Introduction
According to the World Health Organization (WHO), reproductive health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity in all matters related to the reproductive system and to its functions and processes (World Health Organization, 2021). Reproductive health implies that people are able to have a satisfying and safe sex life and that they have the capability to reproduce and the freedom to decide if, when, and how often to do so. Despite the fact that, according to the WHO, the reproductive age in women lasts up to 49 years (World Health Organization, 2006), problems with the realization of reproductive rights in women may arise much earlier. After 35 years, most women experience a decline in sexual functions and deteriorating general health. Of course, this does not happen to everyone, but there is a high probability that a woman will face certain difficulties at this age. A slight decrease in reproductive function is noted from 27–28 years old, becoming even more pronounced at ages between 35 and 40 years old and, by the age of 45, the reproductive function approaches zero.
Recently, women have increasingly realized their reproductive function at a later reproductive age, when they have moved forwards in their career progression and acquired a certain material status necessary for full-fledged child care and upbringing. There are constant discussions about the expediency of motherhood in advanced reproductive age.
Significant numbers of factors affect the reproductive health state: socioeconomic, ecological, lifestyle, the level of medical literacy, the state of the organization, and the quality of the available medical care (Wu et al., Reference Wu, Zhang and Wang2000). These affect a woman’s fertility in a different manner, whilst age-related changes occur in everyone.
Age-related reasons for fertility declines in women
Negative changes accumulate in the oocyte’s genome with age. This reduces the fertilization possibility, normal embryo development should fertilization have been achieved, and implantation and healthy offspring birthrates (Franasiak et al., Reference Franasiak, Forman, Hong, Werner, Upham, Treff and Scott2014). However, within the cohort of developing embryos from this group of women, many blastocysts with a euploid chromosome set number are also unable to implant and develop into living embryos. Therefore age-related ooplasm abnormalities may also reduce oocyte competence, even after fertilization and progress to adversely affect embryonic development (Capalbo et al., Reference Capalbo, Rienzi, Cimadomo, Maggiulli, Elliott, Wright, Nagy and Ubaldi2014).
Age determines the deterioration of morphological and functional oocyte characteristics, and the embryos obtained from them has a multifactorial nature. It has been shown that the diameter of the cytoplasm and the thickness of the zona pellucida decrease linearly with the age of women (Valeri et al., Reference Valeri, Pappalardo, De Felici and Manna2011). Cell volume decrease may be due to changes in ion pump activity or the ability to regulate homeostatic water balance. The decrease in oocyte quality may be associated with impaired lipid metabolism and decreased melatonin in the follicular fluid (Cordeiro et al., Reference Cordeiro, Montani, Pilau, Gozzo, Fraietta and Turco2018; Zhang et al., Reference Zhang, Lu, Chen, Zhang and Xiong2020).
Despite the contribution of the paternal genome to the embryo chromosomal balance, it is considered that the mother’s age is the main cause of embryo aneuploidies. Age-related chromosomal abnormalities mainly arise because of meiotic impairments during oogenesis, following flawed chromosome segregation patterns such as non-disjunction, premature separation of the sister chromosome, or their reverse segregation (Cimadomo et al., Reference Cimadomo, Fabozzi, Vaiarelli, Ubaldi, Ubaldi and Rienzi2018). The chromosomal aberration rate in MII stage oocytes of advanced reproductive age patients varies from 4% to 62% (Kuliev et al., Reference Kuliev, Cieslak and Verlinsky2005). A cytogenetic analysis of unfertilized oocytes showed an increase in chromosomal abnormality rate with age (Petrushko, Reference Petrushko2003). It is believed that the risks of aneuploidy may be associated with a long delay in oocyte meiosis stage I, which occurs before ovulation (Pellestor et al., Reference Pellestor, Andréo, Arnal, Humeau and Demaille2003). It is known that oocyte telomeres begin to shorten over a lifetime due to the chronic effects of oxidative and genotoxic stress, the late exit of female gametes from the cell-cycle cessation, as well as reduced telomerase activity (Keefe et al., Reference Keefe, Marquard and Liu2006), cohesin dysfunction, and meiotic spindle abnormalities (Keefe et al., Reference Keefe, Kumar and Kalmbach2015).
An evaluation of OCT4, SOX2, CDX2, GATA3, and YAP gene expression and the corresponding embryo proteins from young and advanced-age women showed that the expression of SOX2 and CDX2 genes in embryos at the morula stage in the group of women over 38 years old was statistically lower than in the group of younger patients (Gharanfoli et al., Reference Gharanfoli, Shahverdi, Dalman, Ghaznavi, Alipour and Eftekhari-Yazdi2020).
The most common specific abnormalities in embryos of women older than 36 years are sex chromosome monosomy (45,X), which accounts for almost 10% of all miscarriages, and trisomies 16, 21 and 22, which together account for 50% of all miscarriages detected in spontaneous abortions (Gharanfoli et al., Reference Gharanfoli, Shahverdi, Dalman, Ghaznavi, Alipour and Eftekhari-Yazdi2020).
Another theory of ageing causing changes in the cell, including oocytes, is the mitochondrial free radical theory of ageing (Barja, Reference Barja2014). According to this theory, reactive oxygen species (ROS) and various toxic byproducts of aerobic metabolism are probably involved in cellular damage to genomes and mitochondrial DNA (mtDNA) and are associated with mutations. The increased production of ROS caused a clear disruption in the respiratory chain of the cell, leading to the accumulation of mutations and unbalanced redox activity (Taylor and Turnbull, Reference Taylor and Turnbull2005; Fragouli et al., Reference Fragouli, Spath, Alfarawati, Kaper, Craig, Michel, Kokocinski, Cohen, Munne and Wells2015). Basal ROS levels often decline during the normal mitochondrial function phase within the respiratory chain, whilst an excess level of cellular ROS is determined by age and contributes to significantly increased oxidative damage and loss of cellular activity. Therefore, there was a change in mitochondrial function: a decrease in mitochondrial membrane potential (MMP), oxidative phosphorylation (OXPHOS), and the number of mtDNA copies in advanced-age women compared with younger women (May-Panloup et al., Reference May-Panloup, Boucret, Chao de la Barca, Desquiret-Dumas, Ferré-L’Hotellier, Morinière, Descamps, Procaccio and Reynier2016). This coincided with lower mtDNA levels for advanced-age women in embryos at the early cleavage stage, but paradoxically the opposite was observed at the blastocyst stage, with higher mtDNA levels associated with increased aneuploidy and failed implantation (Fragouli and Wells, Reference Fragouli and Wells2015; Liu et al., Reference Liu, Han, Li, Wang, Ma, Zhang, Guo, Wang, Wang, Duan, Xu, Yin and Yao2017).
ART features for advanced reproductive age women
Increases in serum progesterone and estradiol levels were observed in advanced reproductive age patients (Chahal and Drake, Reference Chahal and Drake2007). These patients have a poor response to stimulation for superovulation (Seifer et al., Reference Seifer, Baker and Leader2011). The oocyte fertilization rate was significantly lower in patients aged more than 36 years compared with younger women (Asada et al., Reference Asada, Tokoro, Sonohara, Fukunaga, Hattori and Hashiba2019). All of these factors led to the fact that the effectiveness of ART programmes in women over 40 years old was ∼5% (Zhang et al., Reference Zhang, Choo and Yang2015). These unsuccessful ART outcomes have pushed reproductive specialists and scientists to carry out scientific research to improve reproductive indicators for advanced-age women. Among the existing approaches, two main ones can be distinguished: (1) methods allowing the preservation of reproductive cells at a younger age using ART intervention and cryobanking; and (2) methods aimed at improving the existing functional indicators of oocytes and embryos of advanced-age women to aid optimal selection during ART.
Cryotechnology as the basis for preserving the reproductive potential of advanced-age women
Economically developed countries have passed laws on reproductive health protection. Scientists are developing methods to preserve reproductive health and prolong it for the longest possible period. Modern methods of preserving reproductive health and prolonging the reproductive period of women are based on cryotechnology.
Oocyte freezing for so-called ‘social reasons’ in female groups applies to women who seek to prolong, protect, and secure their fertility for later years (Simopoulou et al., Reference Simopoulou, Sfakianoudis, Bakas, Giannelou, Papapetrou, Kalampokas, Rapani, Chatzaki, Lambropoulou, Lourida, Deligeoroglou, Pantos and Koutsilieris2018). In 2013, the American Society for Reproductive Medicine, for the first time, approved the cryopreservation of oocytes as non-experimental (American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology, 2013). Experience has shown that the cryopreservation of oocytes is a promising area for maintaining female fertility. However, it is important not only to obtain a high survival rate of oocytes after cryopreservation and preserve their main function but also to ensure the absence of the negative effects of cryopreservation factors on the genome of embryos that will develop from oocytes after long-term, low-temperature storage.
Data on the chromosomal status of embryos derived from cryopreserved oocytes are quite contradictory. Some studies have found that cryopreservation factors can induce meiotic spindle abnormalities and chromosome disorganization in human oocytes, which, in turn, may increase the appearance of embryos with aneuploid chromosome set numbers (Bromfield et al., Reference Bromfield, Coticchio, Hutt, Sciajno, Borini and Albertini2009). However, we have previously shown that the level of chromosomal aneuploidy of embryos derived from cryopreserved and fresh oocytes did not exhibit significant differences (Buderatska et al., Reference Buderatska, Gontar, Ilyin, Lavrinenko, Petrushko and Yurchuk2020). It should be noted that these results were obtained in a study of women with a mean age of 27.6 ± 4.8 years.
There are very few data in the scientific literature on autologous oocyte cryopreservation for advanced-age women with successful pregnancy and childbirth (Parmegiani et al., Reference Parmegiani, Cognigni, Bernardi, Ciampaglia, Pocognoli and Filicori2009).
Recent publications have reported that the survival rate after cryopreservation has increased in recent years, which confirmed the influence of methodological approaches to female gamete cryopreservation provided using optimal ART (Pai et al., Reference Pai, Baid, Palshetkar, Pai, Pai and Palshetkar2021). The turning point in the improvement of oocyte cryopreservation methods was the use of vitrification (Kuleshova et al., Reference Kuleshova, Gianaroli, Magli, Ferraretti and Trounson1999). The absence of ice crystal formation when the temperature was lowered to −196°С and at the stage of warming made it possible to reduce the level of cell damage and significantly increase the efficiency of oocyte cryopreservation compared with slow freezing (Levi-Setti et al., Reference Levi-Setti, Patrizio and Scaravelli2016). Also, using different techniques prior to cryopreservation of oocytes and embryos at various preimplantation stages could help to preserve their functional characteristics in younger age women (Petrushko et al., Reference Petrushko, Yurchuk, Buderatska and Piniaiev2018, Reference Petrushko, Yurchuk, Piniaiev and Buderatska2019). It should be noted that the state of the endometrium is also very important when transferring embryos and contributes to the level of implantation. Women older than 38 years have reduced implantation (6.5% vs. 10.9%, P = 0.01) and pregnancy (10.1 vs. 18.7%, P = 0.02) rates compared with younger women (Borini et al., Reference Borini, Levi Setti, Anserini, De Luca, De Santis, Porcu, La Sala, Ferraretti, Bartolotti, Coticchio and Scaravelli2010). More optimistic results of the incidence of pregnancy are given in the work by Rienzi and colleagues, who found 12.6% for women in the older group compared with 27.5% for women younger than 38 years (Rienzi et al., Reference Rienzi, Cobo, Paffoni, Scarduelli, Capalbo, Vajta, Remohí, Ragni and Ubaldi2012).
The results of oocyte cryopreservation, depending on the woman’s age revealed that ‘take home baby’ rate ranged from 5% to 17% in patients older than 40 years. The birth rate in patients aged 41–42 years was 2–3% lower than in patients aged 37–40 years (Cil and Seli, Reference Cil and Seli2013).
Data from the United States Reproductive Technology Association in 2013 showed that live birth rate in cycles with fresh embryos from non-donor oocytes decreased from 21% at the age of 38–40 to 11% at the age of 41–42, with a further reduction to 4.5% for age over 42 years.
The cryopreservation of oocytes by social indicators at younger age and subsequent in vitro fertilization and embryo transfer gives women who expect to become pregnant at an advanced age two important benefits: becoming genetic parents to their own offspring and reducing the risk of having children with chromosomal abnormalities associated with aneuploidy. In addition, freezing oocytes may be the best alternative for women who do not have a partner at a particular stage in life or who have moral prejudices about embryo cryopreservation (Buderatska and Petrushko, Reference Buderatska and Petrushko2016).
The use of cryotechnology to preserve women’s fertility at a young age is not limited to the cryopreservation of oocytes. In contrast with the ‘social reasons’ for postponing conception, there are also medical ones, in which there are some contraindications for induction of superovulation to obtain mature oocytes. In these cases, ovarian tissue cryopreservation (OTC) is recommended before gonadotoxic therapy to further aid transplantation after recovery at an older age (Kim et al., Reference Kim, Lee, Lee and Kim2018a). OTC also can be offered as an alternative to preserve fertility in young patients at risk of premature ovarian insufficiency. However, despite significant advances in the development of methods for OTC, slightly more than 130 children have been born to date. Restored fertility using OTC could be realized by ovarian tissue transplantation or in vitro maturation followed by in vitro fertilization. It should be noted that transplantation of ovarian tissue has some contraindications, especially when the ovary is part of the malignancy. The efficiency of the OTC procedure is questionable at more than 36 years of age, and it is still considered experimental in many countries, where legislation and regulations vary (ESHRE Guideline Group on Female Fertility Preservation et al., Reference Anderson, Amant, Braat, D’Angelo, Chuva de Sousa Lopes, Demeestere, Dwek, Frith, Lambertini, Maslin, Moura-Ramos, Nogueira, Rodriguez-Wallberg and Vermeulen2020).
Techniques improving the oocyte and embryo quality of advanced-age women
Methods for improving fresh or cryopreserved oocyte and embryo quality are proposed. For example, methods are co-culture systems with Vero, oviduct and endometrium cells (Moshkdanian et al., Reference Moshkdanian, Nematollahi-mahani, Pouya and Nematollahi-mahani2011); microsurgical removal of fragmentation in day 2 embryos (Kim et al., Reference Kim, Kim, Park, Kwak, Yoo, Park, Sun, Kim, Lee, Park and Chi2018b); and individualization of the embryo day transfer, etc. (Yoon et al., Reference Yoon, Yoon, Son, Kim, Im and Lim2001). The most promising method of oocyte renewal takes into consideration that the mitochondrial free radical theory of ageing is mitochondrial replacement therapy (MRT). It is known that, unlike the nuclear genome that is inherited equally from both parents, the mitochondrial genome is transmitted mainly from the mother’s gamete (Zou et al., Reference Zou, Slone, Cao and Huang2020). Mitochondrial DNA is circular in structure and contains 37 genes that control the production of proteins involved in energy metabolism. Therefore an mtDNA mutation can affect organs that depend on it, giving rise to several incurable diseases such as deafness, diabetes mellitus, myopathies, glaucoma, and others (Costa et al., Reference Costa, Santana, Vilanova and Parente2016). MRT could be performed using several techniques, each of which has advantages and disadvantages.
Ooplasm transfer
The first donor cytoplasm that contained healthy mitochondria along with sperm was transferred in 1997 to a 39-year-old recipient’s oocyte cytoplasm using the ICSI procedure (Cohen et al., Reference Cohen, Scott, Schimmel, Levron and Willadsen1997). In this case, the reconstituted zygote contained the original parent’s nuclear DNA and mixed mtDNA from both donor and recipient oocytes. However, this technology was later banned due to mitochondrial heteroplasm with two types of mtDNA and chromosomal abnormalities in future offspring (Barritt et al., Reference Barritt, Brenner, Malter and Cohen2001; Mobarak et al., Reference Mobarak, Heidarpour, Tsai, Rezabakhsh, Rahbarghazi, Nouri and Mahdipour2019).
Meiotic spindle transfer
The first live birth case in humans using meiotic spindle transfer was reported by Zhang et al. (Reference Zhang, Liu, Luo, Chavez-Badiola, Liu, Yang, Munne, Konstantinidis, Wells and Huang2016a) in a 36-year-old woman diagnosed with Leigh syndrome. The metaphase II meiotic spindle was extracted from the recipient’s oocyte and transferred to a healthy donor oocyte with a pre-removed own spindle. After fertilization of the reconstructed oocyte using ICSI, the resulting zygote contained mitochondria from a healthy donor and the original nuclear DNA of the parents. Using this MRT method, less than 1% of maternally affected mtDNA was transferred to the offspring (Craven et al., Reference Craven, Tang, Gorman, De Sutter and Heindryckx2017). However, this indicator of the maternal mtDNA content may fluctuate, depending on technical aspects such as the competency of the embryologist involved.
Polar body transfer (PBT)
To perform PBT, the first polar body of the recipient’s oocyte is transferred to the enucleated donor’s oocyte. After that, the reconstructed oocyte is fertilized using the ICSI method. In addition to the first PBT, it is possible to carry out the transfer of the second PB. After fertilization, the recipient’s oocyte secretes the second polar body, which is extracted and transferred to the donor’s zygote with the previously removed female pronucleus. PBT has several advantages, such as minimum transfer of affected patient mtDNA as the PB includes few mtDNA copies and PBT yields undetectable carryover of donor mtDNA in two generations (Wang et al., Reference Wang, Sha, Ji, Zhang, Chen, Cao and Zhu2014). Also, PBT leads to less chromosomal damage due to the PB structural features and location. Moreover, for the first PBT, this technique could be used to double the number of oocytes for poor responders with the absence of mtDNA abnormalities.
Pronuclear transfer (PNT)
This technology of mitochondrial transfer is based on the fact that the pronuclei of one zygote are transferred to another enucleated zygote. To do this, a donor oocyte and an oocyte with disturbed mitochondrial DNA are fertilized with the sperm of the future father. Shortly after the appearance of the pronuclei, a pronuclear transfer is carried out into the zygote obtained from the donor oocyte. Therefore, the embryo carries the nuclear DNA from the parents, and the donor’s mitochondrial DNA.
This technique has some advantages, as pronuclei are visualized well under a light microscope without the use of additional equipment, and the fertilization procedure can be performed using ICSI as well as IVF. However, from an ethical point of view, the implementation of this technique requires the destruction of the embryo at the zygote stage, and it is this method of mitochondrial transport that has the greatest limitations in some efforts (Ishii and Hibino, Reference Ishii and Hibino2018). In addition, for the fusion of pronuclei and donor cytoplasm, the inactivated viral vector SeV (Sendai virus, also known as HVJ-E) is used (Tachibana et al., Reference Tachibana, Sparman, Sritanaudomchai, Ma, Clepper, Woodward, Li, Ramsey, Kolotushkina and Mitalipov2009; Craven et al., Reference Craven, Tuppen, Greggains, Harbottle, Murphy, Cree, Murdoch, Chinnery, Taylor, Lightowlers, Herbert and Turnbull2010). The absence of viral genetic material has been shown previously (Tachibana et al., Reference Tachibana, Sparman, Sritanaudomchai, Ma, Clepper, Woodward, Li, Ramsey, Kolotushkina and Mitalipov2009).
The first report of a successful pregnancy with a fetus bearing a normal karyotype and low heteroplasia rate was received in 2016 in a 30-year-old woman who had had two unsuccessful IVF attempts (Zhang et al., Reference Zhang, Zhuang, Zeng, Grifo, Acosta, Shu and Liu2016b), as a result of which all resulting embryos halted development at the two-cell stage.
Germinal vesicle transfer (GVT)
Immature oocytes in prophase I of the first meiosis have a nucleus that stays in the form of a ‘germinal vesicle’ until meiosis resumption. GVT is removed and transferred to a donor oocyte with a previously extruded germinal vesicle. The ooplast and karyoplast merger is conducted using electrofusion with an electro-cell manipulator then the reconstructed oocyte undergoes in vitro maturation followed by fertilization.
This technique was first applied for advanced reproductive age women by Zhang et al. (Reference Zhang, Wang, Krey, Liu, Meng, Blaszczyk, Adler and Grifo1999), however the reconstructed oocytes did not reach the mature stage.
The advantage of GVT is that it can be performed before the onset of meiosis I (MI). As mitochondria play an important role in chromosome segregation, the restoration of mitochondria prior to meiosis I may contribute to a higher level of the euploid set of oocyte chromosomes and the development of a normal embryo after fertilization (Tanaka and Watanabe, Reference Tanaka and Watanabe2018). Whether GVT can save chromosomal abnormalities in age-related oocytes needs further study.
AUGMENT technology
Autologous germline mitochondrial energy transfer (AUGMENT) is the strategy launched by OvaScience in 2014 to transfer producing energy mitochondria from the autologous egg precursor cells into the oocytes. This action has been shown to enhance the quality of the egg and the fetus (Fakih et al., Reference Fakih, Shmoury, Szeptycki, dela Cruz, Lux, Verjee, Burgess, Cohn and Casper2015; Cozzolino et al., Reference Cozzolino, Marin and Sisti2019). The results from other researchers have indicated the lack of a positive effect on fertilization and development of euploid embryos for patients whose average age was 36.3 ± 3.6 years. Further studies on the effectiveness of this method on the oocytes of older women that are characterized using a pronounced decrease in energy reserves are required (Labarta et al., Reference Labarta, de Los Santos, Herraiz, Escribá, Marzal, Buigues and Pellicer2019).
Autologous mitochondrial injections are also performed with the use of cumulus and granulose cells that improve the fertilization rate, the quality of the embryos for 3 days, and the pregnancy rate (Tian et al., Reference Tian, Liu, Ye, Fu, Sheng, Wang, Wang, Heng and Liu2019; Tzeng et al., Reference Tzeng, Hsieh, Au, Yen, Chang and Cheng2004). However, the use of autologous mitochondrial injections is not recommended for mitochondrial mutations, which can increase with age.
Stem cells for germ cell production
Another alternative direction for the reproduction of advanced-age women is the reconstitution of gametogenesis in vitro. In the renewal of the ovarian reserve and the competence of germ cells, the production of mature gametes from germ cell progenitor stem cells, embryonic stem cells, the tail tip of fibroblasts, or even by reprogramming granulosa cells into oocytes is important (Hayashi et al., Reference Hayashi, Ogushi, Kurimoto, Shimamoto, Ohta and Saitou2012; Hikabe et al., Reference Hikabe, Hamazaki, Nagamatsu, Obata, Hirao, Hamada, Shimamoto, Imamura, Nakashima, Saitou and Hayashi2016; Tian et al., Reference Tian, Liu, Ye, Fu, Sheng, Wang, Wang, Heng and Liu2019). Successful in vitro reconstitution of primordial germ cells has recently had a significant effect on the field. The authors demonstrated the entire process of mammalian oogenesis in mice in vitro from primordial germ cells, in which the birth of fertile offspring was obtained from a cultured gonad (Morohaku et al., Reference Morohaku, Tanimoto, Sasaki, Kawahara-Miki, Kono, Hayashi, Hirao and Obata2016).
Skin-derived stem cells (SDSCs) constitute a heterogeneous population of stem cells generated in vitro from the dermis, which can be cultured as spherical aggregates of cells in suspension culture. Under certain in vitro or in vivo conditions, SDSCs show multipotency and can generate a variety of cell types (Ge et al., Reference Ge, Cheng, Dyce, De Felici and Shen2016). It has been shown that SDSCs are able to produce primordial germ cell-like cells in vitro, and even oocyte-like cells. Whether these germ cell-like cells can give rise to viable progeny remains, however, unknown.
Using platelet-rich plasma (PRP) therapy for fertility preservation of advanced-age women
Ovarian tissue rejuvenation due to the paracrine effect of PRP has become a fairly new and actively developing direction (Cakiroglu et al., Reference Cakiroglu, Saltik, Yuceturk, Karaosmanoglu, Kopuk, Scott, Tiras and Seli2020).
Many studies have documented that the use of PRP can reduce the signs of inflammation, postoperative blood loss, and infection and, in addition, lead to accelerated osteogenesis and the healing of wounds and soft tissues (Park et al., Reference Park, Yang and Chung2011). Many articles have reported that PRP therapy implementation can enhance healing and the anti-ageing process using angiogenesis regeneration due to the multiple growth factors and cytokines involved (Du and Lei, Reference Du and Lei2020).
PRP realizes its effects due to cytokines and growth factors that are contained in platelet granules, such as transforming growth factor-β, insulin-like growth factors 1 and 2 (IGF-1 and IGF-2), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), hepatocyte growth factor (HGF), basic fibroblast growth factor (bFGF), granulocyte colony-stimulating factor (G-CSF), and many others (Amable et al., Reference Amable, Carias, Teixeira, da Cruz Pacheco, Corrêa do Amaral, Granjeiro and Borojevic2013; Ramaswamy Reddy et al., Reference Ramaswamy Reddy, Reddy, Babu and Ashok2018).
The addition of Ca2+ to PRP leads to the release of platelet granule contents and the activation of processes induced by growth factors (Amable et al., Reference Amable, Carias, Teixeira, da Cruz Pacheco, Corrêa do Amaral, Granjeiro and Borojevic2013). PRP cryopreservation can activate platelet granules in addition to the advantage of prolonged shelf life (Kelly and Dumont, Reference Kelly and Dumont2019; Kleinveld et al., Reference Kleinveld, Juffermans, Noorman and Vincent2020).
The use of PRP therapy could be applied in the fight against infertility of women with a poor response, premature ovarian insufficiency, and late reproductive age, who do not want to carry out the oocyte donation programme, and make it possible to improve the hormonal background and activate folliculogenesis in the ovaries (Melo et al., Reference Melo, Navarro, Jones, Coward and Coleman2020; Sills et al., Reference Sills, Petersen, Rickers, Wood and Li2020).
Given the inverse relationship between ageing, growth hormone concentration, and IGF-1 (Fanciulli et al., Reference Fanciulli, Delitala and Delitala2009), the use of PRP reached in various cytokines and growth factors, including IGF-1, for injections into ovarian tissue led to an increase in cell proliferation and the follicle development.
It was shown that the injection of autologous PRP into the ovarian tissue of women with limited ovarian reserve or absence of menstruation for more than 1 year improved fertility in all patients aged 42 ± 4 years. Therefore, 5.3 ± 1.3 MII oocytes and at least one embryo suitable for freezing were received for each patient in the IVF cycle at 78 days after treatment (Sills et al., Reference Sills, Rickers, Li and Palermo2018). Similar results were obtained by other authors, who reported an improvement in hormonal status and pregnancy rate, including natural rates, after PRP therapy in women with low ovarian reserve (Petryk and Petryk, Reference Petryk and Petryk2020). Since 2019, several cases of childbirth after PRP therapy have been published, as well as the onset of natural pregnancy in women who had premature menopause (Farimani et al., Reference Farimani, Heshmati, Poorolajal and Bahmanzadeh2019; Pantos et al., Reference Pantos, Simopoulou, Pantou, Rapani, Tsioulou, Nitsos, Syrkos, Pappas, Koutsilieris and Sfakianoudis2019).
Except for injection into the ovarian tissue, PRP could be used to increase the effectiveness of oocyte in vitro maturation methods, which is relevant for patients with polycystic ovary syndrome, poor responders, and fertility preservation for women of different reproductive ages (Yurchuk, Reference Yurchuk2021). It has been shown that the addition of PRP into the maturation medium increased the quality of mature bovine oocytes (gametes with high mitochondrial potential) and led to an improvement in bovine embryo development (Moulavi et al., Reference Moulavi, Akram, Khorshid Sokhangouy and Hosseini2020; Ramos-Deus et al., Reference Ramos-Deus, Santos Nascimento, Vieira, Chaves, Albuquerque, Ferreira-Silva, Grázia, Santos Filho, Batista, Teixeira and Oliveira2020) Therefore, despite encouraging achievements of in vivo and in vitro PRP used for improving the fertility of patients with advanced maternal age, more extensive database evidence is requested.
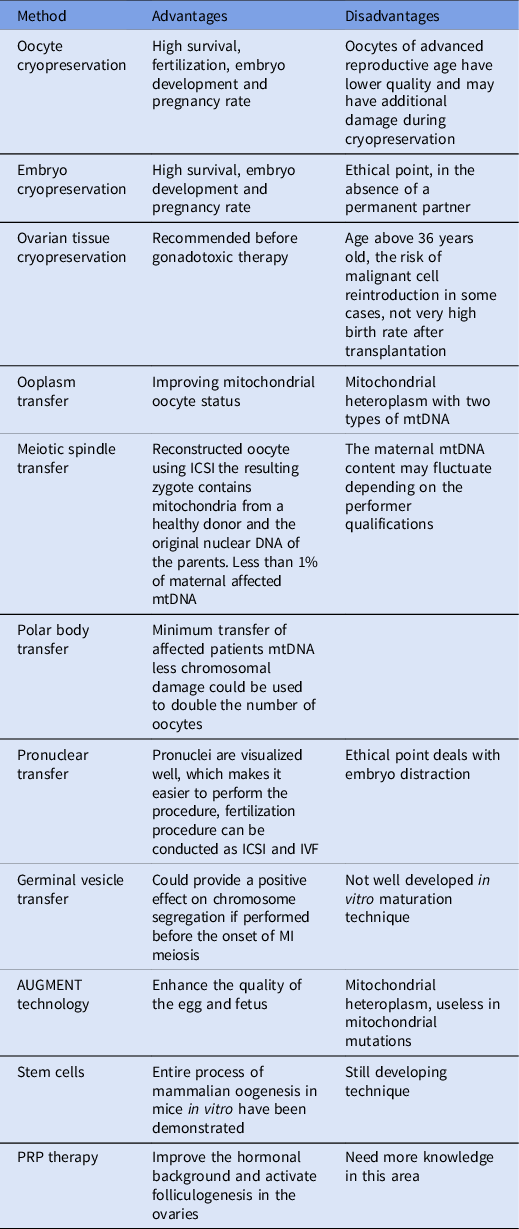
The advantages and disadvantages of the main methods for improving oocyte function and fertility potential are listed in Table 1.
Table 1 The advantages and disadvantages of the methods for fertility preservation and improvement of the oocyte competence of advanced age patients.
Conclusion
The possibility of the realization of reproductive function in women in the late reproductive period is one of the most urgent problems of modern science. Assisted reproductive technologies have advanced in the field, not only for infertility in young women but also in older patients. Some approaches have been aimed at improving the reproductive function of women of late reproductive age by preserving fertility at an early age, namely by cryopreservation of oocytes or embryos. Physicians should inform all patients of reproductive age of their reduced fertility after the age of 35 and recommend not postponing pregnancy planning to late reproductive age or preserving fertility using cryopreservation techniques. Patients should be informed about the current possibilities of science to ensure the preservation of reproductive function through the use of cryotechnology and to allow them to make informed choices.
Other approaches have been aimed at improving the quality of oocytes and embryos obtained from women of late reproductive age. Among these technologies, the methods of mitochondrial replacement have been especially prominent as the main source of the ageing of female oocytes. These technologies are aimed at preserving the mother’s nuclear genotype to make possible the generation of, genetically, one’s own child in advanced reproductive age patients. Whilst these technologies are pushing the boundaries for manipulating female reproductive cells to achieve better outcomes in ART, the optimistic results of studies on gametogenesis reconstitution from somatic stem cells do not yet make it possible to implement them in clinical practice and require significant further research and validation. At the same time, the growing popularity of the use of PRP therapy to improve the reproductive hormonal background and activate folliculogenesis in women of older reproductive age requires further in-depth research and has good prospects for treatment.
Conflict of interests
The authors declare that there are no conflicts of interest.




