Introduction
Lower extremity amputation is defined as the complete loss in the transverse anatomical plane of any part of the lower limb and can be divided into major (above ankle, through knee, and up to hip amputations) and minor (foot and toes) amputations (Nather and Wong, Reference Nather and Wong2013; Ang et al., Reference Ang2017; Chan et al., Reference Chan2019). Diabetic lower extremity amputation (DLEA) is a major surgical procedure performed in patients with diabetes and generally disruptive to patients’ normal life and can have a profound and lasting impact on an individual’s physical and functional capacity and quality of life (Liu et al., Reference Liu2010; Holzer et al., Reference Holzer2014; Barg et al., Reference Barg2017; Silva et al., Reference Silva, Furtado, dos Santos, da Silva, Caldas, Bernardes and Ferraz2019). Amputation-related physical inabilities affect patients’ daily activities of living and their social roles and identities, which often leave them with a sense of dependency and powerlessness (Chini and Boemer, Reference Chini and Boemer2007; Sousa et al., Reference Sousa, Corredeira and Pereira2009; Livingstone et al., Reference Livingstone, Van De Mortel and Beverly2011; Senra et al., Reference Senra, Oliveira, Leal and Vieira2012; Foster and Lauver, Reference Foster and Lauver2014; Grech and Debono, Reference Grech and Debono2014; Washington and Williams, 2016). It is also common that patients experience emotional distress and require emotional support alongside the medical management of their DLEA (Horgan and MacLachlan, Reference Horgan and MacLachlan2004; Liu et al., Reference Liu2010; Senra et al., Reference Senra, Oliveira, Leal and Vieira2012; Dunne et al., Reference Dunne2014; Grech and Debono, Reference Grech and Debono2014; Delea et al., Reference Delea2015). In particular, major amputation is reported to compromise patients’ body image and their relationships with others (Coffey et al., Reference Coffey2009; Norlyk et al., Reference Norlyk, Martinsen and Kjaer-Petersen2013; Holzer et al., Reference Holzer2014; McDonald et al., Reference McDonald, Sharpe and Blaszczynski2014; Siersma et al., Reference Siersma, Thorsen, Holstein, Kars, Apelqvist, Jude, Piaggesi, Bakker, Edmonds, Jirkovská, Mauricio, Ragnarson Tennvall, Reike, Spraul, Uccioli, Urbancic, van Acker, van Baal and Schaper2014), while patients with minor amputation often require re-amputation due to wound-related complications, such as wound dehiscence and prolonged healing times (Pollard et al., Reference Pollard2006; Dudkiewicz et al., Reference Dudkiewicz2009; Kono and Muder, Reference Kono and Muder2012; Vogel et al., Reference Vogel, Petroski and Kruse2014; Chan et al., Reference Chan2019), which also affect the process of rehabilitation (Price et al., Reference Price, Moffatt and Crofts2015). Post-amputation wound healing is generally challenging in the first 12 months after amputation, as wound healing rate is only achieved in less than half of the whole amputee population (Chan et al., Reference Chan2019).
In Singapore, following a lower extremity amputation upon discharge from hospital to home, patients with post-amputation wounds are predominantly managed in the primary care setting by nurses who assist with patients’ transition to stability and normality. Effective wound care in primary care as part of continuity of care is therefore essential for patients’ recovery physically and psycho-socially. Several recent qualitative studies explored issues related to patients’ mobility and focussed on the perceptions of declined functionality and complicated prosthesis adjustment of people living with amputation (Norlyk et al., Reference Norlyk2016; Anderson et al., Reference Anderson2019; Batten et al., Reference Batten2019; Khan et al., Reference Khan2019). These aspects emphasise the challenge and complexity of the rehabilitation phase of major DLEA after wound healing. Many research studies have also explored rehabilitation of patients with major amputation (Chini and Boemer, Reference Chini and Boemer2007; Sousa et al., Reference Sousa, Corredeira and Pereira2009; Senra et al., Reference Senra, Oliveira, Leal and Vieira2012; Grech and Debono, Reference Grech and Debono2014; Silva et al., Reference Silva, Furtado, dos Santos, da Silva, Caldas, Bernardes and Ferraz2019). Little is known about the early stages of DLEA where patients may have to grapple with potential slow-healing post-amputation wounds and cope with physical and psychosocial stress. A meta-analysis revealed that almost one-third of transmetatarsal–minor amputations eventually result in one or more proximal re-amputations (Thorud et al., Reference Thorud, Jupiter, Lorenzana, Nguyen and Shibuya2016). However, few studies have focussed on trying to understand patients’ lived experiences with potential slow-healing post-amputation wounds after minor amputations.
A recent study found that the trends in major and minor DLEA are increasing in Singapore (Ang et al., Reference Ang2017). This remains a gap in research concerning the experience of patients living with both major and minor amputation shortly after their DLEA and prior to the post-amputation wound healing in primary healthcare. The purpose of this study is to give voice to patients’ insider perspectives on what they experience after both major and minor DLEA with a post-amputation wound in primary care and ultimately enable healthcare professionals to develop interventions to assist patients in physical healing and psychosocial recovery.
Concept of normality and DLEA
The concept of normality in relation to health and illness describes how individuals adjust to and accept their ability to live with an illness (Williams, Reference Williams2000). Normalisation is a cognitive and behavioural adaptation process which involves the use of coping techniques to minimise the impact of disease, enable the individual to engage in normal activities, and manifest a normal appearance to others (Knafl and Deatrick, Reference Knafl and Deatrick1986). O’Neal (Reference Neal2007) suggests that normalisation can be seen as an adaptive coping strategy in responding to chronic illness. DLEA is one of the most complex complications for patients with diabetes. The subsequent post-amputation wound healing is particularly challenging as patients with diabetes have compromised blood circulation and other underlying complications, which may have adverse effects on the healing process (Price et al., Reference Price, Moffatt and Crofts2015; Chan et al., Reference Chan2019). Given the complexity of DLEA and the natural of slow-wound healing, understanding amputee’s sense making of their illness, coping and normalising strategies will enlighten healthcare providers on better care delivery.
Methods
Design
This study employs a qualitative design adopting interpretative phenomenological analysis (IPA) approach. IPA is used to make sense of the participants’ lived world (Smith and Osborn, 2015) with a focus on examining how individuals make sense of their life experiences (Pietkiewicz and Smith, 2014). Studies using IPA are concerned with existential issues and are often related to major life-changing events, as in the case of the loss of a lower extremity (Smith, Reference Smith2004). IPA also acknowledges that everyone is influenced by the world in which we live in and the experiences we encounter. Therefore, IPA is an interpretative process between the researcher and participant, influenced predominantly by Heidegger’s interpretive phenomenology, hermeneutics, and idiography (Peat et al., Reference Peat, Rodriguez and Smith2019).
Setting and participants
The study was conducted in a regional primary healthcare setting in Singapore. Its six polyclinics serve a significant proportion of the population in the central and northern parts of Singapore and provide a comprehensive range of health services for the family, functioning as a one-stop health centre providing treatment, health promotion, and disease prevention (National Healthcare Group Polyclinics, no date).
Previous evidence found that a 12-month period after amputation is usually the crucial time-span during which emotional challenges typically surface (Fisher and Hanspal, Reference Fisher and Hanspal1998; Price and Fisher, Reference Price and Fisher2007) and one-fifth of patients with diabetes die within the first year of their amputation (Linette Lai, 2015). Hence, participants who had undergone at least one episode of major or minor amputation due to diabetes in the last 12 months and underwent post-amputation wound care in polyclinics were recruited for the study. Patients who are below 18 years old and with cognitive impairment and known mental illnesses were excluded from the study. Wound care nurses from the clinics screened and identified eligible patients.
Ethical considerations
The study was approved by the ethics board (Ref No. 2018/00424) of the researched institution. Wound care nurses from the respective clinics screened and identified eligible patients based on the study inclusion and exclusion criteria. A co-researcher (ECAL) cum interviewer was introduced to all eligible participants by wound care nurses. A copy of Participant Information Sheet was distributed to each individual potential participant for their consideration prior to participation. The same co-researcher then approached the willing participants and briefed them the aims of the study and answered their queries prior to obtaining the individual written consent. Participation of the study was completely voluntary for all participants. Collected audio interview data were de-identified and all transcripts were anonymised using unique identifiers to protect the privacy and confidentiality of the participants.
Data collection
Semi-structured interviews with a duration of 45–60 min each were undertaken and audio recorded. Field notes and reflexive diaries were also used to capture researchers’ observations and interpretations. Interviews were conducted in a quiet room when the patients came for their wound treatment. An interview guide was developed and refined to allow the interviewer to probe for specific areas of interest in participants’ experiences. Data were collected between September 2018 and January 2019.
Data analysis
The interviews were transcribed verbatim and analysed using IPA (Smith et al., 2009). We adopted a seven-step analysis framework comprising: reading and re-reading, initial note making, developing emergent themes, searching for connections across emergent themes, moving to the next case, looking for patterns across cases, and taking interpretations to deeper levels. Following this framework, each interview was read and re-read several times. Initial analyses involved all six authors identifying and taking descriptive notes of linguistic and conceptual units of meaning in the first three interviews. In keeping with IPA’s idiographic, phenomenological commitment (Smith et al. 2009), each interview in the current study was analysed individually in-depth by three main researchers. Emergent themes were derived from initial close reading and extensive note taking, as recommended by Smith et al. (2009). The three main researchers in the study team worked closely in order to establish consensus on their interpretations. The researchers moved iteratively between transcripts and initial notes, in order to identify emergent themes within the transcript. Doubts were cleared by discussions to achieve intersubjective agreement. Each interview’s emergent themes were collected and clustered into subordinate themes, which were then used to structure superordinate themes and relate them to the overarching theme which summarised the essence of the phenomenon under study. Interviews stopped after the nineth interview when data sufficiency was reached. Themes that appeared frequently or which had particular resonance for interviewees in terms of significantly reflecting important aspects of the lived experience were given more weightage.
Methodological rigor
Credibility was supported by the fact that several members of (ZX, GLJ, and DL) the research team were nursing professionals, and thus familiar with issues faced by patients’ post-DLEA discharge. Additionally, the primary researcher (ZX) is a wound care specialist with deep knowledge and practical experience in caring for patients with DLEA wound. Regular study team debriefings were conducted to improve the validity of the data analysis process. Confirmability was enhanced by contacting two participants for a validation exercise to receive their feedback on the accuracy of the identified themes. Dependability was achieved by having two expert qualitative researchers and two nursing researchers with experience in qualitative research review the transcribed material to validate the codes and descriptors identified. About one-quarter of the anonymised transcript data was also independently analysed by two other team members experienced in qualitative methods (BB and LM) to enhance dependability by validating the primary coders’ analysis and interpretations.
Findings
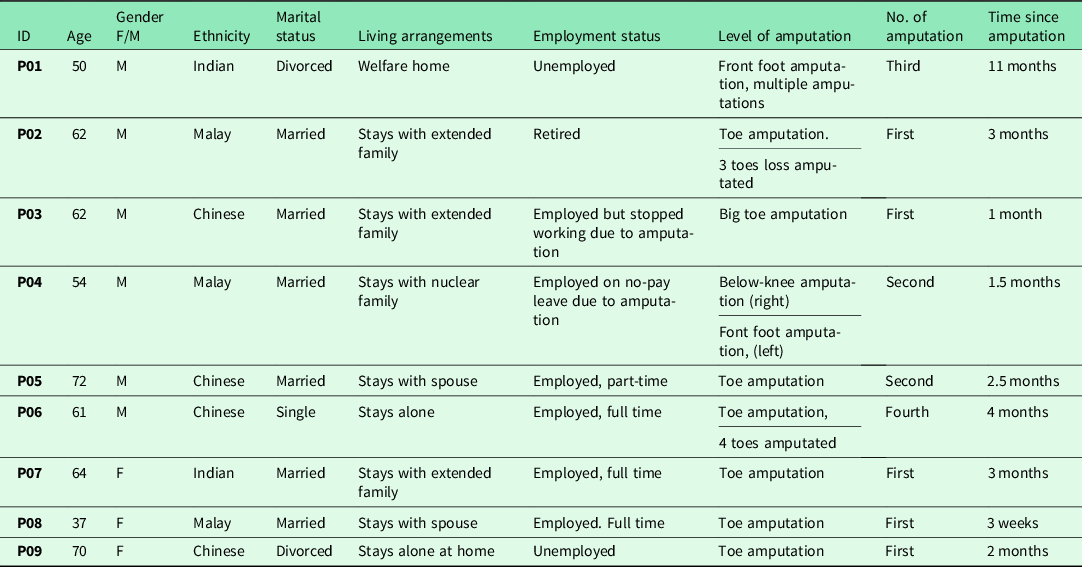
An overview of the characteristics of the nine participants can be seen in Appendix 1. Analysis of the data surfaced eight subordinate themes, which were grouped under three superordinate themes linked to one overarching concept. The essence of the phenomenon of ‘the lived experiences of patients with DLEA and wound’ can be described as ‘struggling for “normality”’ which encompasses the three domains of sense making: physical loss disrupted normality, emotional impact aggravated the disrupted normality, social challenges further provoked the disrupted normality, and attempt to regain normality (Figure 1). The emphasis was on the struggle to maintain a normal life by walking on one’s own feet and seeking to present a normal life to others, despite the complexity of DLEA and underlying disruption of wound healing.
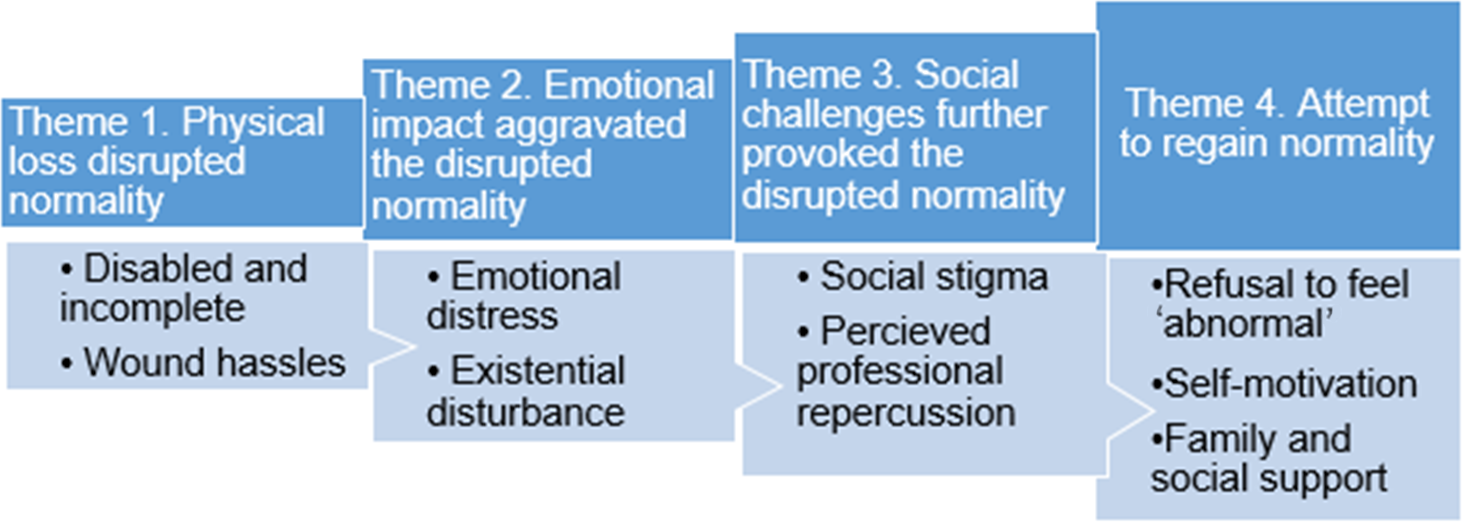
Figure 1. The essence of ‘struggling for normality’ embodies physical loss, emotional impact, social challenges, and attempt to regain normality
Theme 1. Physical loss disrupted normality
Disabled and incomplete
The physical disability caused by the amputation resulted in participants feeling disabled and incapacitated. A foot loss meant more than just a physical loss to them. Losses also included loss of independency, change of social roles, plans for the future, and the loss of identity as a walking person.
… they had taken away the whole foremost of my foot… I can’t drive, I can’t walk independently, I can’t run! I cannot be a soccer player and play soccer anymore! …(P01)
Losing part of one’s leg or foot also resulted in a sense of incompleteness, confusion, and bewilderment which further intensified the experience incapacity. A sense of incompleteness, incapacity, and disability deriving from the absence of the lower extremity hindered participants’ daily life and activities and made them feel a loss of identity and the loss of ability to perform familial and social roles, thus disrupted their normality.
… I’m searching—middle of the night I’m searching for my leg…? Where’s the rest of my foot?… I am incomplete… How am I going to survive? How am I going to work? Because – I can’t walk anymore, I’ve to sit on a wheelchair… Not being able to play my role, as a father, as a husband….As a… breadwinner. (P04)
Wound hassles
The physical wound was a factor affecting walking and wearing a prosthesis and an obstacle to maintain a normal life. Severe restriction of movement, confinement, and inconvenience were blamed on the hassles of wound care by most of participants. A lot of mental energy was invested in trying not to get the wound wet while showering and taking care of it as instructed.
… It is very troublesome when I am showering! I have to wrap the foot and make sure it does not get wet… … It bothers me a lot… (P06)
… I am confined (looked at amputation wound) … so I can only move about in my house… Obviously my world only consists of my room… So I look forward for my visits to the clinics for treatment to heal the wound, because it’s kind of a place where I visit the world… (P08)
The impact of the physical wound was associated with fear of pain and potentially causing further injury to the wound. This led to an apprehension of touching and moving the affected lower extremity. The amputation wound became a threat to well-being, which resulted in a lack of physical mobility and compromised normality.
… I am afraid to put too much pressure on it and injury the wound… scared of hurting. If I step too strongly here, the sole and the wound area will hurt. … It’s very painful… (P09)
Despite having an amputation wound with partial foot removed, a participant’s rejection of a wheelchair to move around showed a strong sense of the desire to maintain self-identity and normality.
… I am not a wheelchair man! I will never be a “wheelchair man” or a “bed man” for life… I can still walk with heel… (P01)
Theme 2. Emotional impact aggravated the disrupted normality
Emotional distress
Lower extremity loss and wound also resulted in emotional vulnerability and existential uncertainty. More than half of the participants expressed anxiety and fear of further amputations as lack of control over their wound healing and future health. In extreme cases, this bordered on despair, giving in to the threat and awareness of imminent death if another amputation had to be undertaken. Those feelings were sometimes overwhelming and generated emotional distress and depression leading to thoughts of suicide which disrupted the process of normalisation.
… very depressed… very depressed… … how I wish I can just take something and don’t have to wake up…(P04)
… very depressed… …if wound does not heal, very scared and worried they (doctors) will cut higher and higher…if it really happens, then… everything I will give up, pass it off, I don’t want to stay anymore! (P06)
The anxiety of the slow-healing of the existing wound further aggravated the disrupted normality. The fear of provoking further amputations invoked uncertainty, worsened self-confinement mentality, and threatened normalisation.
The healing… can take anything up to six months or even more. So, that is the part that worries me the most… And then for this period of time, I have to sit back and practically do nothing, and wait for the wound to heal. It’s a hassle, but I have to accept it… and hopefully it heals. But if there is further (wound infection) …. the foot may have to go… (sigh) (P03)
Existential disturbance
Losing a leg caused an existential disruption which restricted patients’ lifestyles and changed their views of the world dramatically. One participant underwent a below-knee amputation and was severely disoriented when he reached home after discharge from hospital. Confusion and loss of independency exacerbated his existential disruption.
… It takes me about couple of hours just to realize that I am at home… I have to depend on my wife to move me around to toilet with the wheelchair because I need to be transferred from wheelchair to the toilet seat… (P04)
In some cases of foot amputations, participants’ felt an existential uselessness and hopelessness related to their inability to maintain their normality and social identity.
You find yourself quite useless and not being able to do things. That life is not exciting anymore. There’s no challenge ahead of you because your abilities are limited, especially to earn money to work and to make yourself useful. … (P03).
By contrast, in cases of major amputation, the new possibilities of walking again opened up by the prosthesis began a process of self-development to have an identity and regain normality.
When I see a guy older than me, who just got his prosthetic leg, and I see how fast he walks… When will it be my turn? I’m looking forward to have my prosthetic leg… (P04)
Theme 3. Social challenges further provoked the disrupted normality
Social stigma
Facing the reality of being labelled as an ‘abnormal’ was hard for participants. Unsupportive social networks restricted their social life, instigated self-isolation, and triggered anger. Their anger and reluctance to think about amputation and their wound can be illustrated as social withdrawal, which further provoked the disrupted normality.
I have not been meeting a lot of people. You know people’s mouth; you cannot stop them from asking you questions about your amputation … I’m tired of answering questions from people, like what happened? … I wanted to tell them to their face, “shut up, stop asking me questions! I’m done already, I don’t want to think about this… (deep inhales) … I do not want to answer the stupid questions! … (P08)
A participant expressed fear that his amputation may attract people’s attention and how this affected his social engagement.
…not possible to go out… people look at me that I’m—an—alien… because I’m wearing shorts, with the (stump) everything half of it, so… they look at me like “an alien” …… (P04)
Perceived professional repercussion and financial burden
Participants were also concerned about financial survival because they were unable to cope with the financial burden of medical treatment, including transport fees for wound treatment and wound care expenses.
… But the other stress is, financially, how am I going to cope with it? … (all these) drained me off financially… and…I do not know whether I am able to cope up with it… (P03)
Job insecurity and uncertainty were highlighted by one participant who had undergone below-knee amputation. The amputation deprived him of his ability to walk and cut short his career path. The consequences of the amputation on his work life and professional identity had severe impact on his self-esteem.
So but if I get back to work, it’s going to be a change at my work because I am an amputee … unfortunately, long service doesn’t count… (P04)
Theme 4. Attempt to regain normality
Refusal to feel ‘abnormal’
In order to present a ‘normal self’ to others and avoid social stigma, amputees decided to act as a ‘normal’ person by hiding visible signs of partial foot loss with wound, for instance by using covered shoes. Acting as a ‘normal’ person was a personal drive to regain her self-identity.
… but I need to buy a pair of covered shoes to cover my ugly foot with the missing toe, then there’s nothing abnormal … (P09)
A participant who underwent partial foot amputation with two wounds on the foot insisted to walk without walking aid and claimed that ‘everything is normal’. The refusal of being ‘abnormal’ and insisting of walking on her own feet reflected the desire to regain normality.
…No, I have to train myself without that (walking frame)… I said I can walk! Everything is normal… (P07)
Self-motivation
Despite the complexity of wound healing, a few participants made conscious efforts to accept the inevitability of the amputation by maintaining old hobbies and making plans. Those participants made efforts to stay motivated by having plans and hope for visualising the future for normal life.
Once my wound is closed, I will put on back my bowling shoe and start to bowl again. Even though I won’t bowl like before, but I want to – I still want to bowl… (P08)
A participant with multiple comorbidities and wound complications talked about his future plans and goals during interview. Self-reliance and determination to not be bound by physical limitations were expressed in his positive self-talk. Although healing seemed impossible, he struggled to cope with his medical conditions and looked forward to regain normality.
… (Self-talk) Think positive, be positive, you’ll go far than what you think you can’t! … I told myself, there are more things you can do … you got hands, you still got your body … I got more things to do. I got more places to go in life. I still got the business in my mind … (P01)
Family and social support
The changed family role caused by amputation did however threaten participant’s social self-identity. Despite high levels of dependency after discharge from the hospital, unconditional family care motivated one participant to look forward and reaffirmed his family role as the ‘same father’ while back home. Family members safeguarded participants’ physical and psychological well-being and played multiple roles in an attempt to facilitate their transition back to independence and regain normality.
Kids tried to accommodate to me to what I need. “… you’re still the same father. Minus one leg or what, you’re still the same father (weeping)…” … I am blessed that I have strong support from my wife, children, and siblings…friends… so I have to look forward… (intake of breath) …food-wise, they do … control it… They are my dietitian; they are my disciplinarian… (P04)
With perceived social stigma in mind, instead of withdrawing from social life, some participants were interested in exploring a moral support group to facilitate normalisation and recovery.
… we need the moral support where there’s a group you can talk, you can cry… among one another… at least we are prepared to face what are the problems, what are the emotional things that we will go through… (P04)
Discussion
Struggling for wound healing and normality
This study explores how patients with DLEA and post-amputation wound making sense of their lived experience after discharge from acute hospitals to home during recovery and wound healing period. This study illustrates that both minor and major amputations are a life-disrupting event, with implications beyond the loss of a body part, and require re-conceptualising the self. Our findings demonstrate that amputation-related physical loss, emotional impact, and social challenges threatened participants’ self-identity and disrupted their perceptions of normal life, and our participants struggled to regain normality throughout the recovery journey. These are in line with findings from previous studies that amputation particularly major amputation-related physical impairments bring challenges to patients’ self-identity and amputees’ expected return to normality (Hamill et al., Reference Hamill, Carson and Dorahy2010; Senra et al., Reference Senra, Oliveira, Leal and Vieira2012; Ostler et al., Reference Ostler, Ellis-Hill and Donovan-Hall2014). In particular, prosthesis gave them a sense of normality and made their hope of walking again a real possibility (Norlyk et al., Reference Norlyk2016) and the expectation of returning normality appeared to be an important coping mechanism (Ostler et al., Reference Ostler, Ellis-Hill and Donovan-Hall2014). These have been also described by a participant with below-knee amputation in the present study who was extremely depressive immediately after amputation until he found prosthesis as his hope and new possibility to walk again as he expressed that ‘I’ m looking forward to have my prosthetic leg’.
In the present study, we also found that most of our participants with minor amputation remained hopeful for the future, expecting to walk on their own feet even though all of them described a strong sense of anxiety and struggling with uncertainty of wound healing. Anxieties about their challenges of complete wound healing were balanced against the hope of returning to being a ‘normal’ person and regaining control of their lives. The dynamic between hope for wound healing and fear of wound breakdown further revealed the reality of their struggles for normality. Many also struggled with the frustrations of wound hassles and a prolonged healing process. The refusal to feel ‘abnormal’ and the self-motivation to cope with challenges related to DLEA and the post-amputation wound reinforced their perceptions of struggling to maintain normality. Most of them expressed that wound healing took precedence over any other social plans and hindered their social adaptation and delayed normalisation. These findings provide important additional insight into the existing knowledge on the experience of patients with minor amputation, while also posing new challenges to healthcare professionals in primary healthcare pertaining to post-amputation wound care.
Uncertainty of wound healing as a threat to the disrupted normality
Healing of post-amputation wound is challenging and the healing time following minor amputations can take up to five months (Fortington et al., Reference Fortington2013), with more than one in five of minor amputations progressing to major amputation one year after the first amputation (Chan et al., Reference Chan2019). In the present study, all participants expressed the fear of wound deterioration and concern about possible further amputations during the interviews. Most participants expressed that wound-related physical restrictions and dependency on others worsened their emotional distress and existential disturbance. Furthermore, high costs of wound treatment, complexity of wound care, and uncertain prognosis of healing added stress to patients and their families. Most of the participants also expressed that the post-amputation wound further confined their movement as they had to restrict weight-bearing activities including walking and had to wear customised treatment shoes for the purpose of foot wound healing. This reflects the likelihood that situations of body image disturbance exacerbated the challenges of fighting to maintain normality. And the situation could result in moving into a totally disrupted normality if severe wound complications develop and further amputation occurs. Given that the threat to the disrupted normality arises from episodes of wound complications and the possibility of re-amputation, there is an urgent need to shift wound care towards a more holistic pathway where both physical healing and psychosocial recovery should be the focus of the patient care. The finding calls for a new care model to support those people who live with DLEA with post-amputation wound.
Attempting to regain normality through self-motivation
Despite being confronted with the challenges of DLEA and possible complications to wound healing, our participants struggled to regain normality by actively exploring adjustment strategies and accommodating themselves to more realistic expectations, as a way to self-motivate and foster positive outcomes. This finding is in line with the findings from previous studies (Murray, Reference Murray2010; Norlyk et al., Reference Norlyk, Martinsen and Kjaer-Petersen2013; Dunne et al., Reference Dunne2014) that the hope of re-conquering or seeking to pursue former interests and goals was a way to establish a feeling of normality. For instance, one participant with toe amputation shared that she could not wait to put on her bowling shoes and resume her routine bowling activity ‘even though I won’ t bowl like before’. The goal of regaining normality is epitomised in hope for wound closure and regaining the ability to walk. This finding has been described by participants in previous studies (Gallagher and MacLachlan, Reference Gallagher and MacLachlan2004; Murray, Reference Murray2010; Ostler et al., Reference Ostler, Ellis-Hill and Donovan-Hall2014; Littman et al., Reference Littman, Erin and Haselkorn2017; Batten et al., Reference Batten2019) where participants sought to live a ‘normal life’ and expected to be able to walk and return to many of the activities that they had previously carried out, as a sign that they were able to regain normality.
However, some participants shared that their foot post-amputation wound interfered with their physical functional performance. Moreover, they had to ‘sit and practically do nothing’ until complete wound healing because they perceived that physical activity could hinder wound healing. This passivity also reflected their unwillingness and low confidence level in performing self-care and the perceived low knowledge level in how to live well with the amputation and the post-amputation wound. Hall et al. (Hall et al., Reference Hall2005) found that individuals’ ability to self-manage and make adjustments to the physical and psychosocial changes that occurred may influence how easily they could regain a sense of normality. Hence, the findings indicate a need for patient education programs to enhance self-motivation and self-care behaviours for optimal wound care and underlying disease management.
The role of family support to regain normality
For most of our participants, family members were their primary companions who journeyed alongside them in their recovery process. Upon discharge from hospital to home, one participant expressed feelings of anxiety, disorientation, and even de-familiarisation of his own home. Previous work (Sjödahl et al., 2004; Washington and Williams, 2016) has also found that the transition from hospital to home sometimes is difficult for patients as the reality of their new ‘self’ in terms of their physical inabilities becomes more apparent as they return to their home. During this phase, the participants in the current study also struggled to take control of their lives and assimilate the full impact of the lower extremity loss. However, they received unconditional care from their family members to help them cope with their physical trauma and emotional distress. The participants often also described that family members were pillars of strength to motivate and encourage them to move forward. Kim and Han found that perceived family support is the main factor affecting self-care for patients with diabetic foot wounds (Kim and Han, Reference Kim and Han2020). How far patients can go for recovery depends on their own motivation and social support from family caregivers (Road to Recovery, 2016). Hence, in the phase of post-amputation home recovery, family members should be encouraged to continue to perform their multiple roles as a ‘dietitian’ and ‘disciplinarian’ to support patients in coping with their life challenges. In addition, we suggest engaging family members in participating in patient care programmes to facilitate patients’ ongoing physical and psychosocial adjustment.
Social awareness and support to regain normality
Many studies have explored body image disturbance (Senra et al., Reference Senra, Oliveira, Leal and Vieira2012; Norlyk et al., Reference Norlyk, Martinsen and Kjaer-Petersen2013; McDonald et al., Reference McDonald, Sharpe and Blaszczynski2014; Norlyk et al., Reference Norlyk2016; Khan et al., Reference Khan2019) and changed self-identify for patients who have undergone major amputations. In the present study, we found that body image and anxiety was a concern for the participants with both major and minor amputation. Participants with toe amputation opted for concealing their bulgy dressing and incomplete foot with covered shoes to make them feel ‘normal’ and avoid social abandonment. Some participants also expressed feeling of perceived ‘abnormality’, social stigma, and social exclusion which further contributed to social withdrawal and challenged their attempt to regain normality. This finding resonates with previous literature that individuals with amputation often internalise aspects of social stigma relating to feelings of shame and embarrassment about their perceived ‘abnormality’ (Rybarczyk et al., 2000) which affected their social identity(Chini and Boemer, Reference Chini and Boemer2007; Sousa et al., Reference Sousa, Corredeira and Pereira2009; Livingstone et al., Reference Livingstone, Van De Mortel and Beverly2011; Senra et al., Reference Senra, Oliveira, Leal and Vieira2012; Foster and Lauver, Reference Foster and Lauver2014; Grech and Debono, Reference Grech and Debono2014; Washington and Williams, 2016). Participants in the present study voiced that social support, in particular, cultivating social awareness, was essential to enable them to live with DLEA and return to normality. In this context, amputee support groups or community outreach programmes could be considered for patients with DLEA to promote their reintegration in social life and regain normality.
Apart from social stigma, the participants also expressed job insecurity caused by physical limitations which could potentially result in loss of income. In Singapore, although the government subsidises up to 80% of the total cost of care provided in public hospitals and primary care polyclinics (Roosa et al., Reference Roosa, Robin, Elias, Ana and George2020), some of our participants could not afford the high costs of co-payment for medical bills related to the complexity of amputation care. These financial concerns resulted in added stress during recovery. This finding urges practitioners to work closely with social sectors to assist patients in restoring their social relations.
Implications for Clinical Practice
We agree with the findings from the previous study (Barg et al., Reference Barg2017) that the overall post-amputation responses were generally similar among participants with a DLEA regardless of level of amputation. Our findings further revealed that patients living with both major and minor DLEA were struggling to physically and psychosocially adjust to renegotiate self-identity and regain normality. Hall et al. (Hall et al., Reference Hall2005) found that the strategies to maintain normality are associated with psychological, behavioural, social, and medical aspects. Therefore, we propose an interdisciplinary team care model (Figure 2) which echoes and builds upon the current literature (Butcher and Corbett, Reference Butcher and Corbett2014; Hingorani et al., Reference Hingorani2016; Khan et al., Reference Khan2018) and our findings to address amputees’ physical and psychosocial needs to support them through the crucial post-DLEA transition period and facilitate possibilities for normalisation. In a primary care setting, the composition of interdisciplinary team can include physicians, nurses, psychologists, podiatrists, medical social workers, and family members to assist DLEA patients with wound healing, underlying disease management, as well as in need of psychosocial adjustments to regain normality. Our model focusses on normalisation based on the concept of a team approach and addresses recovery as a whole, where clinicians assist with physical healing, while psychologists, medical social workers, and family members provide support to psychosocial adjustment improve the care process from amputation to ambulation as normal person.
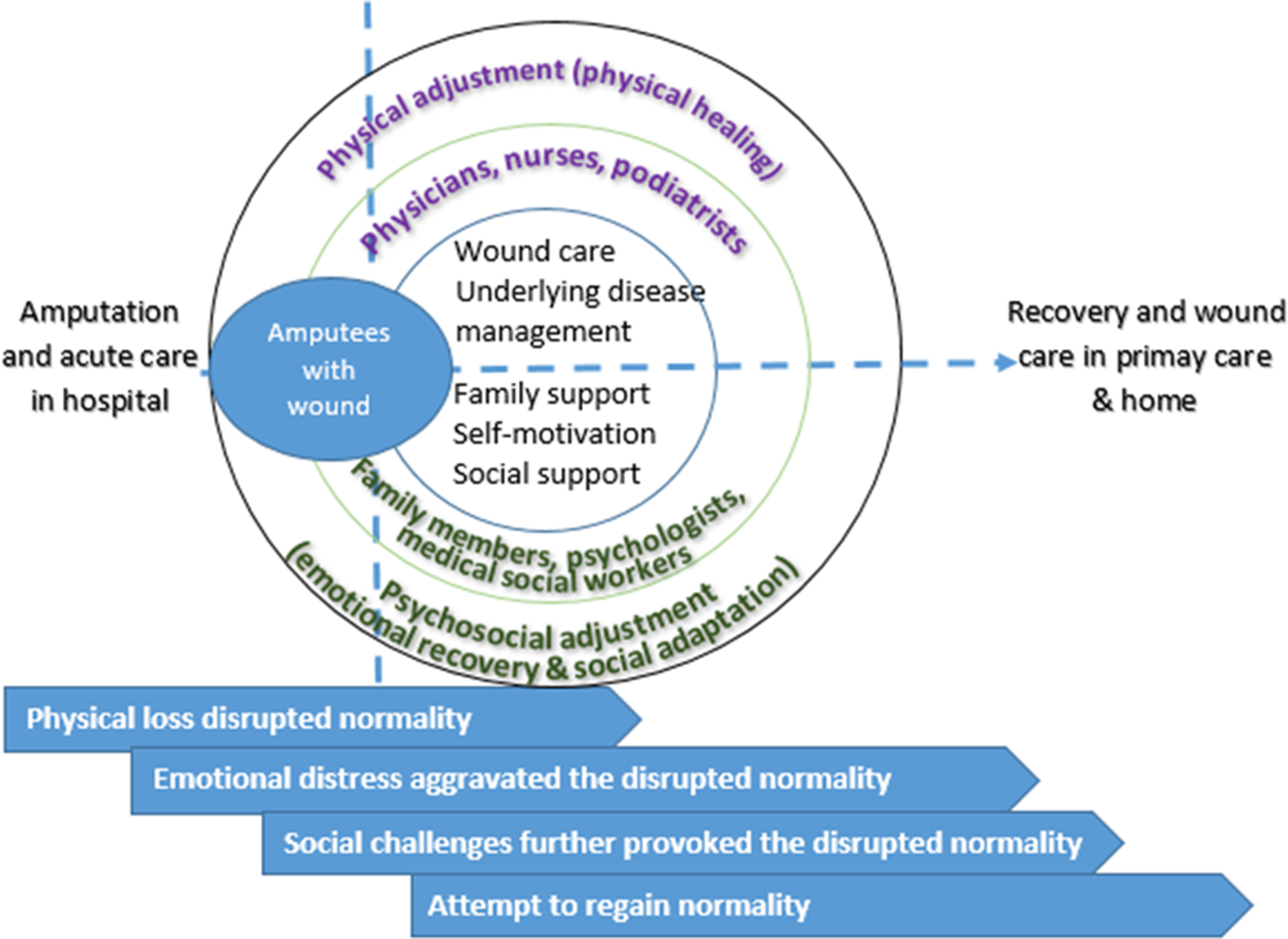
Figure 2. Interdisciplinary care model for physical and psychosocial adjustment and normalisation for patients with DLEA and post-amputation wound in primary healthcare
Limitations
In the present study, we had a selection bias as males between the age of 50 and 72 years made up most of the sample. However, this reflects the population of the diabetic amputees in Singapore (Ang et al., Reference Ang2017). Our study was also carried out at a particular time point. Hence future longitudinal studies could enrich our findings by exploring the trajectory of patients’ experience by interviewing them at different time points post-amputation, or across subsequent amputations. Future studies should also consider the experiences of female amputees.
Conclusion
The study highlights the complex physical and psychosocial transition back to normality that patients face after DLEA and before post-amputation wound closure. Patients with both major and minor amputation and post-amputation wound may benefit from the interdisciplinary team care model for physical and psychosocial adjustment, more rapid wound healing, higher coping efficacy, and higher levels of social adaptability to regain normality. Healthcare professionals in primary care can consider the proposed interdisciplinary team care model to aid patients living with DLEA and post-amputation wound to adapt to their adjusted multiple social roles and regain normality.
Acknowledgements
The authors thank Lee Kong Chian School of Medicine, Nanyang Technological University Singapore and National Healthcare Group Polyclinics (NHGP) Singapore for the joint Centre for Primary Healthcare Research and Innovation grant. The authors wish to express their gratitude to NHGP Nursing Services and NHGP Clinical Research Unit for the support. Special thanks to Dr Gloria Law who was the Research Fellow at Family Medicine and Primary Care, Lee Kong Chian School of Medicine, Nanyang Technological University Singapore for her guidance in grant proposal writing. Special thanks to Miss Maja Magdalena Olsson who is a PhD student of Queensland University of Technology, Australia for her help with proofreading the manuscript. The authors’ heartfelt appreciation to all participants in this study for sharing their time and experiences.
Funding information
This study was funded by research grant (Ref No. 002) under the Centre for Primary Health Care Research and Innovation, a partnership between the Lee Kong Chian School of Medicine, Nanyang Technological University Singapore and the National Healthcare Group Singapore.
Conflict of interest
The authors declare that there is no conflict of interest.
Author contributions
Study design, data analysis and manuscript preparation: Z.X.; study design and data analysis: GLJ; data collection and data analysis: ECAL; study design: DL; data verification, revision and approval of the final manuscript: all authors
Appendix 1. Participant’s characteristics