Preventing repetition of self-harm has been the focus of a number of studies. Psychological and social interventions have mostly been evaluated but none has been clearly effective in reducing repetition (Reference Hawton, Arensman and TownsendHawton et al, 1998). Many trials have been too small to identify clinically important effects. The three largest trials to date have involved manual-assisted cognitive therapy for those with a previous history of self-harm (Reference Tyrer, Thompson and SchmidtTyrer et al, 2003), a primary care guideline-based intervention (Reference Bennewith, Stocks and GunnellBennewith et al, 2002) and the provision of a crisis card allowing telephone consultation as an alternative to self-harm (Reference Evans, Morgan and HaywardEvans et al, 1999). Neither manual-assisted cognitive therapy nor the primary care guideline intervention had any effect on reducing repetition of self-harm at 1 year. The study of crisis card provision has only reported the 6-month outcome. At this time there was no overall effect of the crisis card in preventing repetition of self-harm but there was an indication of benefit for those with no previous history of self-harm (odds ratio (OR) compared with usual treatment 0.64, 95% confidence interval (CI) 0.34-1.22).
We report the results of the 12-month follow-up of the crisis card study. This allows direct comparison with other studies reporting 12-month repetition rates and further investigation of the potential benefit of this intervention for those who have no previous history of self-harm.
METHOD
The study recruited 827 patients admitted to hospital following self-harm between November 1994 and July 1996. Patients were randomised after standard treatment was planned to also receive a card offering 24-h crisis telephone consultation with an on-call psychiatrist for up to 6 months after the index episode. Those in the standard treatment group received no information on the crisis card. Standard treatment varied according to the judgement of the assessing clinician and included advice only, referral to the community mental health team or psychiatric hospital admission. The trial is described in detail elsewhere (Reference Evans, Morgan and HaywardEvans et al, 1999). The primary outcome was repeated self-harm within 6 months of the index episode. We investigated 12-month repetition rates to determine whether the suggested beneficial effects of emergency card provision for those with first episodes of self-harm are sustained over longer periods.
We identified repetition of self-harm by means of a self-harm case register (Reference Evans, Johnson and StantonEvans et al, 1996). We used logistic regression in Stata version 8.0 for Windows to calculate odds ratios for repetition comparing control and intervention groups. We investigated whether the effect of the intervention differed between people with and without a previous history of self-harm by fitting an interaction term (treatment × past history) to our model and investigating the overall treatment effect. We compared time to episode of repeat self-harm between those receiving standard care and those with a crisis card using the log-rank test.
RESULTS
We recruited 827 patients, representing 64% of those admitted to general hospital following self-harm during the study period; 417 were given a crisis card and 410 received standard treatment (Reference Evans, Morgan and HaywardEvans et al, 1999).
Main analysis
There were 167 individuals (20.2%) with repeat episodes of self-harm in the 12 months after the index episode. Of participants carrying a crisis card, 90 (21.6%) had a repeat episode of self-harm within 1 year compared with 77 (18.8%) in the control group (OR=1.19, 95% CI 0.85-1.67). Time to repetition did not differ between the control and intervention groups (log-rank test χ2 0.98, P=0.32). The Kaplan-Meier curve is shown in Fig. 1.
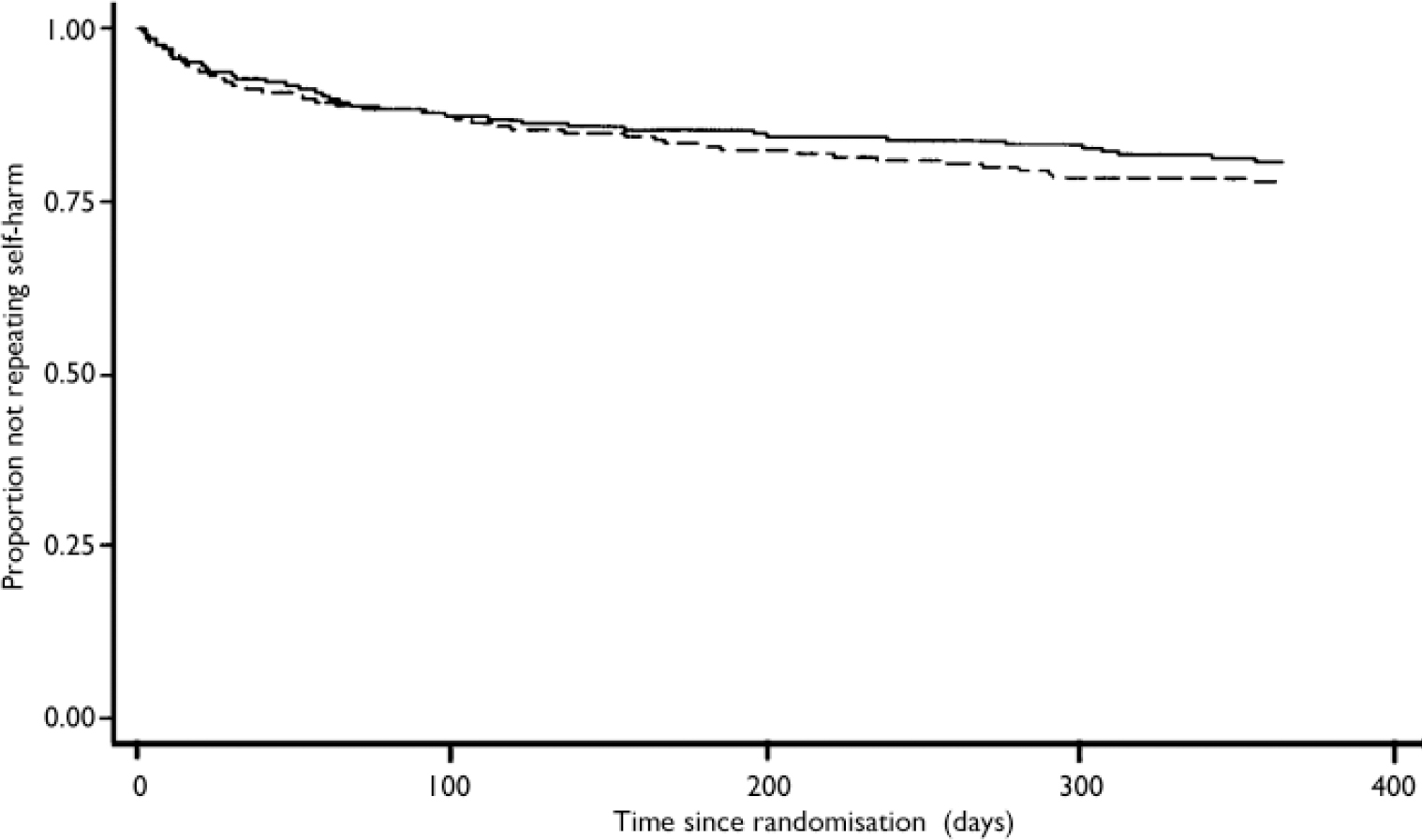
Fig. 1 Kaplan-Meier survival estimate: days to repetition of self-harm; —, treatment as usual; - - - -, crisis card.
Subgroup analysis
There was no strong evidence that the effect of the crisis card differed between those with the single index episode and those with a past history of self-harm (likelihood ratio χ2=2.37, P=0.12). Of the subjects in the intervention group with the single index episode, 30 (13.6%) had a repeat episode of self-harm within 1 year compared with 31 (15%) in the control group (OR=0.89, 95% CI 0.52-1.52). Of the individuals in the intervention group with a previous history of self-harm, 60 (30.9%) had repeat episodes of self-harm within 1 year compared with 45 (22.5%) in the control group (OR=1.54, 95% CI 0.98-2.42).
During the first 6 months following the provision of the card, 70 individuals made telephone contact; the majority only once; the maximum number of contacts was 16. We have no data on subjects trying to make contact but failing to get past the hospital switchboard. There was no report of such difficulties. Of patients in the intervention group, those making telephone contact were more likely to have repeat episodes of self-harm (OR=4.91, 95% CI 2.83-8.50).
DISCUSSION
These data confirm that there is no benefit in issuing a crisis card allowing telephone consultation to all those presenting to hospital after self-harm. There was no effect on the number of repeat episodes at 12 months and no difference between those with and without a previous history of self-harm. The possible benefit for those with a single past episode of self-harm (Reference Evans, Morgan and HaywardEvans et al, 1999) was not found at 12-month follow-up. It is important to note that while not significant, the 95% confidence interval for repetition among those with a previous history of self-harm includes a 142% increase. We can be confident that the crisis card is unlikely to be beneficial for this group.
A number of issues need consideration. We defined repetition by hospital attendance following self-harm. It is known that self-reported repetition rates are higher than those identified solely through hospital attendance (Reference Guthrie, Kapur and Mackway-JonesGuthrie et al, 2001). It is unlikely that this differed between intervention and control groups. Although this study was large, it was not large enough to exclude a clinically important effect in those presenting following a first episode. The 95% confidence intervals around the estimated effect of the intervention following a first episode included a 48% reduction and a 52% increase in repetition. As this intervention is likely to be much cheaper than manual-assisted cognitive therapy, a small beneficial effect may still be cost-effective.
This study was based on services running nearly 10 years ago. There have been major changes in mental health service provision in the UK in recent years (Department of Health, 1999). It is noteworthy that those who made contact were at greater risk of repetition, possibly because they had suicidal ideas. An alternative explanation is that the telephone contact evoked feelings of rejection thereby increasing risk. More skilled handling of those in crisis may be necessary. Crisis teams are now widely available and staffed 24 h a day. These teams include staff with specific training or experience in crisis management. It is possible that contact with crisis teams might prevent repeated self-harm more effectively than contact with on-call junior doctors as offered in this study. The context in which the card is provided is important. We did not have any information about how many subjects kept the card or whether they thought it might be useful. The card is more likely to be effective if the recipient is confident they can use it. Often specialist teams assess those presenting with an episode of self-harm; this includes crisis teams in some areas. Such teams might encourage greater confidence in the card as an alternative to self-harm.
Before conducting further trials of sufficient size, qualitative research should be undertaken to investigate whether this intervention might benefit those presenting following a first episode. This could help to refine the intervention to utilise some of the potentially beneficial changes in mental health service provision in the UK since the planning of this original trial.
Acknowledgements
We thank Gemma McCann for updating the self-harm register and Muriel Cole for preparing the manuscript.




eLetters
No eLetters have been published for this article.