The early phase of psychotic illness is a ‘critical period’, with major implications for secondary prevention of the impairments and disabilities that accompany psychosis. Timely and effective intervention during the first psychotic episode can alter the subsequent course of the illness (Reference Birchwood, Todd and JacksonBirchwood et al, 1998). Traditionally, patients who are acutely psychotic have been treated in in-patient units. This can be associated with marked anxiety, not only resulting from psychotic experiences but also from the circumstances of admission and early treatment (Hammill et al, 1989), which can be extremely traumatic (Reference Mcgorry, Chanen and MccarthyMcGorry et al, 1991). Hospitalisation may also predispose individuals to disability by promoting the loss of independence and skills, thereby making a return to work increasingly difficult (Reference Stein and TestStein & Test, 1980).
There is clear evidence that significant numbers of people with a range of acute psychiatric problems, whose care has traditionally been provided in hospital, can be treated successfully in their own homes (Reference Minghella, Ford and FreemanMinghella et al, 1998; Reference Bracken and CohenBracken & Cohen, 1999; Reference Brimblecombe and O'SUllivanBrimblecombe & O'Sullivan, 1999; Reference Harrison, Poynton and MarshallHarrison et al, 1999). Home-based treatment can help individuals and their carers by providing care within a free and familiar environment and it has the potential to facilitate a rapid return to normal lifestyle and function.
The NHS Plan (Department of Health, 2000) states a need for the development of ‘crisis resolution’ teams across the country, offering intensive home treatment as an alternative to admission. While some areas will have specific early intervention in psychosis services, the majority of acutely ill individuals with first-episode psychosis are more likely to have initial contact with a crisis resolution team. We present a brief study of service outcome for individuals who presented to a service that provides rapid assessment and intensive home treatment to patients with acute mental illness. Our aim was to assess the proportion of such individuals with first-episode psychosis who can successfully be treated at home and identify factors associated with the success of this arrangement.
Structure of the service
In north-west Hertfordshire, two community treatment teams provide rapid assessment and intensive home treatment as an alternative to hospital admission. During treatment, home visits may take place several times a day. The teams prescribe and provide medication and monitor compliance; offer emotional support and practical advice to both patients and carers; and provide assistance with the activities of daily living. Cover is provided from 09.00 to 21.00, 7 days a week. Each team comprises eight nursing staff, a Senior House Officer (SHO)/staff-grade doctor and sessions from a consultant psychiatrist and specialist registrar. An on-call rota of junior doctors provides cover in the evenings and at weekends.
Referrals are accepted for assessment if, based on the information received, the person appears to be suffering from an acute mental illness that is potentially severe enough to warrant hospital admission. Assessments considered to be urgent can be carried out within 2 hours of referral.
Method
Assessments during an 18-month period (1 January 1998 to 30 June 1999) were screened for patients presenting with first-episode psychotic illness. Psychotic illnesses of all types, including drug-induced psychosis, were included. The analysis excluded those under the age of 16, those with dementia and patients with a past history of psychosis. Where assessments confirmed that the individual's presentation potentially warranted hospital admission, patients were routinely offered home-based treatment by the community treatment team, unless there were clear reasons necessitating admission. In every case, data were collected concerning: demographics, mode of referral, current living situation, employment status, past history of self-harm and violence. Psychopathology on initial assessment was measured using the Brief Psychiatric Rating Scale (BPRS) (Reference Overall and GorhamOverall & Gorham, 1962) and diagnosis made according to ICD—10 criteria (World Health Organization, 1992).
Those who received home-based treatment were followed up until their symptoms decreased to a level where other services, such as community mental health teams and out-patient clinics, were able to provide appropriate care. Extended handover periods were common to ensure continuity of care. If a patient required in-patient admission, either at initial assessment or subsequently during home treatment, the most important reason for admission was noted.
For the purpose of analysis, the sample was divided into two groups. The first consisted of those who required hospital admission at any stage and the second of those who were managed by the team and successfully completed home-based treatment. A t-test was used to compare BPRS total scores, ‘thinking disorder’ sub-scale scores and age in the two groups. All other variables were compared using Fisher's exact test. All analyses were carried out using SPSS 8.0 for Windows.
Results
Forty patients were identified who met the criteria for first-episode psychosis. Their age ranged from 19 to 93 years (median 36 years). Twenty-three (58%) were male and 17 (42%) were female. Twenty-one (53%) referrals were directly from general practitioners (GPs), 11 (28%) from psychiatric services, and the remainder came from a variety of other sources, including families and self-referrals. Twenty (50%) of the initial assessments were carried out in patients' homes, eight (20%) in community mental health centres, seven (18%) at local psychiatric units and the remainder either in police stations or accident and emergency departments.
Following initial assessment, eight (20%) patients were admitted directly to hospital; three (8%) did not require input from the community treatment team as their condition did not appear to be severe enough potentially to warrant admission to hospital, and thus did not meet the criteria for community treatment either. These were followed up in psychiatric out-patient clinics and are not included in the study. Twenty-nine (73%) individuals were taken on for home treatment by the team. Of those starting home treatment, nine (31%) subsequently required hospital admission. The mean duration of stay with the team for those subsequently admitted was 11.5 days (range 1-90 days). Fig. 1 shows the service outcomes of the patients.
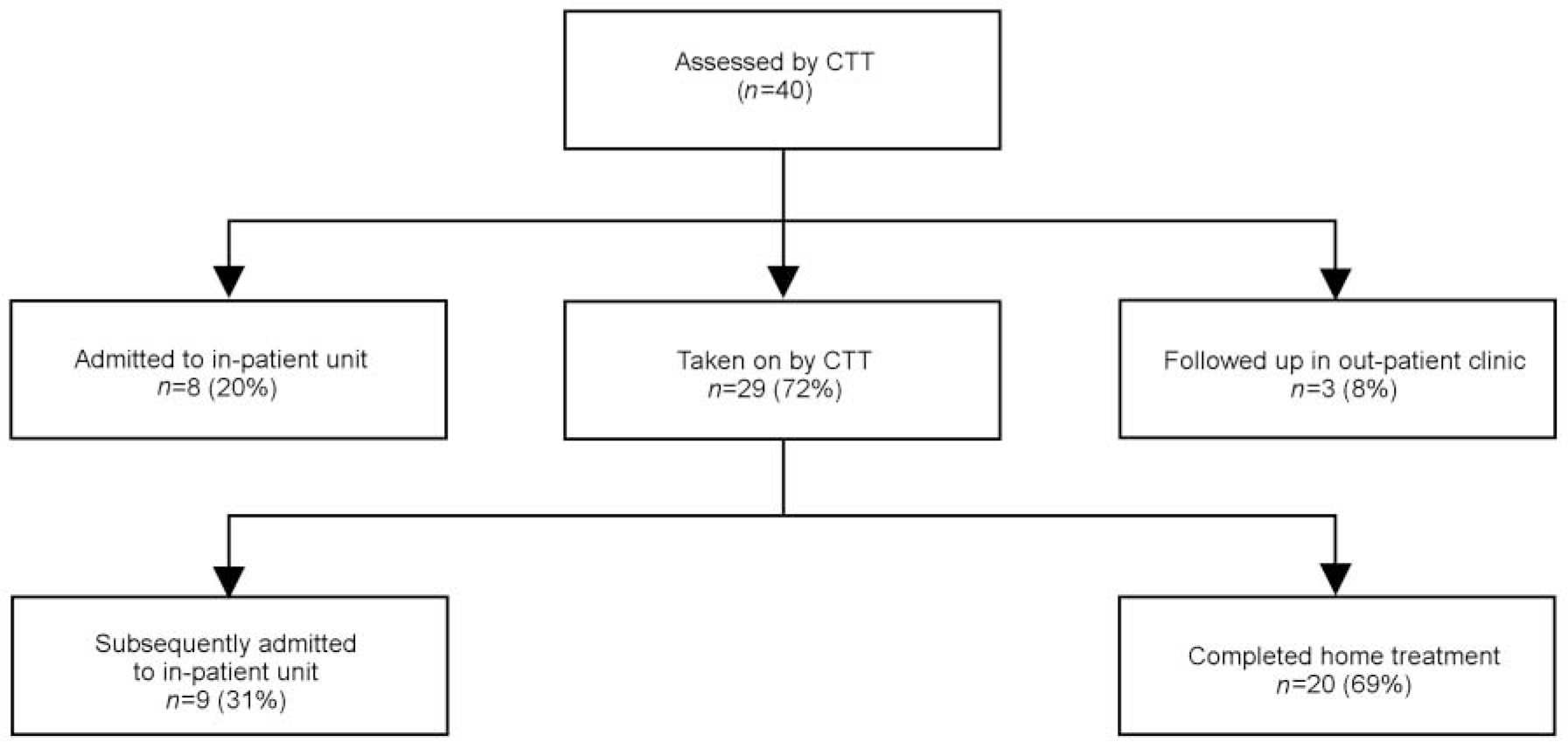
Fig. 1. Service outcomes (CTT=community treatment team).
Patients who required admission at any stage were compared with those who were successfully treated at home by a community treatment team. No significant difference was found between the two groups for any variable (Table 1).
Table 1. Hospitalised versus non-hospitalised patients by variable
| Variables | Admitted (%) | Never admitted (%) | Significance |
|---|---|---|---|
| Number | 17 | 20 | |
| Gender | |||
| Male | 9 (53) | 11 (55) | NS |
| Female | 8 (47) | 9 (45) | NS |
| Not employed | 8 (47) | 14 (70) | NS |
| Living alone | 5 (29) | 7 (35) | NS |
| Previous history | |||
| Violence | 4 (24) | 5 (25) | NS |
| Self-harm | 2 (12) | 2 (10) | NS |
| Brief Psychiatric Rating Scale total (mean) | 21 | 20 | NS |
| Thinking disorder (mean) | 7 | 5 | NS |
| Diagnosis | |||
| Schizophrenic type | 11 (65) | 10 (50) | NS |
| Mood disorders | 5 (29) | 10 (50) | NS |
| Organic disorders | 1 (6) |
Median duration of stay in hospital for patients who required admission was 31 days (range 3-118 days), compared with 47 days in home treatment (range 7-190 days) for those successfully managed at home. Of the 20 patients who were successfully managed at home, two required hospitalisation within 90 days of discharge from community treatment team follow-up. The remaining 18 (90%) did not require re-referral to the team or hospitalisation within the same period.
The reasons for admission recorded for the eight patients admitted at initial assessment were risk to self (either related to suicidal intent or dangerous behaviour such as wandering late at night) in five cases (63%) and, in one case each: not agreeing to accept treatment, carers unable to cope and patient's preference for hospital. Of the nine patients who were subsequently admitted from home treatment, the recorded reasons were: risk to self (n=3), risk to others through violence or fire-raising (n=3) and poor compliance with treatment (n=2). In one case, the reason for admission was not clearly documented.
Discussion
The study is somewhat limited by a relatively small sample size. However, its findings do tentatively suggest that over half of first-episode psychosis cases, presenting to a crisis resolution service in a manner that may potentially require immediate hospitalisation, may be managed successfully at home. This finding is similar to that established by a similar service in Australia (Reference Fitzgerald and KulkarniFitzgerald & Kulkarni, 1998). With the massive increase in home treatment/crisis resolution services being planned, these findings have considerable implications for the care of this very needy group. There are also obvious implications for in-patient areas, who may find a marked change in the mix of problems they encounter (Reference Harrison, Poynton and MarshallHarrison et al, 1999).
None of the variables measured in this study predicted an increased likelihood of failure of home treatment. Unlike some other studies (Reference Brimblecombe and O'SUllivanBrimblecombe & O'Sullivan, 1999; Reference Harrison, Alam and MarshallHarrison et al, 2001), there was no difference in outcome between diagnostic categories, although this may partially relate to the broadness of the categories applied, for example ‘mood disorders’. Also, there was no statistical difference in initial BPRS scores between the two groups, which is similar to the results of an Australian study (Reference Fitzgerald and KulkarniFitzgerald & Kulkarni, 1998). The reasons for hospital admission identified by the community treatment teams did not simply relate to severity of psychopathology or diagnosis, but were factors such as risk to self or others or poor compliance with treatment.
There is a range of factors that appears to contribute to a service's ability to successfully provide home treatment to this client group. The basic availability of an extended-hour service, providing frequent visits, is usually perceived by both patients and carers to be very supportive (Reference CohenCohen, 1999). The home treatment/crisis resolution team itself must have a specific role in the assessment of all possible referrals for hospital admission. This is important as other professionals, who are not experienced in providing intensive home treatment, may tend to admit to hospital rather than consider community-based treatment as a practicable alternative. The availability of medical staff to review medication, in terms of titrating dosage and responding rapidly to side-effects, appears to play an important role in increasing compliance and thus the likelihood of treatment being successful. The community treatment teams typically prescribe atypical anti-psychotic medication in an attempt to reduce rejection of treatment as a result of side-effects. Practical advice and help, concerning issues such as benefits and housing, are also important components in providing comprehensive care, as such practical support is often particularly valued by home-treatment patients (Reference GodfreyGodfrey, 1996). Good links with other services are important in ensuring continuity of care for patients.
As the use of alternatives to hospitalisation spreads across the UK, further research is required into the identification of which characteristics of individuals will predict a need for hospitalisation rather than home treatment. However, the results reported here suggest that resolving this issue will be difficult.
Declaration of interest
None.





eLetters
No eLetters have been published for this article.