluded from the analysis.
Results
Prevalence of successful weight loss
The median (IQR) 15-month weight change was −2·0 (−8·0, −1·8) kg or −2·7 % of enrolment weight. Just over a third of participants (37 %) achieved a weight loss of ≥5 % and therefore classified as successful (Table 2). The degree of weight loss increased significantly as the length of membership increased. That is, a median (IQR) weight change of −4·4 (−10·7, −0·5) % was achieved by those who were members for >12 months, with 47 % achieving a weight loss of ≥5 %, whereas a median (IQR) weight change of −0·9 (−5·7, −2·9) % was achieved by those who were members for ≤3 months, of whom 28 % achieved a ≥5 % weight loss.
Table 2 Self-reported weight change from enrolment to 15 months in a commercial web-based weight-loss programme cohort, Australia, 2007–2008

| Membership length (months) | ||||||||||
| Total | ≤3 | >3 to ≤6 | >6 to ≤12 | >12 | ||||||
| (n 614) | (n 249) | (n 91) | (n 91) | (n 183) | ||||||
| Weight change from enrolment to 15 months | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR |
| Absolute† (kg) | −2·0 | 8·0, 1·8 | −1·0 | −5·0, 2·2 | −1·2 | −6·0, 1·4 | −4·0 | −10·1, 0·0 | −3·9 | −12·0, 0·5 |
| Percentage of baseline (%)* | −2·7 | −8·2, 1·6 | −0·9 | −5·7, 2·9 | −1·7 | −6·5, 1·7 | −3·9 | −11·1, 0·0 | −4·4 | −10·7, 0·5 |
| % | % | % | % | % | ||||||
| Percentage change from baseline by defined categories† | ||||||||||
| >0 % | 33·9 | 39·8 | 38·5 | 24·2 | 28·4 | |||||
| ≤0 to >−5 % | 29·5 | 32·5 | 27·5 | 31·9 | 25·1 | |||||
| ≤−5 % to >−10 % | 16·1 | 14·9 | 16·5 | 12·1 | 19·7 | |||||
| ≤−10 % to >−15 % | 10·9 | 8·8 | 5·5 | 19·8 | 12·0 | |||||
| ≤−15 % | 9·6 | 4·0 | 12·1 | 12·1 | 14·8 | |||||
IQR, interquartile range.
*Significant difference (P = 0·0 0 1) between membership length categories (Kruskal–Wallis test).
†Significant difference (P < 0·001) between membership length categories (χ 2 test).
Differences between successful and unsuccessful participants
Table 3 describes differences in sociodemographic characteristics and programme-related factors by successful and unsuccessful participants. Successful participants had been a member of the programme for significantly more days, and therefore completed the survey fewer days since their last membership. Successful participants were less likely to have used other weight-loss strategies in the previous 15 months.
Table 3 Sociodemographic and intervention factors by successful and unsuccessful participants in a commercial web-based weight-loss programme cohort, Australia, 2007–2008
| Successful | Unsuccessful | ||||
| (n 225) | (n 389) | ||||
| Median or % | IQR or n | Median or % | IQR or n | P value | |
| Age (years)* | 38·0 | 31·5, 45·7 | 38·5 | 32·0, 46·3 | 0·86† |
| Gender | |||||
| Female | 85·3 | 192 | 89·5 | 348 | 0·13‡ |
| Male | 14·7 | 33 | 10·5 | 41 | |
| BMI (kg/m2)* | 34·1 | 29·4, 39·4 | 32·3 | 28·7, 36·8 | 0·02† |
| Ethnicity | |||||
| Anglo-Saxon | 74·2 | 167 | 72·5 | 282 | 0·054‡ |
| European | 13·8 | 31 | 9·8 | 38 | |
| Other | 3·6 | 8 | 2·6 | 10 | |
| Did not wish to respond | 8·4 | 19 | 15·2 | 59 | |
| Socio-economic status (IRSAD) | |||||
| 1–2 | 6·4 | 14 | 6·8 | 26 | 0·93‡ |
| 3–4 | 10·5 | 23 | 8·7 | 33 | |
| 5–6 | 20·5 | 45 | 20·5 | 78 | |
| 7–8 | 29·1 | 64 | 31·6 | 120 | |
| 9–10 | 33·6 | 74 | 32·4 | 123 | |
| Remoteness (ARIA) | |||||
| Major city | 74·6 | 164 | 72·1 | 274 | 0·51‡ |
| Regional/remote | 25·5 | 56 | 27·9 | 106 | |
| Days since enrolment* | 484 | 470, 494 | 488 | 474, 499 | <0·001† |
| Days a member in previous 15 months* | 214 | 92, 395 | 121 | 91, 366 | <0·001† |
| Days since last membership* | 126 | 0, 379 | 333 | 84, 396 | <0·001† |
| Other weight-loss strategies used in the previous 15 months | |||||
| None | 47·1 | 106 | 34·7 | 135 | <0·001‡ |
| 1 | 35·1 | 79 | 30·6 | 119 | |
| 2 | 12·0 | 27 | 17·5 | 68 | |
| 3 or more | 5·8 | 13 | 17·2 | 67 | |
| Intervention satisfaction | |||||
| Satisfied | 79·6 | 179 | 70·2 | 273 | 0·03‡ |
| Neutral | 17·3 | 39 | 23·9 | 93 | |
| Dissatisfied | 3·1 | 7 | 5·9 | 23 | |
IQR, interquartile range.
*Values are presented as median and IQR.
†Wilcoxon rank-sum test.
‡χ 2 test.
Table 4 describes differences in behavioural factors by successful and unsuccessful participants. A higher proportion of successful participants reported more frequent self-monitoring of weight, dietary intake and exercise. A higher proportion of successful participants met the recommended intake targets for vegetable and fruit consumption (i.e. respectively five and two servings daily).
Table 4 Prevalence and risk of behavioural factors by successful and unsuccessful participants in a commercial web-based weight-loss programme cohort, Australia, 2007–2008

| Successful | Unsuccessful | ||||
| (n 225) | (n 389) | ||||
| % | n | % | n | P value | |
| Self-monitoring: Weight | |||||
| <1 time/month or never | 11·1 | 25 | 26·2 | 102 | <0·001* |
| <1 time/week | 9·8 | 22 | 7·7 | 30 | |
| 1 time/week | 38·7 | 87 | 30·6 | 119 | |
| >1 time/week | 21·8 | 49 | 17·7 | 69 | |
| ≥1 time/d | 18·7 | 42 | 17·7 | 69 | |
| Self-monitoring: Food | |||||
| <1 time/month or never | 47·6 | 107 | 60·2 | 234 | 0·002* |
| <1 time/week | 4·9 | 11 | 6·2 | 24 | |
| 1 time/week | 4·0 | 9 | 5·4 | 21 | |
| >1 time/week | 12·4 | 28 | 10·5 | 41 | |
| ≥1 time/d | 31·1 | 70 | 17·7 | 69 | |
| Self-monitoring: Exercise | |||||
| <1 time/month or never | 43·1 | 97 | 59·4 | 231 | <0·001* |
| <1 time/week | 6·2 | 14 | 5·1 | 20 | |
| 1 time/week | 7·1 | 16 | 5·7 | 22 | |
| >1 time/week | 12·0 | 27 | 12·6 | 49 | |
| ≥1 time/d | 31·6 | 71 | 17·2 | 67 | |
| Vegetable intake | |||||
| <2 servings/d | 35·6 | 80 | 48·3 | 188 | 0·009* |
| 2–4 servings/d | 50·2 | 113 | 40·1 | 156 | |
| ≥5 servings/d | 14·2 | 32 | 11·6 | 45 | |
| Fruit intake | |||||
| <1 serving/d | 22·7 | 51 | 31·9 | 124 | 0·026* |
| 1 serving/d | 33·3 | 75 | 33·2 | 129 | |
| ≥2 servings/d | 44·0 | 99 | 35·0 | 136 | |
| Do you fry foods? | |||||
| Yes | 19·6 | 44 | 26·5 | 103 | 0·053* |
| No | 80·4 | 181 | 73·5 | 286 | |
| Do you use butter in cooking? | |||||
| Yes | 19·6 | 44 | 27·3 | 106 | 0·033* |
| No | 80·4 | 181 | 72·8 | 283 | |
| Do you skip meals? | |||||
| Yes | 21·8 | 49 | 42·4 | 165 | <0·001* |
| No | 78·2 | 176 | 57·6 | 224 | |
| Do you drink tea or coffee with sugar? | |||||
| Yes | 28·4 | 64 | 32·9 | 128 | 0·251* |
| No | 71·6 | 161 | 67·1 | 261 | |
| Do you use low-fat products? | |||||
| Yes | 87·1 | 196 | 79·4 | 309 | 0·016* |
| No | 12·9 | 29 | 20·6 | 80 | |
| Do you keep snack foods in the house? | |||||
| Yes | 27·1 | 61 | 44·0 | 171 | <0·001* |
| No | 72·9 | 164 | 56·0 | 218 | |
| Drink 6+ glasses of water a day? | |||||
| Yes | 62·7 | 141 | 44·0 | 171 | 0·108* |
| No | 37·3 | 84 | 56·0 | 218 | |
| Breakfast consumption frequency | |||||
| <5 d/week | 9·8 | 22 | 22·0 | 85 | <0·001* |
| ≥5 d/week | 90·2 | 202 | 78·0 | 302 | |
| Soft drinks consumption frequency | |||||
| >1/d | 6·3 | 14 | 9·0 | 35 | 0·004* |
| 1/d | 5·8 | 13 | 8·8 | 34 | |
| <1/d | 21·0 | 47 | 30·4 | 118 | |
| Never | 67·0 | 150 | 51·8 | 201 | |
| Takeaway food consumption frequency | |||||
| >1 time/week | 7·6 | 17 | 25·3 | 98 | <0·001* |
| 1 time/week | 20·1 | 45 | 20·6 | 80 | |
| 1–3 times/month | 38·4 | 86 | 29·9 | 116 | |
| 1 time/month | 24·1 | 54 | 18·3 | 71 | |
| Never | 9·8 | 22 | 5·9 | 23 | |
| Restaurant food consumption frequency | |||||
| >1 time/week | 7·6 | 17 | 10·8 | 42 | 0·705* |
| 1 time/week | 14·7 | 33 | 13·1 | 51 | |
| 1–3 times/month | 32·1 | 72 | 33·3 | 129 | |
| 1 time/month | 35·7 | 80 | 33·0 | 128 | |
| Never | 9·8 | 22 | 9·8 | 38 | |
| Alcohol intake | |||||
| High risk | 11·2 | 25 | 12·4 | 48 | 0·924* |
| Moderate risk | 20·5 | 46 | 18·8 | 73 | |
| Low risk | 51·3 | 115 | 52·6 | 204 | |
| No risk | 17·0 | 38 | 16·2 | 63 | |
| Physical activity level | |||||
| Low | 28·5 | 61 | 41·7 | 148 | 0·002* |
| Moderate | 41·1 | 88 | 38·3 | 136 | |
| High | 30·4 | 65 | 20·0 | 71 | |
| Time spent sitting (min/d) | |||||
| Median | 300 | 360 | 0·04† | ||
| IQR | 161, 480 | 180, 500 | |||
| Restraint score | |||||
| Mean | 15·2 | 14·4 | <0·001‡ | ||
| sd | 2·0 | 2·0 | |||
| Emotional eating score | 7·2 | 8·4 | <0·001‡ | ||
| Mean | 2·5 | 2·5 | |||
| sd | |||||
| Uncontrolled eating score | <0·001† | ||||
| Median | 20 | 22 | |||
| IQR | 18, 22 | 19, 24 | |||
*χ 2 test.
†Wilcoxon rank-sum test.
‡Two-sample t test.
Successful participants were less likely to report unhealthy eating habits such as skipping meals, keeping snack foods in the house, eating takeaway foods, drinking soft drinks and not regularly consuming breakfast. Successful participants also had significantly lower uncontrolled and emotional eating scores, as well as higher dietary restraint scores. A higher proportion of successful participants reported high levels of physical activity.
Multivariate analysis of successful weight loss
Table 5 outlines the behavioural factors found to be independently associated with successful weight loss. Compared with participants who reported weighing themselves infrequently (never to less than once monthly), those who weighed themselves more frequently were more likely to be successful. Participants who weighed themselves less than once weekly but more than once monthly had the highest odds of being successful. Participants who reported they ate takeaway foods less than once weekly, particularly those who never consumed takeaway foods, were more likely to be successful. Participants who did not skip meals or keep snack foods in the house, as well as those with higher dietary restraint scores were also significantly more likely to be successful. The higher a participant's emotional eating score the less likely he/she was to be successful.
Table 5 Behavioural factors independently associated with successful weight loss in a commercial web-based weight-loss programme cohort, Australia, 2007–2008
| OR | 95 % CI | P value | |
| Self-monitoring of weight | |||
| <1 time/week | 4·31 | 1·88, 9·85 | 0·001 |
| 1 time/week | 2·66 | 1·45, 4·87 | 0·002 |
| >1 time/week | 2·95 | 1·50, 5·80 | 0·002 |
| ≥1 time/d | 3·01 | 1·50, 6·05 | 0·002 |
| Do you skip meals? | |||
| No | 2·18 | 1·39, 3·41 | 0·001 |
| Do you keep snack foods in the house? | |||
| No | 1·97 | 1·28, 3·02 | 0·002 |
| Takeaway food consumption frequency | |||
| 1–3 times/month | 3·63 | 1·84, 7·17 | <0·001 |
| 1 time/month | 3·31 | 1·54, 7·11 | 0·002 |
| Never | 4·56 | 1·72, 12·08 | 0·002 |
| Eating patterns score | |||
| Dietary restraint | 1·18 | 1·06, 1·31 | 0·002 |
| Emotional eating | 0·84 | 0·77, 0·91 | <0·001 |
Adjusted for gender, baseline BMI, age, ethnicity, days since membership, total membership days, intervention satisfaction and number of other weight-loss strategies (n 601).
Discussion
The first aim of the current study was to examine the prevalence of successful weight loss at 15 months post-enrolment in a commercial web-based weight-loss programme. The study is one of only a small number( Reference Gosselin and Cote 13 – Reference Wolfe 16 ) to investigate the long-term weight loss achieved by participants of a commercial weight-loss programme, and the first to evaluate this for a commercial web-based programme. We found that just over a third of participants achieved a weight loss of ≥5 % at 15 months post-enrolment. The study also identified key behavioural factors that were associated with the likelihood of successful weight loss 15 months post-enrolment. These included regular self-monitoring of weight, not skipping meals, not keeping snack foods in the house, infrequent takeaway food consumption, less emotional eating and greater dietary restraint. These findings highlight strategies that can be incorporated in treatment programmes in an attempt to improve long-term weight loss.
Over one third of participants achieved a clinically important weight loss at 15 months post-enrolment, thereby reducing their risk of weight-related morbidity such as type 2 diabetes mellitus( Reference Knowler, Barrett-Connor and Fowler 27 , 28 ). Furthermore, the proportion of participants who achieved ≥5 % weight loss increased significantly as membership length increased. As many participants (41 %) subscribed to the programme for less than 3 months, a potential strategy to improve long-term weight loss is to encourage participants to subscribe for longer or to offer a longer (e.g. 6 months) minimum subscription length. This is consistent with other research which suggests that the greatest level of weight loss is achieved after 6 months of treatment( Reference Perri and Corsica 2 ). It is noteworthy that over 60 % of the participants who subscribed for 3 months or less had not regressed to their enrolment weight after 1 year, as is commonly the case for behavioural weight-loss programmes( Reference Perri and Corsica 2 ). This suggests that a short-term web-based weight-loss programme has the potential to achieve modest weight loss 1 year post-enrolment and prevent weight gain. However, this must be further tested prospectively and objectively in an RCT.
Notably only two RCT( Reference Morgan, Lubans and Collins 37 , Reference Rothert, Strecher and Doyle 38 ) and one observational study( Reference Wing, Pinto and Crane 39 ) have assessed participants’ maintenance of weight loss following the completion of a web-based weight-loss intervention. Morgan et al. reported a −5·3 kg weight change at 9 months post-completion of a 3-month web-based intervention, with 58 % of participants achieving a weight loss of ≥5 %( Reference Morgan, Lubans and Collins 37 ). Rothert et al. reported significantly greater weight-loss maintenance in a tailored Internet group (−2·7 and −3·0 %) compared with an information-only Internet group (−1·2 and −1·2 %) at 3 and 6 months post-enrolment in a 6-week intervention( Reference Rothert, Strecher and Doyle 38 ). Wing et al. reported an average weight loss of −3·8 % in overweight and obese participants 2 months post-completion of a 16-week web-based intervention( Reference Wing, Pinto and Crane 39 ). The magnitude of long-term weight loss reported in the current study may appear low in comparison to the other studies. However, those studies evaluated weight change only within a short time frame after completion of the intervention (2 to 9 months), and the interventions also included non-web-based components (e.g. face-to-face sessions, resources)( Reference Morgan, Lubans and Collins 37 – Reference Wing, Pinto and Crane 39 ). As many survey participants (41 %) in the present study subscribed to the programme for 3 months or less, many had not participated in the programme for approximately 1 year when they completed the survey; therefore the results are noteworthy.
The results from long-term follow-up studies of commercial weight-loss programmes have been varied. Approximately 44 % of female participants of Mincavi, a group-based face-to-face programme, maintained ≥5 % weight loss after 2 years( Reference Gosselin and Cote 13 ). Weight Watchers, a group based face-to-face programme, reported that 70–80 % of participants who achieved their goal weight maintained ≥5 % weight loss after 1 year( Reference Lowe, Kral and Miller-Kovach 14 , Reference Lowe, Miller-Kovach and Phelan 15 ). The Jenny Craig programme, which involves weekly face-to-face individual and group consultations, has reported that among participants who achieved their goal weight, an average weight loss of 12·5 kg was sustained after 1 year( Reference Wolfe 16 ). The prevalence of successful weight loss reported in the current study may appear low in comparison to other long-term follow-up studies of commercial weight-loss programmes. However, the participants in the comparison studies are not representative of all enrolees, with three of the studies only including participants who were initially successful at achieving significant weight loss( Reference Gosselin and Cote 13 – Reference Wolfe 16 ) and the other study only including female participants( Reference Gosselin and Cote 13 ). Therefore, the results cannot be generalised to the whole population of their respective commercial users in terms of degree of long-term weight loss. More specifically, those studies that only include participants who were initially successful may overestimate the true prevalence of long-term weight loss.
The second aim of our study was to determine behavioural factors associated with successful weight loss 15 months post-enrolment. We found in a univariate analysis that twelve different behavioural factors were associated with successful weight loss 15 months post-enrolment. However, only six behavioural factors were independently associated with success. This suggests that there were six key drivers (self-monitoring of weight, skipping meals, keeping snack food in the house, frequency takeaway food consumption, restrained eating and emotional eating) to long-term weight-loss success in this cohort. It is likely that the other six factors that were not independently associated with success were related to these six key drivers (e.g. skipping meals and breakfast consumption frequency).
Self-monitoring of weight was associated with successful weight loss, which is consistent with previous research that has demonstrated more frequent self-weighing (daily or weekly) is associated with improved weight-loss maintenance( Reference Kruger, Blanck and Gillespie 19 , Reference McGuire, Wing and Klem 40 – Reference Wing, Tate and Gorin 42 ). However, these studies often do not differentiate between less frequent self-weighing categories, and group frequencies such as less than once per month and less than once per week together. Our study included a greater number of self-weighing frequency categories and demonstrated that participants who weighed themselves less than once per week, but more often than once per month, had the greatest odds of being successful. This suggests that more frequent self-weighing (e.g. one or more times per week or day) may not be essential to achieve clinically important weight loss in the long term.
Eating patterns play an important role in long-term weight-loss success, with higher levels of dietary restraint and lower levels of emotional eating associated with maintenance of lost weight( Reference McGuire, Wing and Klem 40 , Reference Butryn, Thomas and Lowe 43 – Reference Niemeier, Phelan and Fava 46 ). The results from our study are consistent, demonstrating that for each 1 point increase in the emotional eating score, the likelihood of being successful decreased by 16 %, whereas for each 1 point increase in restraint score the likelihood of being successful increased by 18 %. Therefore, strategies to assist individuals to manage emotional eating and to strengthen dietary restraint are required. Recent studies have demonstrated that behavioural interventions can produce positive changes to participants’ eating patterns( Reference Teixeira, Silva and Coutinho 44 ) but further research is required to determine the most effective strategies to ensure long-term weight loss.
Previous studies have demonstrated that successful weight loss is associated with consistent eating patterns and regular breakfast consumption( Reference Wyatt, Grunwald and Mosca 22 , Reference Gorin, Phelan and Wing 47 ). While unable to demonstrate that consuming breakfast was significantly associated with success, we found that skipping meals was associated with a lack of success. Therefore, it may not be skipping breakfast that is the problem behaviour, but rather skipping any meals. The current study also suggests that the availability of snack foods within the home environment may also negatively affect weight loss. Finally, our study suggests that reducing takeaway food consumption to less than once per week significantly increases the likelihood of successful weight loss, with no takeaway food consumption being most ideal, which is also consistent with previous research( Reference Kruger, Blanck and Gillespie 19 ).
Limitations
To maximise external validity our study aimed to recruit participants who were representative of the consumers who enrol in a commercial web-based weight-loss programme. Therefore, inclusion in our study was not dependent on achieving a goal weight or having a significant weight loss or whether individuals completed or used the web-based programme, as is the case with other similar studies. Survey responders were similar to non-responders for most pre-treatment characteristics. However, programme enrolees who agreed to be contacted to participate in research were older, with higher BMI, of lower socio-economic status, and more likely to be Anglo-Saxon or from regional/remote areas of Australia. The response rate to the online survey was also low. However, a similar study that followed up participants 12 months post-enrolment in a web-based weight-loss programme via an online survey achieved a similar response rate (15 %)( Reference Couper, Peytchev and Strecher 48 ). Therefore, the results of our study may misrepresent the prevalence of successful weight loss 15 months post-enrolment among all programme enrolees. The response rate and representativeness of future research could potentially be improved with different recruitment strategies, offering alternative methods of survey completion (e.g. telephone, mail) or greater incentives.
Another potential limitation of the present study is that all outcomes were self-reported. To reduce measurement bias, validated questionnaires (e.g. IPAQ, Three Factor Eating Questionnaire-R18, short diet questions) were used where possible. Self-reported weight data were used to evaluate success, and weight can be under-reported( Reference Conner Gorber, Tremblay and Moher 49 ). However, self-reported weight recorded by participants of a web-based weight-loss programme has been found to be accurate compared with measured weight( Reference Harvey-Berino, West and Buzzell 50 ).
The study also considered behavioural factors cross-sectionally and did not capture pre-treatment or changes in behaviours. Therefore, the analysis demonstrated which behaviours at 15 months were associated with successful weight loss but did not determine whether the participants improved their behaviour to achieve weight loss, or behavioural characteristics remained the same and success could have been predicted at baseline. Furthermore, the analysis adjusted for intervention-related factors (e.g. number of membership days, other weight-loss strategies used), but the study did not examine whether these intervention-related factors influenced the behavioural factors associated with successful weight loss, and this could be an area of future research.
Conclusions
The findings suggest that over one third of participants in a commercial web-based weight-loss programme achieved clinically important weight loss 15 months post-enrolment, and that participating in the programme for 6 months or longer was associated with greater weight loss. The findings also provide support for existing recommendations, as well as propose novel strategies, to be incorporated within obesity treatments to improve the likelihood of successful weight-loss outcomes in the long term. More specifically the findings suggest individuals trying to achieve or maintain ≥5 % weight loss should be advised to regularly weigh themselves, avoid skipping meals or keeping snack foods in the house, and limit the frequency of takeaway food consumption. Furthermore, strategies to assist individuals to manage emotional eating and to strengthen dietary restraint should also be incorporated within obesity treatments.
Acknowledgements
Sources of funding: This study was supported by an Australian Postgraduate Award (M.J.N.), a scholarship top-up from SP Health Co. Pty Ltd (M.J.N.) and an Australian National Health and Medical Research Council Career Development Award research fellowship (C.E.C.). Potential conflicts of interest: M.J.N. received a postgraduate scholarship top-up from SP Health Co. C.E.C. was a consultant dietitian to SP Health Co. P.J.M. and C.E.C. hold an Australian Research Council (ARC) Linkage project grant that is evaluating a weight-loss programme with SP Health Co. Author contributions: All authors were responsible for the study design, and reviewing, editing and approving the final version of the manuscript. M.J.N. conducted the statistical analysis and drafted the manuscript. Acknowledgements: The authors acknowledge the work of Ben Noblet in retrieving the data, Anna Crook and Penelope Jones for assistance with interpreting the data set, and Emma Julian for management of the online survey.








