Despite various attempts to dispel them, stereotypes abound in medicine, possibly because it is such a rich and varied profession with many niches that attract all sorts of people. These guilty prejudices, that are invariably demeaning, are largely couched in humour. General practitioners are often seen as leather-patched, cardigan-sporting sandal wearers. Reference Blundell, Harrison and Turney1 Pathologists are grey and distant, maybe a little like Lurch from the Adams Family. Students tremble at the Sir Lancelot Spratt surgeon, as depicted in the Carry On films and the mad psychiatrist is more of a cliché than a stereotype. Reference Walter2
These ideas are all politically incorrect and although we often talk about them with our peers, it remains an off-the-record opinion. There are very few papers that explore these beliefs in a serious or systematic way, however considerable consistency in people's beliefs has been found. Reference Bellodi3 They also appear to be fairly stable across time; they are not confined to the UK and nor are they held just within the profession. It seems these stereotypes are a part of our collective understanding of these very particular roles and the fact that they abound points to a possibility that there are real differences.
Stereotypes tend to involve emotionally laden descriptors of behaviour that conjure an image of a personality. Measuring personality types would have been an interesting undertaking in its own right; however, more specifically, we are interested in the emotional behaviour of clinicians as this might shed light on how they fulfil their responsibilities.
Although there are drawbacks in a reductionist approach, we need to consider the ‘typical’ surgeon and psychiatrist. This will allow for a more manageable comparative study which will hopefully uncover some wider principles. As such, we would ask the reader to look at their own prejudices and not dismiss them as irrational, but try to understand what their presence might indicate. It should be emphasised at the outset that this exercise is done in a spirit of exploration and not attack.
A quote from a book review in the BMJ illustrates the surgeon beautifully:
‘“Thinking surgeon” is a phrase that invites a smirk. Surgeons like to cultivate their image as doers, not thinkers. In multidisciplinary discussions they generally brood for a long time before saying, “I'm only a simple surgeon but…” No one is fooled by this self-deprecation, which is a preamble to the surgeon cutting through the verbiage and getting to the heart of the matter.’ Reference Drife4
Surgeons are seen as doers: they make decisions and act on them. The above quote depicts a surgeon cutting their way through extraneous words that are a hindrance. To them there is a complex problem that can be simplified by focusing on just a few aspects; they are frustrated by diversions, which could cloud the picture and waste time.
Kovarik talked of a surgeon as having a personality that must make difficult decisions with inadequate data. Reference Kovarik5 Although there are fewer surprises these days, on opening up an abdomen to find an inoperable tumour, a good surgeon should ‘cut through’ the sea of grey allowing for a simpler black and white question. Is it this certainty that allows the surgeon to get to the heart of the matter so effectively?
Psychiatrists on the other hand are paid to listen. Reference Strange Khursandi6 Helping the patient and those around them, including the psychiatrist himself, gain a more nuanced and complex understanding of the difficulties is a vital part of the role. In 2006, Alan Louie wrote that
‘psychiatrists must explore their patients’ emotional landscape, encouraging them to experience tears, confront fears and verbalise anger. During this work, the psychiatrist also needs to manage his emotions and countertransference’. Reference Louie, Coverdale and Roberts7
Cutting through the verbiage will just damage this process and needs to be done only when unavoidable. It is by adopting a position of uncertainty that psychiatrists could be seen as turning the black and white into grey. Of course, there are still black and white management decisions, but these are normally resisted and it might be this that sets surgeons and psychiatrists apart. To some surgeons the idea of an hour-long appointment for an initial assessment might seem ridiculous, but often even this is not enough for the psychiatrist.
The concept of emotional intelligence can be traced back to 1920 when Thorndike considered that success could not be accounted for by IQ alone and that socially competent behaviour was also important. Reference Thorndike8 In the 1940s, Weschler described how there were non-intellective factors that influenced general intelligence. Reference Weschler9,Reference Weschler10 In 1983, Howard Gardner distinguished social intelligence from emotional intelligence, Reference Gardner11 and later in the 1990s, Salovey & Meyer proposed that emotional intelligence should include both inter- and intrapersonal intelligence. Reference Salovey and Mayer12 It was not until Goleman's bestselling book, Emotional Intelligence, Reference Goleman13 that the term became widespread.
It is generally agreed that emotional intelligence is a measure of the ability to recognise, understand and manage emotions in ourselves and others. Reference Emmerling and Goleman14 Reuven Bar-On defined it as ‘an array of personal, emotional and social competencies that enable one to cope with environmental demands’. Reference Bar-On15 Bar-On has gone on to develop one of the most widely used measures of emotional intelligence to date. Reference Bar-On16 This has been shown to provide a reliable and valid measure of socially and emotionally competent behaviour in the individual. Reference Bar-On17 To quote McMullen,
‘Essential requirements to sustaining ourselves as happy and successful doctors are the capacity to empathise, look after ourselves, and communicate effectively. All of this relates more to our EQ than our IQ’. Reference McMullen18
Reuven Bar-On has demonstrated emotional intelligence is significantly related to performance, not only in school and university, but also in the workplace. Reference Bar-On19 A study of middle managers in a large retail organisation demonstrated a significant relationship between an individual's emotional intelligence and their morale, stress and performance at work. Reference Dulewicz, Higgs and Slaski20 In the only meta-analysis of studies relating to emotional intelligence, the authors found that emotional intelligence should indeed be considered a valuable predictor of performance. Reference Van Rooy and Viswesvaran21 The role of emotional intelligence in leadership has been of particular interest; this role seems to become more important the more senior the leader. Reference Goleman, Mckee and Boyatzis22
The business world seems to have been at the vanguard of work in this area; however, there have been some recent attempts to apply these principles in medicine. North Eastern Ohio Universities College of Medicine developed and piloted a 34-item instrument for their applications process. They were able to identify characteristics which correlated with desirable personal attributes and interpersonal skills in the applicants. Reference Carrothers, Gregory and Gallagher23
In a rare study of its kind, a limited association was found between the physicians’ emotional intelligence and patient satisfaction. Although this study used a validated assessment tool, it was limited by a small sample size. Reference Wagner, Moseley, Grant, Gore and Owens24 In 1994, Lewis found that patients consistently identified good interpersonal skills on the part of the practitioner as an important and desirable quality. Reference Lewis25 A more recent study demonstrated that perceived empathy in physicians was associated with improved patient satisfaction and treatment adherence. The study went on to suggest that health providers who wish to improve patient satisfaction and treatment adherence should first identify components of their empathic communication which need improvement. Reference Kim, Kaplowitz and Johnston26
The Bar-On Emotional Quotient Inventory (EQ-i) has repeatedly been shown to provide a reliable and valid measure of socially and emotionally competent behaviour. Reference Dulewicz, Higgs and Slaski20 Similar to IQ testing, it is a self-report questionnaire which gives a score produced from subscales based on the components of emotional intelligence. There are 15 subscales which give rise to five composite factors (Table 1). It takes around 30 min to complete the 133-item test. The overall score (Total EQ) is standardised with a mean of 100.
Table 1 The components of the Bar-On Emotional Quotient Inventory (Bar-On EQ-i)Reference Bar-On 17
| Component | |
|---|---|
| 1. Intrapersonal | |
| i. Self-regard | The ability to respect and accept oneself as basically good. It is associated with feelings of security, inner strength and self-confidence |
| ii. Emotional self-awareness | The ability to recognise one's feelings and emotions, to differentiate between them and to know what caused them |
| iii. Assertiveness | The ability to express feelings, beliefs and thoughts. To defend one's rights in a non-destructive manner |
| iv. Independence | The ability to be self-directed and self-controlled in one's thinking/actions, and to be free of emotional dependency |
| v. Self-actualisation | The ability to realise one's potential capacities and is affiliated with feelings of self-satisfaction |
| 2. Interpersonal | |
| i. Empathy | The ability to be aware of, understand and to appreciate the feelings of others |
| ii. Social responsibility | The ability to act as a cooperative, contributing and constructive member of one's social group, even when one may not benefit personally |
| iii. Interpersonal relations | This ability to establish and maintain mutually satisfying relationships that are characterised by intimacy |
| 3. Stress | |
| i. Stress tolerance | The ability to withstand adverse events and stressful situations. This is similar to the concept of ‘ego strength’ and ‘positive coping’ |
| ii. Impulse control | The ability to resist or delay an impulse, drive or temptation to act |
| 4. Adaptability | |
| i. Reality testing | The ability to assess the correspondence between what is experienced and what objectively exists |
| ii. Flexibility | The ability to adjust one's emotions, thoughts and behaviour to changing situations and conditions |
| iii. Problem-solving | The ability to identify and define problems as well as to generate and implement potentially effective solutions |
| 5. General mood | |
| i. Optimism | The ability to look at the brighter side of life and to maintain a positive attitude, even in the face of adversity |
| ii. Happiness | Happiness combines self-satisfaction, general contentment and the ability to enjoy life |
Method
An initial pilot study was conducted with the aim of gaining experience in the use of the Bar-On EQ-i via the Multi-Health Systems (Berkshire, UK; www.mhs.com/mhs/) scoring organiser and to inform a power calculation. The data analysis of the pilot study did point towards some differences between psychiatrists and surgeons.
The aim of the study was to compare the emotional intelligence characteristics of psychiatrists and surgeons. This would be done by asking each group to complete the online Bar-On EQ-i assessment tool. Keeping in mind the power calculation, our aim was to recruit at least 50 psychiatrists and 50 surgeons. We envisaged difficulties with gender distribution, and decided to ensure that we recruited at least 50 male psychiatrists and 50 male surgeons.
Participants were recruited face to face, via letters sent out in the post and by email. The inclusion criteria were any doctor with active membership of their respective Royal College in any psychiatric or surgical specialty. The definition of psychiatric or surgical specialty was broad to provide a representative sample. For simplicity, doctors without membership of their respective Royal College were deemed not to be sufficiently representative of their specialty. Ethical approval was given by the West London Research Ethics Committee.
Participants were required to consent to the assessment and they could elect to receive their results. They were then provided with a web address and an access code to complete the Bar-On EQ-i. Each participant was able to create an additional unique identifying code to later facilitate the retrieval of their personal results; however, they remained anonymous to Multi-Health Systems at all times. Individuals were asked to complete age and gender as mandatory fields.
The study had a descriptive and comparative component. The descriptive component looked at the measures of location using medians and spread for all outcomes across the two groups. The comparative analysis utilised the Mann–Whitney test to compare all scales by group, and the Spearman's rank correlation looked for a relationship between Total EQ and age.
Results
Respondent characteristics and Total EQ
In total, 148 individuals were recruited to the study, with 90 psychiatrists and 58 surgeons, whose attributes are displayed inTable 2. It was more difficult to recruit female professionals into the study, most notably female surgeons. The psychiatrists were slightly older on average than the surgeons. There was no evidence of a difference in total emotional intelligence between psychiatrists and surgeons (P = 0.872). The median Total EQ scores for both groups were very similar, with psychiatrists scoring 101 (95% CI 97-104) and surgeons scoring 100 (95% CI 96-102).
Table 2 Respondent characteristics and total emotional intelligence
| Psychiatrists (n = 90) | Surgeons (n = 58) | Combined (n = 148) | |
|---|---|---|---|
| Male, n (%) | 55 (61) | 48 (83) | 103 (70) |
| Female, n (%) | 35 (39) | 10 (17) | 45 (30) |
| Age, years: median (IQR) | 34.5 (31-40) | 30 (29-35) | 33 (30-38.5) |
| Median Total EQ (95% CI) | 101 (97-104) | 100 (96-102) | 100 |
Furthermore, there was no evidence of a difference in total emotional intelligence between genders (P = 0.982), and there was no correlation with age (r s = 0.095; P = 0.250).
Emotional intelligence composite factors
The radar diagram (Fig. 1) displays the differences in composite scores between the two groups. Differences were found in the interpersonal and general mood composite factors. Psychiatrists had a higher interpersonal score (P = 0.085), while surgeons had a higher general mood score (P = 0.039).
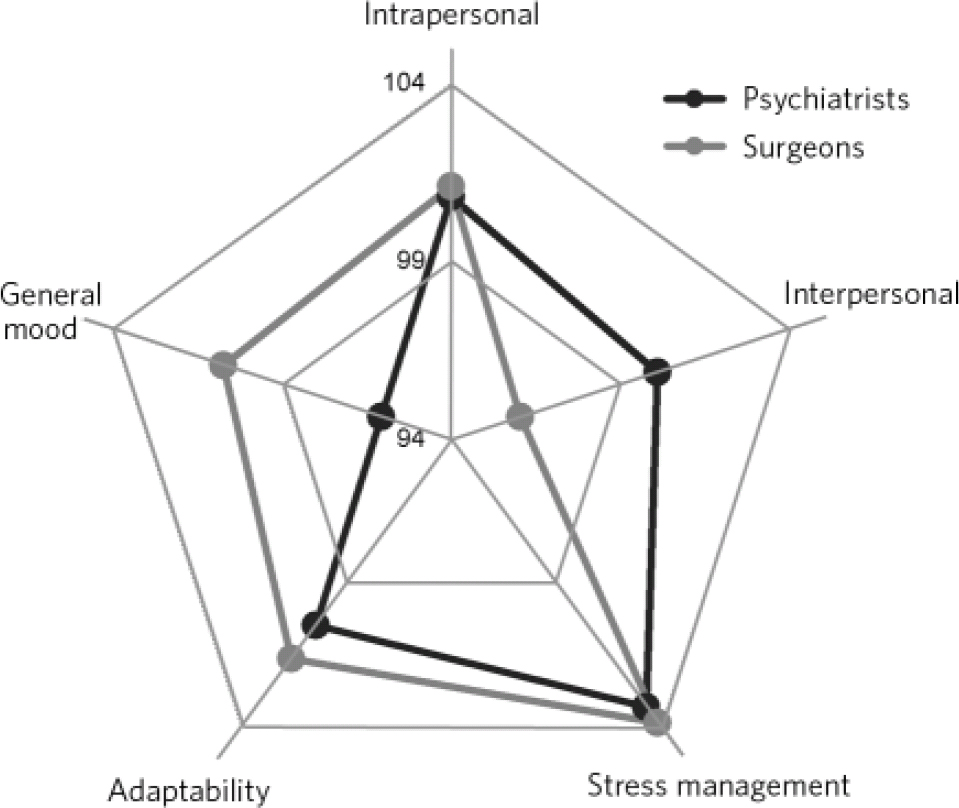
Fig 1 Differences between professionals across the five composite factors of emotional intelligence.
Emotional intelligence subscales
Psychiatrists scored significantly higher in the subscales of emotional self-awareness, empathy, social responsibility and impulse control. On the other hand, surgeons scored significantly higher in the subscales of self-regard, stress tolerance and optimism (Fig. 2). Significant results are displayed in Table 3.
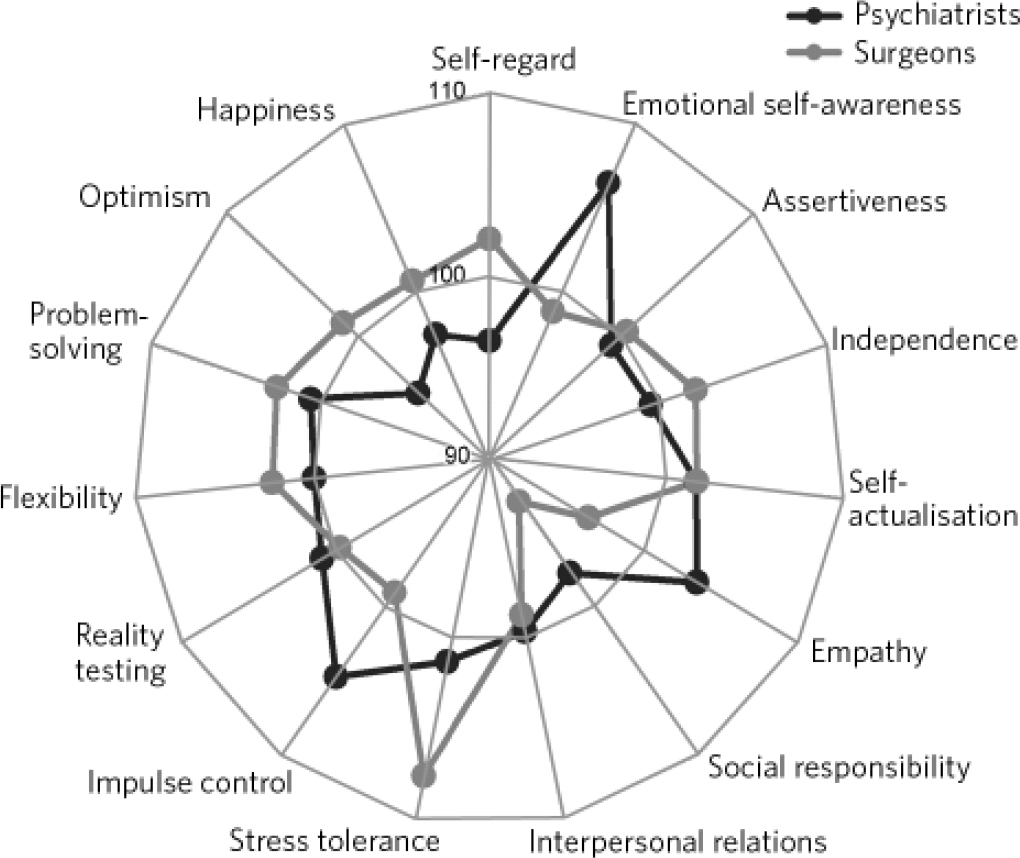
Fig 2 Differences between professionals across the 15 subscales of emotional intelligence.
Table 3 Statistics related to significant subscale differences
| Subscale | Psychiatrists Median score (95% CI) | Surgeons Median score (95% CI) | P |
|---|---|---|---|
| Emotional self-awareness | 107 (103-109) | 98 (95-102) | 0.002 |
| Empathy | 105 (102-109) | 98 (91-105) | 0.005 |
| Social responsibility | 100 (97-103) | 93 (90-99) | 0.040 |
| Impulse control | 107 (104-109) | 99 (94-103) | 0.011 |
| Self-regard | 98 (94-100) | 101 (98-107) | 0.005 |
| Stress tolerance | 102 (99-103) | 108 (104-112) | <0.0001 |
| Optimism | 96 (92-98) | 101 (96-106) | 0.009 |
Discussion
Total emotional intelligence is equal in both groups, suggesting a similar level of gross emotional functioning. This result is surprising for two reasons. First, doctors overall do not seem to fare better than average, as we know they do in IQ. Second, and perhaps more surprisingly, given that emotional understanding is the bedrock of psychiatry, one would have at least expected the psychiatrists to score higher than average.
This might be explained by medical school selection, with entry criteria potentially biased towards those with higher IQ, rather than higher EQ. It is known that medical students have higher than average IQs, but given our results, it is quite possible that there is not a similar relationship with EQ.
The fact that there is no difference between psychiatrists and surgeons is less surprising when one considers the many similarities between the two groups. Not only do both have a common grounding in medical training, but there are similar expectations within their working lives; from leading and supervising teams to managing the demands of patients and commissioners.
When looking at the constituents of emotional intelligence, a more complex picture emerges. This is particularly true of the subscales where the focus of this discussion will remain and it is here that we might make some sense of the respective stereotypes.
With that in mind, it is reassuring that psychiatrists do score higher than surgeons in emotional self-awareness and empathy. Much of their work deals with emotional problems and they are specifically trained in practising their emotional skills, of which self-awareness is a vital component. One would expect psychiatrists to be more empathic and emotionally reflective, thinkers and feelers as opposed to doers.
Just as reassuringly perhaps, surgeons score higher than psychiatrists in self-regard and stress tolerance. Decisions to operate cannot be taken with ambivalence; an effective surgeon needs to be confident and able to withstand extreme real-time pressures. This may in part rely on lower impulse control, as found in the surgeons; however, is this to the detriment of social responsibility?
A greater impulse control might allow the psychiatrist to bear uncertainty, which encourages more complex thoughts and feelings to surface in both patient and the psychiatrist. This is a position in which one is reflective, empathic, socially responsible and able to tolerate the desire to act on internal impulses. Although the surgeon heals patients by ‘doing’, the psychiatric patient is only healed, as such, when they are empowered.
Certain subscales are intuitively related to mood. It is striking that psychiatrists score lower in both happiness and optimism. Is this a reflection of the psychiatrist's greater self-awareness, which is painful at times, something akin to Klein's depressive position. Reference Klein27 This is not to say that surgeons do not have to deal with painful realities, it is merely that they adopt different strategies to deal with them, or does ‘cutting through’ depend on cutting off in an emotional sense? Furthermore, working on a daily basis with psychological pathology has a burden which may affect one adversely. It is also possible that the psychiatrist's self-selection might, in part, represent a more personal inner need. So the question comes down to one of cause or effect.
‘Medicine is not only a science, but also the art of letting our own individuality interact with the individuality of the patient.’ Dr Albert Schweitzer (1875-1965). Reference Cherniss, Goleman, Emmerling, Cowan and Adler28
This study has illustrated some interesting patterns associated with the roles of psychiatrists and surgeons. We are unable to say whether this is a state or trait phenomenon and in this respect a prospective study could be enlightening. We have provided objective evidence, which adds validity to the stereotypes. We would therefore like to suggest that these results represent important aspects of the respective roles, the implications of which we should take seriously. We would argue that the overall EQ score is not particularly important, but that the patterns within the subscales are. It is not only the strengths but also the weaknesses that allow for people to function appropriately within their professional positions.
Limitations
A limitation of this study is that it presupposes uniformity within specialties; they are not homogeneous groups. Clearly, there are other variables that merit exploration such as locality, seniority, subspecialty and professional focus. A broader investigation allowing for a more sophisticated multivariate analysis is required. Further analysis would involve looking at regression models to look at factors associated with being a psychiatrist or surgeon. Further limitations include a non-random sample selection and the difficulties recruiting female surgeons. One also wonders whether a bias may have resulted from the heavy reliance on computer literacy, given that the assessment tool was internet-based.
Implications
The basis of our social and emotional behaviour is laid down in infancy. It is resistant to change, but with a consistent, focused and sustained approach, change is possible through training. Reference Emmerling and Goleman14,Reference Cherniss, Goleman, Emmerling, Cowan and Adler28 It is here that tools like the EQ-i might have a place within healthcare. With this in mind, the EQ-i could be used to encourage insight in order to promote professional development. Michael Balint argued many years ago that by knowing ourselves better we can be more effective at work, and subsequently Balint groups have been widely adopted in general practice. Doctors who have taken part in reflective practice groups report an improved ability to listen to patients. Reference Cherniss, Goleman, Emmerling, Cowan and Adler28
The doctor-patient relationship is more complex than many would give credit. This study casts doubt over the view that doctors can hop between specialties with ease and begs the question of how recent reforms in medical training were validated. Medicine is not simply a technical endeavour and an apprenticeship system of training is arguably always going to be more sensitive to its demands. Using structured assessments in selection is crude and inherently flawed. Defining and selecting an ideal clinician in this way denigrates subjective experience and creates an unhealthy uniformity.
Given our experience of conducting this study, we feel that the concept of emotional intelligence could be better represented. Having acknowledged its utility in the corporate sector, we suggest caution before translation into a medical setting. We dispute the implied equivalence between IQ and EQ. When does self-regard become arrogance, assertiveness become bullying, and high impulse control descend into a lack of spontaneity? It needs to be highlighted that a low score in any domain can represent strength, it is context dependent. So we hope that instead of criticising the psychiatrists for ‘never doing anything’ or the surgeon for ‘not thinking’, one might consider this to be exactly the point.
Acknowledgements
We thank Multi-Health Systems for the use of the Bar-On EQ-i. We also thank Dr Kostas Tsilkos for his significant information technology contribution.








eLetters
No eLetters have been published for this article.