Interest in the early psychosis paradigm began with a focus on early detection and optimal treatment of first-episode psychosis. More recently, attention has extended to the clinically active prepsychotic or prodromal phase of illness (Reference Edwards and McGorryEdwards & McGorry, 2002; Reference Malla and NormanMalla & Norman, 2002). Although this shift in focus has been associated with scientific, clinical and ethical challenges, a number of clinical and research gains have already been realised. These achievements can be attributed to the establishment of a number of clinical and academic centres with a strong commitment to evidence-based medicine and the close integration of clinical and research questions.
This paper describes principles, progress and dilemmas in the prospective detection, engagement and treatment of young people with incipient psychosis. The research programmes conducting this research are also described.
METHOD
Concepts for prepsychotic research
Focus on the prepsychotic or prodromal phase of illness has resulted in the development of specific terminology and concepts. Knowledge of these concepts is essential in understanding the intricacies of this field of research.
The period prior to clear-cut diagnosis of psychosis has traditionally been referred to as the ‘premorbid’ phase. However, this term is confusing because it suggests that changes in mental state and functioning only occur with the onset of acute illness. Studies of childhood antecedents of schizophrenia, although demonstrating significant but minor differences between controls and those who later developed schizophrenia, highlighted the quiescence of the illness during the early phase of life (Reference Jones, Rodgers and MurrayJones et al, 1994). Research by Häfner and colleagues, however, revealed that psychotic illnesses really begin to have clinical and social consequences after puberty, typically during adolescence and early adult life (Reference Hafner, Maurer, Löffler, Hafner and GattazHäfner et al, 1995). A period of non-specific symptoms and growing functional impairment often occurs prior to the full emergence of the more diagnostically specific positive psychotic symptoms. This phase is referred to as the ‘prodrome’.
‘Prodrome’ derives from a Greek word meaning the forerunner of an event (Reference Fava, Grandi and CanestrariFava et al, 1990). This concept is commonly used in clinical medicine to refer to symptoms and signs of an illness experienced before the full-blown syndrome becomes evident. This implies that symptoms are experienced during the prodrome and that the development of full-blown illness is inevitable.
Within the mental health field, indicated prevention is, according to Mrazek & Haggarty, ‘… targeted to high-risk individuals who are identified as having minimal but detectable signs or symptoms foreshadowing mental disorder, or biological markers indicating predisposition for mental disorder, but who do not meet… diagnostic levels at the current time’ (1994, p. 154). Intervention during the prodromal phase of a first psychotic episode with the intention of stopping the onset of the full-blown illness is an example of indicated prevention.
Benefits and obstacles of prepsychotic intervention
The fact that a very substantial amount of the disability that develops in schizophrenia accumulates prior to the appearance of the full positive psychotic syndrome and may create a ceiling for eventual recovery in young people is a key reason for attempting some form of prepsychotic intervention. Other potential benefits are outlined in Appendix 1. A number of obstacles to intervention during this phase should also be noted (Appendix 2).
Challenges in identifying the prepsychotic phase
Indicated prevention in the prepsychotic phase relies on the accurate identification of individuals who are truly experiencing this phase of illness. This requires the ability to distinguish between the prodrome and the premorbid phase as well as between the prodrome and frank psychosis.
Defining the beginning of the onset of a potential psychotic disorder is difficult because a specific group of symptoms occurring during this time has not been identified. In fact, retrospective descriptions of the prodromal phase have indicated that the earliest symptoms experienced by an individual who later developed an acute episode are non-specific, such as sleep disturbance, depressed mood, anxiety and irritability (Reference Yung and McGorryYung & McGorry, 1996; Reference Moller and HusbyMøller & Husby, 2000).
Subtle ‘attenuated’ forms of psychotic symptoms have also been reported during this early stage. Sub-threshold psychotic symptoms deviate from normal phenomena but are not frankly psychotic. They differ from frank psychotic symptoms in either their degree of intensity or frequency. For example, individuals may be concerned that others are laughing at or are hostile towards them, but realise that this is not really true and that he or she is just being ‘a bit paranoid’. Perceptual disturbances can also occur below ‘psychotic intensity’.
Identifying the onset of the prepsychotic phase requires differentiation of ‘normal’ experiences from ‘abnormal’. This is made more difficult by evidence that attenuated psychotic symptoms and ‘psychotic-like experiences’ are experienced by the general population, at far higher rates than psychotic disorders (Reference Peters, Joseph and GarretyPeters et al, 1999; Reference Peters and ClarkePeters, 2001; van Os et al, Reference van Os, Hanssen and Bijl2000, Reference van Os, Hanssen and Bijl2001). This indicates that at least some attenuated psychotic symptoms must either resolve without developing into full-blown psychosis or they can persist without developing into a full-blown psychotic disorder.
Difficulties also exist in identifying the transition point between prepsychotic and acute phases of illness. There is some uncertainty about which types of symptoms should be used to define ‘psychosis’ and when a symptom has become sufficiently deviant to be labelled psychotic. The subjective nature of psychotic symptoms also needs to be considered as observers often date onset of psychotic symptoms well after the individual recalls them as having begun (Reference Häfner, Maurer and LöfflerHäfner et al, 1993; Reference Yung and McGorryYung & McGorry, 1996; Reference Norman and MallaNorman & Malla, 2001). Psychotic symptoms rarely arise suddenly, but are more likely to gradually evolve and worsen, from an attenuated state to a full-threshold state. Most clinicians have no difficulty in diagnosing a full-blown psychotic syndrome in a patient, but more subtle early psychotic features are more difficult to recognise. Appendix 3 summarises other reasons why recognising the onset of psychosis is frequently challenging.
These issues are yet to be resolved. Indeed, discussions about the definition of psychotic disorder tend to become embroiled in debate about the definition of health, disease and illness in general, a subject which is beyond the scope of this article.
Strategies for identifying the prepsychotic phase
A number of strategies have been developed to identify individuals who are thought to be experiencing a prepsychotic phase of illness and are at heightened risk of developing a psychotic disorder. Although differences exist between the strategies they all aim to minimise the identification of false-positives and to maximise true-positives (Reference Yung and McGorryYung & McGorry, 1996). Brief descriptions of these approaches follow.
‘Close-in’ strategy and the ‘at-risk mental state’
Bell (1982) suggested that a ‘close-in’ or ‘multiple gate screening’ approach should be used to identify a high-risk cohort (Reference BellBell, 1992). Using this strategy, an individual must meet a number of conditions to be included in the high-risk group. Bell also recommended using behavioural difficulties in adolescence as selection criteria to improve the accuracy of identifying the high-risk group further. Thus, unlike traditional screening paradigms, this approach is more clinically oriented, focusing on troubled young people, who are experiencing ‘precursor’ signs and symptoms (Reference EatonEaton, 1995). In line with this, these state-based criteria are thought to identify an at-risk mental state.
Studies using this approach have been referred to as ‘ultra-high-risk’ or clinical high-risk studies to differentiate them from traditional high-risk studies, such as the New York high-risk programme (Reference Erlenmeyer-Kimling, Squires-Wheeler and AdamoErlenmeyer-Kimling et al, 1995) or the Copenhagen high-risk project (Reference Cannon and MednickCannon & Mednick, 1993), that rely on family history as the primary inclusion criteria. At-risk mental state/ultra-high risk does not imply that a full-threshold psychotic illness, such as schizophrenia, is inevitable, but suggests that an individual is at risk of developing a psychotic disorder by virtue of their mental state. This terminology is more conservative than the use of the term prodrome, which can only be accurately applied in retrospect if and when the disorder in question fully emerges.
The recommendations made by Bell (Reference Bell1992) were first put into practice at the Personal Assessment and Crisis Evaluation (PACE) Clinic in Melbourne, Australia. The first risk factor used to identify the ultra-high-risk group is age: the strategy focuses on individuals in the peak age range of risk of onset of psychotic disorder–adolescents and young adults (Reference Hafner, Maurer and LöfflerHäfner et al, 1994). According to the criteria developed by the PACE Clinic, other potential risk factors must also be met, such as attenuated psychotic symptoms, self-resolving psychotic symptoms, a trait risk factor (a schizotypal personality disorder in the young person or a family history of a psychotic disorder in a first-degree relative) and functional decline (Appendix 4). Criteria for identifying the ultra-high-risk group have been operationalised according to the Comprehensive Assessment of At Risk Mental States (CAARMS) (Appendix 5) and subsequently using the Structured Interview for Prodromal States (SIPS) and related instruments (Miller et al, Reference Miller, McGlashan and Woods1999, Reference Miller, McGlashan and Rosen2002) and have been validated. The CAARMS and SIPS are semi-structured interviews that were designed to prospectively assess symptoms and signs suggestive of a psychotic prodrome. It should be noted that all young people meeting these criteria are also seeking support and help and are distressed by their symptoms to some degree.
The validity of the ultra-high-risk criteria has now been well supported in longitudinal studies. Out of 49 young people, 20 (41%) who met ultra-high-risk criteria developed an acute psychotic episode within 12 months of recruitment and were started on appropriate neuroleptic treatment (Yung et al, Reference Yung, Phillips and McGorry1998, Reference Yung, Phillips and Yuen2003). This occurred despite the provision of supportive counselling, case management and antidepressant medication if required. The majority of those who developed a psychotic disorder had a DSM–IV diagnosis of schizophrenia (13 out of 20 in the psychosis group, 65%) (Reference Yung, Phillips and YuenYung et al, 2003). The sensitivity and specificity of the criteria could not been determined as individuals who did not meet intake criteria were not followed-up to determine whether they too developed psychosis.
The criteria have been adopted with minor modifications in other centres in different parts of the world. Comparable rates of transition to acute psychosis have been described at these other centres (Table 1). It should be remembered that the population from which subjects are drawn affects the predictive validity of the intake (ultra-high-risk) criteria. As the prevalence of a disorder decreases, the positive predictive value decreases also (Reference Mojabai, Malaspina and SusserMojabai et al, 2003). If the ultra-high-risk criteria were applied to a general population or school setting, the transition rate to full-blown psychosis would be much less than 41%, because the prevalence of truly prodromal individuals in that setting is lower than in the population of help-seeking young people who meet these criteria. There might also be variation in the underlying proportions of true- and false-positives who are referred for assistance. This is dependent on the base rate of psychosis in the different referral source samples, which may change over time within one centre and certainly across centres. For example, the rate of ultra-high-risk positive cases in a general psychiatric out-patient group is 15% (Reference Salokangas, Klosterkotter and BirchwoodSalokangas et al, 2004).
Table 1 Comparison of different rates of transition within 12 months to acute psychosis in different centres
| Centre | Group n | Patients with acute psychosis n (%) |
|---|---|---|
| PACE | 49 | 20 (41) |
| CER | 110 | 77 (70) |
| H-RAP | 34 | 9 (26.5) |
| PRIME | 13 | 7 (54) |
| PAS | 74 | 37 (50) |
| TOPP | 14 | 6 (43) |
| CARE | 53 | 5 (9.4) |
| EDIE | 23 | 5 (22) |
| FETZ | 51 | 5 (9.8) over 15 months |
| PIER | 47 | 11 (23.4) |
Basic symptoms
The German approach to early detection and intervention in schizophrenia follows the long-standing observation that cognitive, affective and social disturbances often occur years before the first psychotic episode and are often recognised by the person affected at this early stage. In the 1960s, these self-experienced deficits were described as ‘basic symptoms’ in great detail by Gerd Huber and colleagues and, based on long-term follow-up studies, have significantly influenced concepts of schizophrenia in German-speaking countries. The Bonn Scale for the Assessment of Basic symptoms (BSABS) was developed to assess the occurrence of these experiences.
In the Bonn long-term study (Reference Huber, Gross and SchüttlerHuber et al, 1979), basic symptoms were found prepsychotically in 37% of patients who later developed schizophrenia. These findings were confirmed by the retrospective Age-Beginning-Course (ABC) study (Reference Häfner, Maurer, Löffler and HafnerḦafner et al, 2002), which revealed even higher rates of patients with long-lasting prepsychotic deficits. Of this group, 73% reported the onset of negative and non-specific symptoms, including basic symptoms, an average of 5 years before the first positive symptom of schizophrenia. Furthermore, social deficits appeared as early as 2–4 years before the first hospital admission and, thus, in the prodromal phase about a year before the onset of the first psychotic symptom (Reference Hafner, Löffler and MaurerHäfner et al, 1999).
In the prospective Cologne Early Recognition study (CER; Reference Klosterkötter, Hellmich and SteinmeyerKlosterkötter et al, 2001), 160 individuals who were suspected of being in the onset phase of schizophrenia were assessed with the BSABS (Reference Gross, Huber, Klosterkötter and LinzGross et al, 1987): 79 patients developed schizophrenia over the follow-up period, which averaged 9.6 years, on average, 1.9 (s.d.=2.5) years after the first examination, and 77 of these 79 participants and 33 who did not develop schizophrenia had reported at least one basic symptom at first examination, indicating reasonably good prognostic accuracy of symptoms (Table 2).
Table 2 Predictive statistics associated with individual basic symptoms
| Basic symptom | Sensitivity | Specificity | PPV | NPV | Odds ratio | FP (%) | FN (%) |
|---|---|---|---|---|---|---|---|
| ≥ Any 1 basic symptom | 0.98 | 0.59 | 0.70 | 0.96 | 70.51 | 20.6 | 1.3 |
| Thought interference | 0.42 | 0.91 | 0.83 | 0.62 | 7.32 | 4.4 | 28.8 |
| Thought perseveration | 0.32 | 0.88 | 0.71 | 0.57 | 3.45 | 6.3 | 33.8 |
| Thought pressure | 0.38 | 0.96 | 0.91 | 0.62 | 14.71 | 1.9 | 30.6 |
| Thought blockages | 0.34 | 0.86 | 0.71 | 0.57 | 3.16 | 6.9 | 32.5 |
| Disturbance of receptive language | 0.39 | 0.91 | 0.82 | 0.61 | 6.46 | 4.4 | 30.0 |
| Decreased ability to discriminate between ideas and perception, fantasy and true memories | 0.27 | 0.95 | 0.84 | 0.57 | 7.03 | 2.5 | 36.3 |
| Unstable ideas of reference | 0.39 | 0.89 | 0.78 | 0.60 | 5.17 | 5.6 | 30.0 |
| Derealisation | 0.28 | 0.90 | 0.73 | 0.56 | 3.50 | 5.0 | 35.6 |
| Visual perception disturbances (at least 1) | 0.46 | 0.85 | 0.75 | 0.62 | 4.83 | 7.5 | 26.9 |
| Acoustic perception disturbances (at least 1) | 0.29 | 0.89 | 0.72 | 0.53 | 3.30 | 5.6 | 35.0 |
Although the German basic symptom approach is more theoretically guided than the ultra-high-risk approach, the transition rate to schizophrenia among the 110 individuals included in the CER study who reported at least one basic symptom at baseline interview was 70%. This is obviously higher than any transition rates to psychosis reported from studies utilising the ultra-high-risk approach (Table 1). It should be noted that the mean follow-up period of the CER study of 9.6 years was much longer than the 12 months reported for the ultra-high-risk samples hitherto. A new instrument to assess basic symptoms was recently developed–the Schizophrenia Prediction Instrument, Adult version (SPI–A). Preliminary results have indicated that 25 of 147 individuals (17%) who have reported experiencing at least one basic symptom have developed schizophrenia within an average of 12 months of assessment (s.d.=7.6; range 2–33). Although preliminary, this result reveals that the basic symptom approach to early detection is not inevitably associated with the strategic and practical disadvantage of necessarily long follow-up periods.
As 20% of individuals who report experiencing basic symptoms do not also report experiencing sub-threshold psychotic symptoms, it is suggested that basic symptoms either describe an additional at-risk group to that identified using ultra-high-risk criteria or – more likely – that basic symptoms occur earlier in course of the illness.
There is a growing consensus in the field that the ‘ultra-high-risk’ and the ‘basic symptom’ approach are complementary, providing criteria to detect different prodromal stages, a concept already realised in the German Research Network on Schizophrenia (GRNS) (Fig. 1).
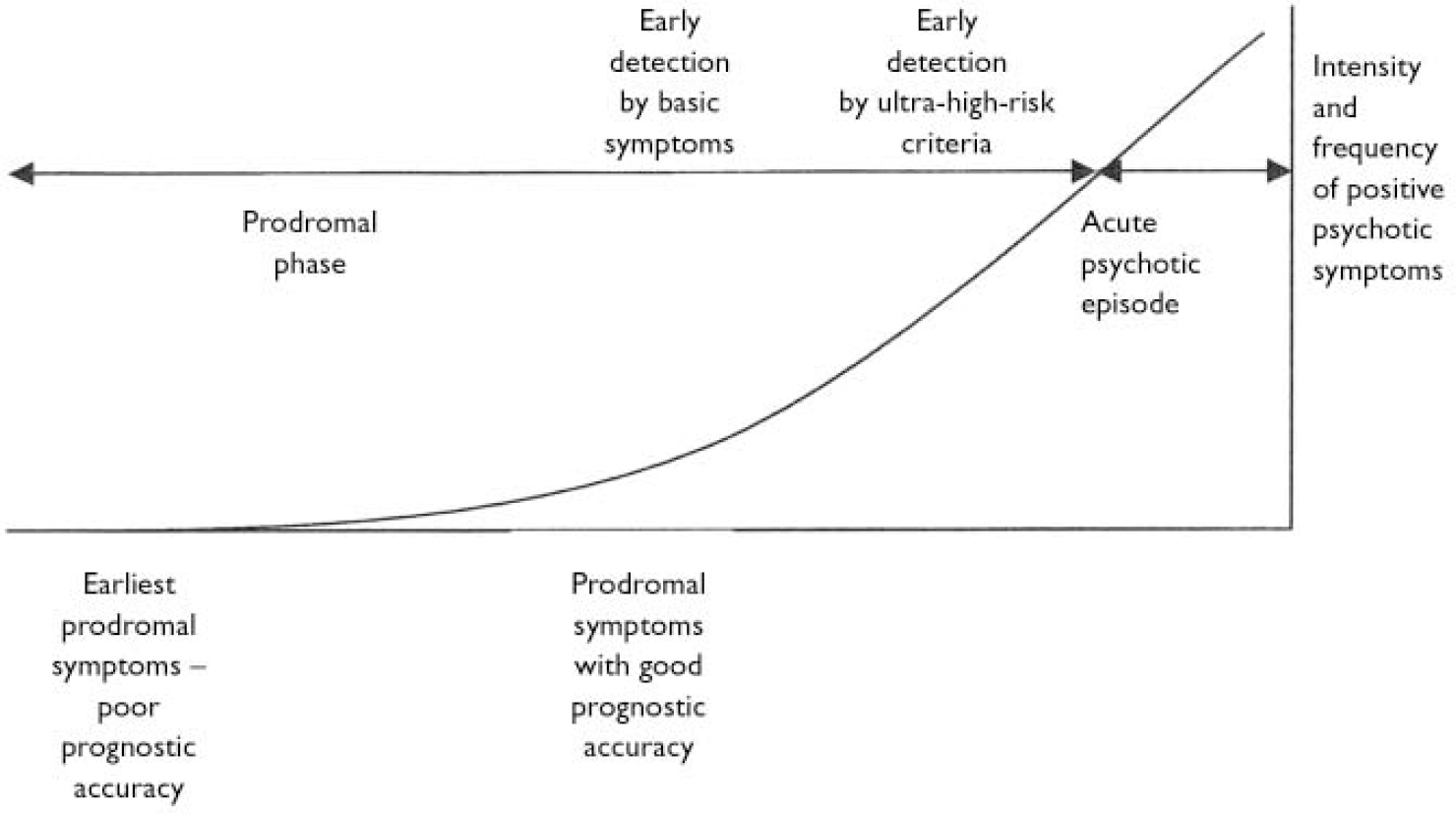
Fig. 1 Model of the onset of psychosis.
Clinical high risk
The Hillside Recognition and Prevention (H-RAP) Program in New York further elaborated the Melbourne ultra-high-risk criteria for identifying young people thought to be at high risk of psychosis. The H-RAP researchers refer to their criteria as identifying a clinical high-risk group to distinguish it from the genetic high-risk studies. Adolescents are recruited to this programme if they experience attenuated positive psychotic symptoms (referred to as the clinical high risk–positive group) or if they display specific combinations of cognitive, academic and social impairments and disorganisation/odd behaviour (referred to as CASID features). This second cohort is referred to as the clinical high risk–negative group and the programme specifically focuses on cognitive impairments which may precede the onset of acute psychosis (Reference CornblattCornblatt, 2002). Operationalised criteria for identifying the clinical high risk–negative group are not yet available. The researchers in this group hypothesise that the developmental course of schizophrenia follows a progression from clinical high risk–negative to – positive to ‘schizophrenia-like psychosis’ (essentially schizophreniform/brief psychotic disorder) to schizophrenia. The transition rate from clinical high risk–positive status to psychotic disorder, using both the PACE and Prevention through Risk Identification, Management and Education (PRIME) clinics’ definitions of psychosis, was 26.5% (9 of 34 patients) within 6 months (Reference Lencz, Smith and AutherLencz et al, 2003), a rate similar to the 6-month transition rate in the PACE Clinic (Reference Yung, Phillips and YuenYung et al, 2003) (Table 1). The transition rate to schizophrenia in the schizophrenia-like psychosis group was 33% (Reference Cornblatt, Lencz and CorrellCornblatt et al, 2002). The key difference between the clinical high-risk and the ultra-high-risk approach is that first-episode schizophrenia rather than first-episode psychosis is the indicated prevention target here, hence the extra category of schizophrenia-like psychosis. This is a key distinction that allows the investigators to regard frankly psychotic patients as ‘sub-threshold’ for schizophrenia and hence contributes to different terminology, strategies and interpretations of results.
RESULTS
Prepsychosis research programmes
Prepsychosis research programmes have now been established in many centres around the world. There are several key, interdependent aims of these programmes:
-
(a) To improve the understanding of the neurobiological and psychosocial processes that occur during the prepsychotic phase and contribute to the onset of acute and persistent psychosis. Conversely, processes that protect against progression and promote recovery and resolution of symptoms and impairment may be clarified.
-
(b) To develop and evaluate a range of psychosocial and biological interventions to treat current syndromes and prevent future disorders fully expressing themselves. Effectiveness and safety issues, including stigma, need to be evaluated hand-in-hand.
-
(c) To establish a clinical service that is not only highly accessible but also acceptable to young people at ultra-high risk of psychosis.
Brief descriptions of these programmes are described below.
The PACE Clinic
This clinic was established in Melbourne, Australia in 1994. It is one arm of a comprehensive early psychosis research programme affiliated with the Early Psychosis Prevention and Intervention Centre (Reference McGorryMcGorry, 1993; Reference McGorry, Edwards and MihalopolousMcGorry et al, 1996). PACE began on a small scale with only a part-time consultant psychiatrist and one research psychologist and a necessarily limited research agenda of mapping the onset of psychosis and establishing valid criteria for identifying the ultra-high-risk cohort. There is now a team of 12 clinicians and research staff at PACE and a more sophisticated clinical research structure. This growth has also mirrored an increased focus on youth mental health in Melbourne over the past few years and the establishment of a youth mental health service (ORYGEN), which contrasts with the usual child and adolescent v. adult mental health divide, reflects the epidemiology of onset of disorders and recognises the special needs of the youth population.
The development and growth of the PACE Clinic has been previously documented (Yung et al, Reference Yung, McGorry and McFarlane1995, Reference Yung, McGorry and McFarlane1996, Reference Yung, Phillips, Drew, McGorry and Jackson1999, Reference Yung, Phillips and McGorry2004; Phillips et al, Reference Phillips, Yung and Hearn1999, Reference Phillips, Leicester and O'Dwyer2002b ; Reference McGorry, Yung, Phillips, Zipursky and SchulzMcGorry et al, 2001a ). Many of the strategies adopted in the establishment of PACE, such as distinguishing the ultra-high-risk service from mainstream mental health services, have ensured that community education is a key feature of the work of the clinic and the provision of clinical assistance to young people referred to the service–independently of their involvement in research projects–has been adopted by other centres.
Prevention through Risk Identification, Management and Education Clinic
The ultra-high-risk concept and close-in strategy have been adopted at the Prevention through Risk Identification, Management and Education (PRIME) Clinic at Yale University, headed by Professor Thomas McGlashan. Young people aged between 12 and 45 years who are thought to be experiencing the onset phase of a first psychotic episode are recruited to the clinic. The PRIME group has coined the term Criteria of Prodromal Syndromes, or COPS, to describe their intake criteria, which are very similar to the ultra-high-risk criteria developed earlier at PACE. The PRIME group have also developed a semi-structured interview originally influenced by the CAARMS and the Positive and Negative Symptom Scale (PANSS; Reference Kay, Fiszbein and OplerKay et al, 1987) called the Structured Interview for Prodromal syndromes (SIPS). The SIPS is utilised to rate presenting symptomatology and to determine if COPS criteria are met (Reference Miller, McGlashan and RosenMiller et al, 2002). Ratings are made on the Scale of Prodromal Symptoms (SOPS), also developed by the PRIME group. Although the PRIME investigators based their definition of the psychosis threshold on that developed at PACE, they did make some changes. For example, PRIME patients are considered to meet the criteria for psychosis if they have attenuated psychotic symptoms and are markedly suicidal or dangerous. The transition rate to acute psychosis in a cohort of young people attending PRIME was 54% (Reference Miller, McGlashan and RosenMiller et al, 2002). The PRIME clinic has expanded to involve other North American centres (Toronto, Calgary and North Carolina) as part of a multicentre clinical trial network.
H-RAP Program
As indicated earlier the H-RAP Program is based in New York. This programme drew from experience with the New York High Risk Project–one of the longest running ‘traditional’ high-risk projects (Reference Erlenmeyer-Kimling, Adamo and RockErlenmeyer-Kimling et al, 1997). Although the RAP programme has not yet conducted a randomised clinical trial with the clinical high-risk population, a ‘naturalistic’ study of the range of clinical treatment provided to this group of young people has been conducted.
Psychological Assistance Service
In 1997 the Psychological Assistance Service (PAS) opened in Newcastle, Australia as a clinical service for the assessment and treatment of young people at high risk of psychosis and those experiencing a first psychotic episode. The high-risk criteria are based on those of PACE but also allow inclusion if a young person has a second-degree relative with a history of psychotic disorder in conjunction with a significant decline in functioning (Reference Carr, Halpin and LauCarr et al, 2000). The transition rate to psychosis within a 12-month period was 50% (Reference Mason, Startup and HalpinMason et al, 2004).
TOPP Clinic
The TOPP Clinic in Norway is an off-shoot of the TIPS programme–a comprehensive community development programme addressing first-episode psychosis (Reference Johannessen, McGlashan and LarsenJohannessen et al, 2001). Larsen (Reference Larsen2002) has used the questionnaire and criteria developed by the PRIME group to identify and follow-up an ultra-high-risk cohort and 84 patients have been assessed with 14 recruited to the study over a 2-year period. Within 12 months of recruitment, 6 out of the 14 (43%) had developed acute psychosis (Reference LarsenLarsen, 2002).
Early Identification and Intervention Evaluation trial
The Early Identification and Intervention Evaluation (EDIE) trial, based in Manchester, UK, reported a 22% transition rate to acute psychosis in 23 young people recruited based on the PACE Clinic criteria who have been followed-up for 6–12 months (Reference Morrison, Bentall and FrenchMorrison et al, 2002). This service is slightly different from the others described in that it is largely a mobile service that utilises other facilities to see patients, such as general practitioner surgeries, schools and so forth and promotes psychological treatment (cognitive–behavioural therapy, CBT) for young people over and above medical approaches (Reference French and MorrisonFrench & Morrison, 2004). Results indicate that cognitively oriented psychological treatment is more effective than monitoring alone in reducing transition rates to acute psychosis in patients at ultra-high risk (Reference Morrison, French and WalfordMorrison et al, 2004).
Early Recognition and Intervention Centre
This centre was established in 2000. As described earlier, criteria have been developed to identify individuals with prepsychosis based on the experience of basic symptoms. Young people are referred to the Early Recognition and Intervention Centre (FETZ) from a broad network of more than 500 primary and mental healthcare professionals, psychiatric hospitals, counselling services, carer associations, schools and health insurance companies. In addition to intensive and continuous public education and awareness campaigns about schizophrenia and psychosis, FETZ provides a thorough psychopathological and neurobiological diagnostic and a wide psychological and biological range of interventions that can be tailored to individual needs. Research conducted by the centre continues the German tradition of early detection, early intervention and investigation of the biological, genetic and neuropsychological basis of schizophrenia. A trial of psychological treatment is currently underway for the early prodromal phase at FETZ, and the late prodromal phase is the focus of a psychopharmacological study utilising amisulpride (Reference Bechdolf, Wagner and HambrechtBechdolf et al, 2002).
OASIS
The OASIS service has recently commenced in south London, UK to detect, assess and intervene in young people at ultra-high risk of psychosis. The PACE Clinic criteria are used and links with the established early psychosis unit (Lambeth Early Onset; LEO) are utilised to identify those individuals who do not meet full criteria for a psychotic disorder but who do meet ultra-high-risk criteria. OASIS is soon to begin a randomised controlled trial using quetiapine and CBT (Reference Johns, Broome and MatthiassonJohns et al, 2002).
Portland Identification and Early Referral service
The Portland Identification and Early Referral (PIER) service is a population-wide system of early detection that utilises a broad-ranging community education and development programme to identify individuals with the early stages of a psychotic disorder based on the COPS/ultra-high-risk criteria (Reference McFarlane, Cook and RobbinsMcFarlane et al, 2002). Detection and engagement rates from this important study are very encouraging. Clinical intervention is multimodal and includes the use of antipsychotic medication ‘where indicated’. The design of this study is in fact similar to the original Buckingham, UK study of Falloon et al (Reference Falloon, Krekorian and Shanahan1990), the findings of which were heuristically very useful, although inconclusive.
Cognitive Assessment and Risk Evaluation programme
The Cognitive Assessment and Risk Evaluation (CARE) programme at the University of California, San Diego is conducting a longitudinal research project to identify psychophysiological, neurocognitive and information-processing measures that are vulnerability markers for schizophrenia-spectrum disorders. Participants in this programme are experiencing low-grade psychotic features, have a schizotypal personality disorder or have a family history of schizophrenia in conjunction with a recent deterioration in functioning. The participants are assessed monthly for a period of 2–5 years (Reference CadenheadCadenhead, 2002).
Center for the Assessment and Prevention of Prodromal States
This centre was established at the University of California, Los Angeles in 2000. This programme aims to investigate the predictive validity for schizophrenia and other psychotic disorders of a range of behavioural, diagnostic, neurocognitive, psychophysiological and neuroimaging measures. Interventions aimed at preventing the onset of psychosis in individuals at high risk are also developed and evaluated.
Commonalities among centres
-
(a) All services attempt to identify young people at high risk of developing first-episode psychosis in the near future, i.e. in the late prodromal phase
-
(b) A combination of mental state risk factors and genetic or trait risk factors is used by all services. Thus all contain heterogeneous samples. The rationale is to maximise pathways available for young people at clinical high risk to access an appropriate service.
-
(c) The services are provided to help-seeking young people. Those who do not wish to be treated cannot be compelled to attend the service
-
(d) In addition, services do not actively promote into care those who are asymptomatic, not distressed or not help-seeking. Thus, for example, screening in schools for students with high levels of attenuated symptoms and encouraging them to attend a service does not occur
-
(e) They all provide a clinical as well as research or evaluative component, although not always for all patients.
-
(f) The services have two clinical foci: management of current difficulties and monitoring and possible prevention or attenuation of emerging psychosis
-
(g) Those services that do use antipsychotic medication in clinical trials use very low doses. This is congruent with the concept of staging in cancer treatment, in which prompt detection enables less toxic therapies to be used early in the course of treatment, compared with more invasive treatments used in more advanced illness.
-
(h) The services are linked with early psychosis services or are able to provide management of first-episode psychosis themselves. Thus, should psychosis occur, timely and optimal treatment is available and duration of untreated psychosis minimised.
-
(i) Rate of transition to psychosis within 12 months ranges from 22% to 54% across the services, but is of the same order of magnitude.
The International Prodromal Research Network (IPRN), which includes many clinicians and researchers working within the services described above, has been created. Meetings are held on a regular basis to discuss progress, implications of research findings and future directions. It is hoped that the creation of such a network will lead to a collaborative research approach.
Prediction of transition to acute psychosis
Clinical predictors
The development and validation of criteria that identify young people at very high risk of developing a psychotic disorder within a short follow-up period has opened the way for further research evaluating putative risk factors for psychosis. Research is currently underway at various centres investigating the role of mood and anxiety, drug and alcohol usage, obstetric complications, delayed childhood milestone achievement, neurological abnormalities, poor premorbid adjustment and other factors in the prediction of psychosis.
Clinical variables including long duration of non-specific symptoms, poor psychosocial functioning, comorbid depression and disorganisation have been associated with increased risk of transition to psychosis within the ultra-high-risk group (Reference Yung, Phillips and YuenYung et al, 2003). Obstetric complications have not been associated with a higher risk of transition to psychosis in the ultra-high-risk cohort. Results of other investigations are anticipated.
Neurobiological predictors
Many studies have suggested that the hippocampal volumes of individuals with established schizophrenia or first-episode psychosis are smaller than controls (Reference Velakoulis, Wood, McGorry and PantelisVelakoulis et al, 2000). Magnetic resonance imaging (MRI) scans of the brains of patients at ultra-high risk are obtained to determine if volume changes in the hippocampal region precede the development of acute psychosis or emerge as mental state deteriorates. Consistent with the neurodevelopmental hypothesis, hippocampal volumes of PACE patients at ultra-high risk at intake lie midway between those of normal controls and patients with chronic schizophrenia or first-episode psychosis (Reference Phillips, Velakoulis and PantelisPhillips et al, 2002a ). More puzzling are the results of a survival analysis, which revealed that those patients at ultra-high risk with larger (although in the normal range) left hippocampal volumes at intake were more likely to develop a psychotic episode in the subsequent 12-month period (Reference Phillips, Velakoulis and PantelisPhillips et al, 2002a ). A comparison of MRI scans of PACE patients at ultra-high risk taken prior to the onset of psychosis, and again once frank psychotic disorder had developed, revealed reduction of grey matter volumes in the left insula cortex and the left posterior medial temporal structures, including the hippocampus and posterior hippocampal gyrus, during the transition to psychosis (Reference Pantelis, Velakouis and McGorryPantelis et al, 2003). This suggests that brain changes occur during the process of transition to psychosis, and although the basis of this remains uncertain it opens up the exciting possibility that with sufficiently early and effective treatment such changes, and their consequences, could be minimised or aborted. Other imaging techniques, such as magnetic resonance spectroscopy (MRS) and functional MRI are currently being investigated.
Assessment of olfactory (smell) identification provides an indication of circuitry involving the orbitofrontal cortex. Deficits in olfactory identification are consistently found in patients with chronic schizophrenia (Reference Brewer, Edwards and AndersonBrewer et al, 1996) and first-episode psychosis (Reference Moberg, Doty and TuretskyMoberg et al, 1997; Reference Seidman, Goldstein and GoodmanSeidman et al, 1997; Reference Brewer, Pantelis and AndersonBrewer et al, 2001). The olfactory identification ability of 81 PACE individuals at ultra-high risk was compared with 31 healthy controls. Those individuals at ultra-high risk who later developed a schizophrenia-spectrum disorder (12 members of the cohort) displayed a significant impairment in olfactory identification ability compared with the individuals at ultra-high risk who did not develop psychosis, the individuals at ultra-high risk who developed a non-schizophrenia-spectrum disorder and the healthy comparison group (Reference Brewer, Wood and McGorryBrewer et al, 2003).
Neuropsychological impairment has been consistently associated with psychotic disorders. It is reasonable to speculate that cognitive functioning might be impaired in individuals who are in the early phases of developing a psychosis and that these changes might also be predictive of future psychosis or whether they come ‘on-line’ once acute psychosis has developed (Reference CadenheadCadenhead, 2002). With this in mind, neuropsychological assessment of individuals at high risk is undertaken as a focus of research at some of the centres described earlier.
Individuals with schizophrenia often display impairments in attention (Reference Heinrichs and ZakzanisHeinrichs & Zakzanis, 1998). Particular interest has been paid to performance of individuals with prepsychosis on the Continuous Performance Task (CPT; Reference Cornblatt, Risch and FarisCornblatt et al, 1988), which assesses attention. The performance of PACE individuals at ultra-high risk on the CPT lies between healthy controls and patients with first-episode psychosis but was closer to the performance of the first-episode group. However, no differences have been found between individuals at ultra-high risk who later developed acute psychosis and those who did not on CPT performance (Reference FranceyFrancey, 2002).
The performance of individuals at ultra-high risk on a range of other neurocognitive tests has been compared with individuals with established or first-episode psychosis as well as healthy age-matched controls at the PACE Clinic. Individuals at ultra-high risk have shown marked impairments in performance on tests of spatial working memory and delayed matching to sample compared with a healthy comparison group (Reference Wood, Pantelis and ProffittWood et al, 2003a ). Further investigation is required to assess the validity of working memory as a predictive tool for psychosis (Reference Wood, Berger and VelakoulisWood et al, 2003b ).
PACE patients at ultra-high risk have also been found to show significantly worse performance on the Performance and Full (short-form) IQ scales of the WAIS–R (Reference WardWard, 1990) compared with controls. Specifically, individuals at ultra-high risk who developed psychosis performed significantly more poorly than those who did not on tests of logical memory and the Visual Reproduction test (Reference Brewer, Francey and WoodBrewer et al, 2005). This finding is suggestive of prefrontal impairments and is in line with findings of impaired spatial working memory (Reference Wood, Berger and VelakoulisWood et al, 2003b ), poorer olfactory identification (Reference Brewer, Wood and McGorryBrewer et al, 2003) and lower frontal grey matter volumes (Reference Pantelis, Velakouis and McGorryPantelis et al, 2003).
The performance of young people attending the PRIME Clinic on a range of neurocognitive tests assessing intellectual functioning, memory, executive functioning and attention was also intermediate to normal controls and those with schizophrenia (Reference Hawkins, Addington and KeefeHawkins et al, 2004). Those participants who developed psychosis tended to perform worse on tasks assessing ‘control’ and tasks of visual memory (Reference Hawkins, Addington and KeefeHawkins et al, 2004). Those who developed psychosis early (within 28 days of assessment) performed worse at entry on tasks of working memory and visual memory than those who became psychotic later (Reference Hawkins, Addington and KeefeHawkins et al, 2004).
The group at ultra-high risk with ‘basic symptoms’ seen at FETZ performed worse than healthy controls on tests of verbal fluency, attention and memory function (Reference Hambrecht, Lammertink and KlosterkötterHambrecht et al, 2002). The relationship between neurocognitive performance and transition to acute psychosis in the FETZ group has not yet been reported.
Intervening in the prepsychotic phase
The aim of treatment provided during the prepsychotic phase is to reduce distressing symptoms experienced by young people who meet high-risk criteria, and, if possible, to prevent these symptoms from worsening and developing into acute psychosis. A stress–vulnerability model of the development of psychosis underpins the treatment approach, incorporating medical and psychological strategies.
Psychological treatment
The psychological treatment provided at the PACE Clinic is primarily based on CBT principles and draws not only on mainstream CBT techniques, but also on the treatment approaches that have been developed and evaluated for use in established psychotic disorders. The therapist and client work together to develop a personal formulation or model for understanding the symptoms the young person is experiencing and strategies for coping with, and reducing these symptoms. Assistance is often provided in liaising with housing, education, employment or other services as difficulties in these areas may contribute to the young person's increased risk status through increasing stress levels.
Clinicians at EDIE in Manchester, UK have described cognitive therapy aimed at assisting young people meeting ultra-high-risk criteria to cope with their symptoms and possibly to prevent the onset of acute psychosis (Reference French and MorrisonFrench & Morrison, 2004). This psychological therapy is targeted towards symptoms that are causing distress and disability with little or no side-effects and is based around a formulation of the affected individual's life experiences, environment, self and social knowledge, intrusions and their interpretations of intrusions, and their emotional, behavioural, cognitive and physiological responses. ‘Change strategies’, such as normalisation, and generating and evaluation of alternative explanations are then employed to assist the individual to deal with the symptoms and to alter their interpretation of events.
Biological treatment
More controversy surrounds the proposal of providing pharmacological treatment for individuals in the prepsychotic phase of illness. The optimal approach remains to be clarified by research. The risk/benefit ratio of offering pharmacological therapy prior to psychosis onset is a big consideration.
One treatment that has been proposed is antipsychotic medication. The rationale behind this proposal is straightforward: antipsychotic medication has demonstrated efficacy with individuals with established psychotic illnesses and this efficacy might translate to the prepsychotic phase. It has been argued that transition rates to psychosis in the ultra-high-risk and basic symptoms groups are not sufficiently high to warrant provision of neuroleptic treatment with known side-effects, as the false-positive rate is too great (Reference Bentall and MorrisonBentall & Morrison, 2002). However, the ‘number-needed-to-treat’ for early clinical trials is not supportive of this argument (Reference Yung and McGorryYung & McGorry, 2003). One strategy for reconciling this impasse is to provide antipsychotic medication within a well-monitored clinical trial environment. Results of two such trials have been released (see below).
Neuroprotective agents might also benefit young people in the prepsychotic phase. The rationale behind such an approach is that dysregulation of neuronal cell production and degeneration in some brain areas might explain neurodevelopmental abnormalities seen in early psychosis (Reference Berger, Wood and McGorryBerger et al, 2003). Neuroprotective substances promoting the regulation of these processes, such as lithium (Reference Manji, Moore and ChenManji et al, 1999), eicosapentanoic acid (EPA; Reference Fenton, Hibbeln and KnableFenton et al, 2000) and glycine (Reference Javitt, Silipo and CienfuegosJavitt et al, 2001), might be potent therapeutic avenues to explore. Open-labelled studies using lithium, glycine and EPA are now underway in Melbourne and Yale (Woods, personal communication, Colorado Springs, 2003).
Other treatment options have yet to be tested in the population at ultra-high risk. One candidate treatment is corticotrophin-releasing hormone receptor agonists (Reference Corcoran, Walker and HuotCorcoran et al, 2003). Furthermore, a recent study has suggested that oestrogen may be effective as an adjunct to atypical antipsychotic medications in reducing the psychotic symptoms experienced by women with established psychosis (Kulkarni et al, Reference Kulkarni, Riedel and de Castella2001, Reference Kulkarni, Riedel and de Castella2002). Oestrogen might therefore have a neuroprotective role in the treatment of women at ultra-high risk.
Investigators at the H-RAP Clinic in New York believe that the development of specific preventive interventions is premature at present. Instead, they have chosen a ‘naturalistic’ approach to study the appropriateness and efficacy of various potential treatments for young people at ultra-high risk. Thus, the treatment provided by psychiatrists to young people meeting RAP criteria is surveyed but RAP do not seek to direct the type of treatment provided. The mental state of over 80% of the patients recruited to RAP has either improved or stabilised over time (Reference CornblattCornblatt, 2002). Over 80% of patients received a pharmacological treatment, either antipsychotic medication or an anti-depressant, with both demonstrating clinical improvements (Reference CornblattCornblatt, 2002). The authors of this study suggest that this indicates that antidepressants may be effective in treating the underlying vulnerability to schizophrenia and should be considered when developing preventive interventions. It should be noted that many of these young people–particularly the group labelled as ‘schizophrenia-like psychosis’ or SLP–would be seen as already psychotic within the PACE framework and clearly requiring antipsychotic medication in other clinical settings.
Intervention trials
The first randomised controlled trial with a high-risk cohort was conducted at the PACE Clinic between 1996 and 1999. In this trial a combined intensive psychological (cognitive) treatment plus very low-dose atypical antipsychotic (risperidone) medication (specific preventive intervention or SPI: n=31) was compared with the effect of supportive therapy (needs-based intervention or NBI: n=28) on the development of acute illness in the high-risk group. At the end of the 6-month treatment phase, significantly more subjects in the NBI group had developed an acute psychosis than in the SPI group (P=0.026). This difference was no longer significant at the end of a post-treatment 6-month follow-up period (P=0.16), although it did remain significant for the risperidone-adherent subgroup of cases. This result suggests that it is possible to delay the onset of acute psychosis in the SPI group compared with the NBI group. Both groups experienced a reduction in global psychopathology and improved functioning over the treatment and follow-up phases compared with entry levels (Reference McGorry, Yung and PhillipsMcGorry et al, 2002). Longer-term follow-up of the participants in this study is now taking place. A second randomised trial commenced in 2000. This is a more sophisticated study with three treatment groups and blind randomisation to these groups. The three groups are: (a) risperidone (antipsychotic medication up to 2 mg daily) and CBT; (b) placebo and CBT; and (c) placebo and befriending. All treatments are offered for 12 months and participants are then monitored for a further 12 months to determine the long-term impact of the treatment.
The first double-blind, placebo-controlled clinical trial using antipsychotic medication has been completed at the PRIME Clinic. This study randomly allocated participants who met Criteria of Prodromal Symptoms (COPS) to receive either olanzapine or placebo for 12 months followed by a 12-month monitoring period. Three reports have been published to date which detail the study rationale and design (Reference McGlashan, Zipursky and PerkinsMcGlashan et al, 2003), baseline characteristics of the prodromal sample (Reference Miller, Zipursky and PerkinsMiller et al, 2003) and effects of olanzapine v. placebo in the first 8 weeks of the double-blind phase (Reference Woods, Breier and ZipurskyWoods et al, 2003).
Meanwhile, in the UK, the Manchester EDIE trial has compared the impact of cognitively oriented psychotherapy with monitoring alone, i.e. no psychological treatment, on the rate of transition to psychosis in 23 young people meeting ultra-high-risk criteria (Reference FrenchFrench, 2002; Reference Morrison, Bentall and FrenchMorrison et al, 2002). After 26 sessions of CBT only 1 of the 13 participants (8%) in this group had developed acute psychosis compared with 4 of the 11 in the monitoring group (36%) (Reference FrenchFrench, 2002). These results are encouraging as they suggest that pharmacological treatment might not be necessary to assist all young people in the prepsychotic phase of illness.
DISCUSSION
Ethical issues
Obviously, there are many ethical questions surrounding this clinical research endeavour. They have been at the forefront of the planning and development of the clinical research programmes described above. These considerations have been addressed at a number of forums and in journal articles (Reference DeGraziaDeGrazia, 2001; Reference Heinssen, Perkins and AppelbaumHeinssen et al, 2001; Reference McGlashanMcGlashan, 2001; Reference McGorry, Yung and PhillipsMcGorry et al, 2001b ; Reference Schaffner and McGorrySchaffner & McGorry, 2001; Reference Wyatt and HenterWyatt & Henter, 2001; Reference Bentall and MorrisonBentall & Morrison, 2002). Important questions remain about treatment options, the treatment of minors, the provision of information regarding risk of illness to individuals at ultra-high risk and the potential for stigmatisation of these individuals.
These are all legitimate areas of concern. Currently, it remains unclear whether the risk/benefit profile of neuroleptic treatments means that they should be prescribed and for how long, but there is sufficient evidence to suggest that clinical trials are warranted. The clinical treatment of young people identified as being at high risk of developing a psychotic disorder, particularly the use of neuroleptics, should be provided only in the context of a research trial, where standards of informed consent and monitoring are highest. Experience at the PACE Clinic has shown that sometimes young people are prescribed antipsychotic medication by psychiatrists and even general practitioners in the absence of a clear-cut psychotic disorder when the prescribing physician suspects that a psychotic disorder is emerging. It is imperative that such treatment be first investigated in an evidence-based manner. The effects of stigma also need to be examined. In some settings, if there is an inappropriately pessimistic mindset linked to the diagnosis of schizophrenia or psychotic disorder (a widespread phenomenon still), or the treatment setting is of poor quality or stigmatising, there may possibly be iatrogenic effects of this type. Such impact has not been seen in the PACE Clinic but this reassuring experience cannot necessarily be generalised and, indeed, needs to be demonstrated empirically.
Until recently, some major grant-giving bodies baulked at funding intervention research in the prepsychotic phase because of perceived ethical problems. In fact, not supporting the collection of vital evidence to guide clinical decision-making in such clinical samples can be viewed as perpetuating ethical dilemmas and confusion, as well as allowing non-evidence-based practice to flourish. This policy suggests that a double standard might exist for psychiatric disorders, since it clearly does not operate for early diagnosis in potentially serious medical illnesses. Similarly, the notion of funding ‘naturalistic’ studies where the use of antipsychotic medication in particular is freely permitted seems flawed and ethically inferior to conducting randomised controlled trials examining the use of anti-psychotics and other biological and psychosocial treatments in this phase. Naturalistic studies of this type (other kinds could be considered more useful) are inevitably going to produce confusing or inclusive results and have all the problems which were some years ago attributed to more rigorous research in this field (specially drug side-effects and potential stigma). Future support is required from the large independent research funding bodies, since this would enable necessary non-industry-funded studies to be conducted.
In conclusion, this paper reviews the development of an approach specifically designed for the detection, monitoring and treatment of the prepsychotic or prodromal phase of illness and the study of the psychobiological processes contributing to onset of psychosis in schizophrenia and related disorders. This is truly a growth area with the potential to benefit such symptomatic young people and their families. Increasingly, our ability to identify those at particularly high risk is being refined and a biological basis for psychosis onset investigated. Caution must be exercised, however, and each step evaluated in an evidence-based manner. Continued modification of ultra-high-risk criteria and better understanding of the process of screening and sample enrichment may be needed. Randomised controlled trials of medication and other interventions must be ongoing and rigorously evaluated. Large-scale screening of population samples in order to expand the scope of prepsychotic treatment is probably not justified merely for this purpose at this stage of knowledge. As an alternative, either enriching strategies could be developed to enable interventions to be evaluated, or a broader screening strategy for the full range of emergent mental disorders in young people could be explored. We expect this area of psychiatry to progress steadily over the next few years.
APPENDICES
Appendix 1: Potential advantages of prepsychotic intervention
-
(a) An avenue for help is provided, irrespective of whether transition ultimately occurs, to tackle the serious problems of social withdrawal, impaired functioning and subjective distress that otherwise become entrenched and steadily worsen prior to the onset of frank psychotic symptoms.
-
(b) Engagement and trust is easier to develop and lays a foundation for later therapeutic interventions, especially drug therapy, if and when required. The family can be similarly engaged and provided with emotional support and information instead of in a highly charged crisis situation.
-
(c) If psychosis develops, it can be detected rapidly and duration of untreated psychosis minimised and hospitalisation and other lifestyle disruption avoided. A crisis with behavioural disturbance or self-harm is not required in order to gain access to treatment.
-
(d) Comorbidity, such as depression and substance misuse, can be effectively treated and the patient therefore gets immediate benefits. If psychosis worsens to the point of transition, the patient enters first-episode psychosis in better health with less distress and fewer additional problems.
-
(e) The prospective study of the transition process is enabled, including neurobiological, psychopathological and environmental aspects. Patients are less impaired cognitively and emotionally and are more likely to be fully competent to give informed consent for such research endeavours.
Appendix 2: Obstacles to prepsychotic intervention
-
(a) False-positive rate for first-episode psychosis remains substantial. Are falsely identified individuals helped or harmed by involvement in clinical strategies? Receiving treatment at this time may heighten stigma or personal anxiety about developing psychosis or schizophrenia. If exposed to drug therapies, especially antipsychotic medications, adverse reactions may occur without benefit in false-positive cases.
-
(b) If the false-positive rate is reduced, then the accurate detection rate may decrease. This is a mathematical feature of the screening process, even when this is based on encouraging help-seeking for this group. Even with enrichment or successful screening, most of the ‘cases’ will still emerge from the low-risk group. Solution may be two- to three-step sequential screens with a continuous entry mechanism. Even if there is a ceiling for the proportion of cases that can be detected and engaged at this phase there will still be some advantages.
-
(c) Cannot distinguish between false-positives and false false-positives (in the latter case a true vulnerability exists although it has not yet been fully expressed) (Reference Yung and McGorryYung & McGorry, 1996).
-
(d) Lessons from early intervention in cancer, coronary heart disease and stroke not yet translated to psychosis and schizophrenia.
Appendix 3: Defining the onset of psychosis prospectively
Situations that complicate the definition:
-
(a) gradual onset of symptoms, especially symptoms which seem to evolve out of underlying personality;
-
(b) fluctuations in intensity and frequency of the symptoms;
-
(c) fluctuations in level of insight into the symptoms;
-
(d) individual may not be aware that the experiences are unusual or abnormal;
-
(e) individual may attribute them to a variety of sources, some plausible;
-
(f) observers may attribute the symptoms to a range of plausible explanations;
-
(g) one individual may not be distressed by the same type of symptoms that another would be disturbed by;
-
(h) individual may not have the language to describe the phenomena;
-
(i) individual may not be disabled by or seek help for the symptoms.
Appendix 4: PACE Clinic criteria for the ultra-high-risk group
Aged between 14 and 29 years Referred to a specialised service for help Meets criteria for one or more of the following three groups:
-
1. Attenuated psychotic symptoms (APS)
-
(a) Presence of at least one of the following symptoms: ideas of reference, odd beliefs or magical thinking, perceptual disturbance, paranoid ideation, odd thinking and speech, odd behaviour and appearance.
-
(b) Frequency of symptoms: at least several times per week.
-
(c) Recency: present within the past year.
-
(d) Duration: present for at least 1 week and no longer than 5 years.
-
-
2. Brief limited intermittent psychotic symptoms (BLIPS)
-
(a) Transient psychotic symptoms: presence of at least one of the following: ideas of reference, magical thinking, perceptual disturbance, paranoid ideation, odd thinking and speech.
-
(b) Duration of episode of less than 1 week.
-
(c) Frequency of symptoms: at least several times per week.
-
(d) Symptoms resolve spontaneously.
-
(e) Recency: BLIPS must have occurred within the past year.
-
-
3. Trait and state risk factors
-
(a) Schizotypal personality disorder in the identified individual or a first-degree relative with a psychotic disorder.
-
(b) Significant decrease in mental state or functioning: maintained for at least 1 month and no longer than 5 years.
-
(c) Recency: the decrease in functioning occurred within the past year.
-
Appendix 5: PACE Clinic inclusion criteria according to Comprehensive Assessment of At Risk Mental States (CAARMS) scores
-
1. Attenuated psychotic symptoms
-
(a) Subthreshold psychotic symptoms: Severity Scale Score of 3–5 on Disorders of Thought Content subscale, 3–4 on Perceptual Abnormalities subscale and/or 4–5 on Disorganised Speech subscales of the CAARMS; plus
-
(b) Frequency Scale Score of 3–6 on Disorders of Thought Content, Perceptual Abnormalities and/or Disorganised Speech subscales of the CAARMS for at least a week; or
-
(c) Frequency Scale Score of 2 on Disorders of Thought Content, Perceptual Abnormalities and Disorganised Speech subscales of the CAARMS on more than two occasions; plus
-
(d) Symptoms present in the past year and for not longer than 5 years.
-
-
2. Brief limited intermittent psychotic symptoms (BLIPS)
-
(a) Transient psychotic symptoms: Severity Scale Score of 6 on Disorders of Thought Content subscale, 5 or 6 on Perceptual Abnormalities subscale and/or 6 on Disorganised Speech subscales of the CAARMS; plus
-
(b) Frequency Scale Score of 1–3 on Disorders of thought Content, Perceptual Abnormalities and/or Disorganised Speech subscales; plus
-
(c) Each episode of symptoms is present for less than 1 week and symptoms spontaneously remit on every occasion; plus
-
(d) Symptoms occurred during past year and for not longer than 5 years.
-
-
3. Trait and state risk factors
-
(a) First-degree relative with a psychotic disorder or schizotypal personality disorder in the identified patient (as defined by DSM–IV); plus
-
(b) Significant decrease in mental state or functioning: maintained for at least 1 month and not longer than 5 years (reduction in GAF Scale of 30% from premorbid level); plus
-
(c) The decrease in functioning occurred within the past year and has been maintained for at least 1 month.
-
Acute psychosis criteria
-
(a) Severity Scale Score of 6 on Disorders of Thought Content subscale, 5 or 6 on Perceptual Abnormalities subscale and/or 6 on Disorganised Speech subscales of the CAARMS; plus
-
(b) Frequency Scale Score of greater than or equal to 4 on Disorders of Thought Content, Perceptual Abnormalities and/or Disorganised Speech subscales; plus
-
(c) Symptoms present for longer than 1 week.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Young people at heightened risk of developing a psychotic disorder can be identified with a high level of confidence.
-
▪ Studies of psychological and pharmacological interventions aimed at prepsychotic individuals have shown promise in preventing further progression and in the treatment of presenting symptoms.
-
▪ Ethical issues about treatment options, the treatment of minors and the provision of information about risk status need to be considered when establishing clinical centres.
LIMITATIONS
-
▪ Although strategies for identifying prepsychotic individuals are associated with transition rates to acute psychosis of 22–54%, the false-positive rate remains substantial.
-
▪ It is uncertain whether receiving treatment at this time may heighten stigma or personal anxiety about developing psychosis or schizophrenia.
-
▪ It is uncertain whether exposure to drug therapy, especially antipsychotic medication, could result in adverse reactions in individuals who are wrongly identified as being in the prepsychotic phase.
Acknowledgements
The PACE Clinic is supported by grants from the National Health and Medical Research Council, Department of Human Resources (Victoria, Australia), Stanley Foundation and Janssen-Cilag Pharmaceuticals.






eLetters
No eLetters have been published for this article.