Dural venous sinuses are valveless venous channels layered between the endosteal and meningeal layers of the brain which allow bidirectional blood flow from and into intracranial veins. Reference Kiliç and Akakin1 Together they form the main drainage pathway from the brain into the internal jugular veins. Major dural venous sinuses include the superior and inferior sagittal sinuses, the straight, transverse, sigmoid, occipital, cavernous, intercavernous, superior and inferior petrosal, sphenoparietal, and marginal sinuses as well as the basilar plexus. The dural venous sinuses possess complex anatomy and marked variability. Reference Standring2 Typically, the right transverse sinus is larger than the left, with each receiving blood from the lateral temporal and basal surfaces of the temporal and occipital lobes, extending to the posterolateral aspect of the petrous temporal bone to subsequently drain into bilateral sigmoid sinuses. Reference Standring2
At the age of 4 ½ fetal months, the transverse sinuses begin to enlarge over a period of 6 to 10 weeks until the sixth or seventh month of gestation. The size of the transverse sinuses then decrease slightly after birth and attains their adult size at approximately 1 year of age. Reference Okudera, Huang and Ohta3 Rapid increases and decreases in the inner diameter of the transverse sinuses at the time of ballooning from the fourth to seventh month of gestation can lead to anatomical variations including the absence of parts of the sinus or the formation of septa or fenestrations. Reference Okudera, Huang and Ohta3 In this short report, we discuss these variations of the transverse sinus and report an unusual case of fenestration.
During the work-up of a 45-year-old female presenting with left-sided binocular horizontal diplopia, an unusual left transverse sinus was identified. Dedicated 2D time-of-flight (TOF) and contrast-enhanced magnetic resonance (MR) venogram images with 3D maximum intensity projection and coned in reconstructions of the intracranial venous system demonstrated a fenestration of the middle to distal aspect of the left transverse sinus (Figure 1), with the transverse sinus splitting into two equal parts approximately 2.8 cm distal to the torcular Herophili. The fenestration is also seen on contrast-enhanced images (Figure 2). At this level, the transverse sinus appeared increased in luminal caliber relative to the remainder of the sinus, where the fenestrated segment measured up to 1.1 cm in maximal thickness, though 0.4 cm distally and 0.7 cm proximally. The contralateral transverse sinus measured up to a maximal thickness of 0.7 cm, mirroring the conventional segments of the left. Distally the fenestrated left transverse sinus reunited with normal patency extending to the left sigmoid sinus. The left and right transverse sinuses were otherwise comparable with the straight sinus draining symmetrically into the right transverse sinus and left transverse sinus proximal to its fenestrated segment. This finding was felt to be incidental and not deemed to represent a cause for the patients presenting symptoms. The remainder of the examination demonstrated no other variation or abnormality.
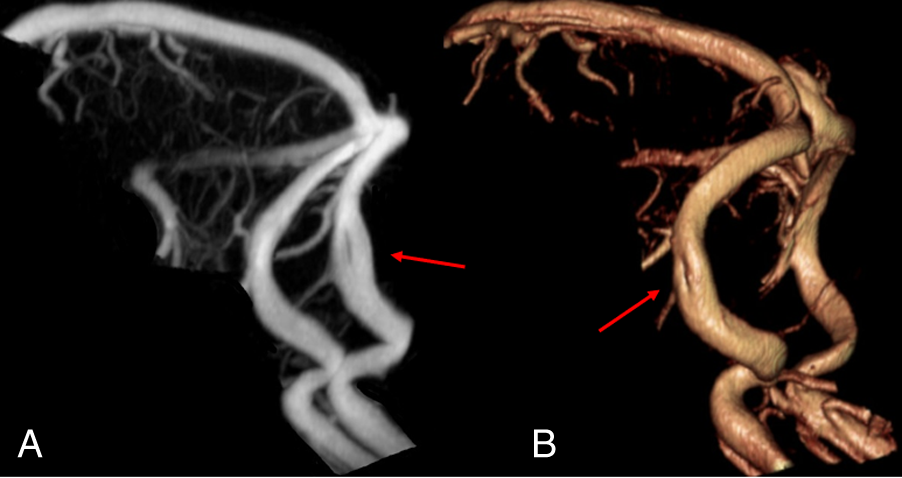
Figure 1: (A) Sagittal maximum intensity projection (MIP) reconstruction of the intracranial venous system demonstrating fenestration of the left transverse sinus (arrow), with a normal right transverse sinus seen superiorly. (A) Oblique coned in volume-rendered reconstruction of the major dural venous sinuses demonstrating fenestration of the left transverse sinus (arrow).
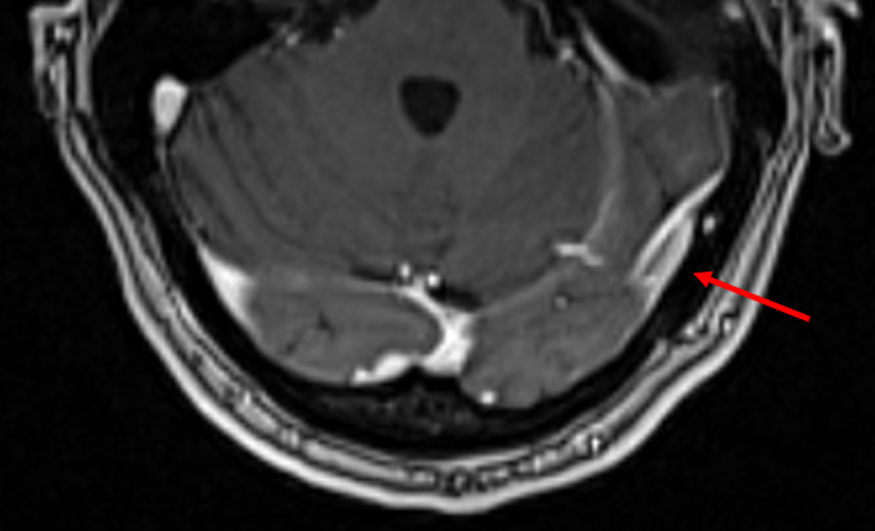
Figure 2: Axial contrast-enhanced MR venogram image coned to the posterior fossa demonstrating fenestration of the left transverse sinus (arrow).
Knowledge of the potential anatomical variations of the dural venous sinuses is critical to avoid erroneous neuroradiological interpretation, whether it be labeling them as pathology or failing to note their presence in cases of impending neurosurgical or endovascular intervention, which could lead to preventable complication. Here, we note a rare anatomical variation of a fenestration of the mid aspect of the transverse sinus, which could be mistakenly described as a nonocclusive thrombus or an arachnoid granulation. The diagnosis of venous thrombosis can be difficult even in the setting of complete occlusion and is often guided by a combination of nonspecific clinical signs, imaging studies, and a detailed knowledge of venous anatomy and potential variants. Cerebral angiography, the current gold standard, can be time-consuming and carries potential risk of the procedure itself. It has been shown that variants such as fenestration are not known to decrease the overall luminal caliber of the vessel, whereas even nonocclusive thrombus will result in a decreased luminal caliber. Reference Leach, Fortuna, Jones and Gaskill-Shipley4 Massrey et al. described a fenestration of the proximal aspect of the transverse sinus on a surgical specimen following removal of the brain and dissection of the venous sinuses of the posterior fossa. Reference Kouzmitcheva, Andrade and Muthusami5 A recent study measuring clinical outcome in pediatric stroke patients with venous thrombosis after recanalization found duplications/fenestrations of a major dural sinus in 14% of cases, though data on the prevalence of the transverse sinus itself is limited. Reference Kouzmitcheva, Andrade and Muthusami5 Massrey et al. described a fenestration of the proximal aspect of the transverse sinus on a surgical specimen following removal of the brain and dissection of the venous sinuses of the posterior fossa. Reference Massrey, Altafulla and Iwanaga6
Many variations have been described in the literature, the most common being hypoplasia of the left transverse sinus, which has interestingly been shown to be more common in male compared to females, determined by a retrospective study on adults as determined by 3D MR venography. The transverse sinuses were symmetrical in 66.9% of patients. Among the remaining third, the left was hypoplastic in 21.3%, and aplastic in 4.1%, whereas the right was hypoplastic in 5.5% and aplastic in 0.7%. The remaining 1.6% of patients showed bilateral hypoplastic transverse sinuses. Reference Goyal, Singh, Bansal and Paliwal7 Browder and Kaplan reported a superior sagittal sinus that demonstrated a doubling of luminal caliber at its distal aspect with a subsequent smaller associated transverse sinus. They also reported a case of transverse sinuses consisting of numerous connections to the torcular Herophili. Reference Browder, Kaplan and Krieger8 McCormick et al. removed 36 sinuses from the transverse through the sigmoid from 19 cadavers, identifying a septum or blind pouch in 72.2% of total sinuses, with over a 40% having greater than one septation or pouch, and greater than a third of the septations and one-quarter of pouches being large, defined by creation of an opening greater than 5 mm, findings that not only have importance to the endovascular surgeon, but also may contribute to the pathophysiological etiology of venous sinus diseases such as idiopathic intracranial hypertension. Reference McCormick, Bartels, Rodriguez, Johnson and Janjua9
Numerous variations of the dural venous sinuses, including the transverse sinuses, have been described and are not uncommon. We however report a rare variant of fenestration of the transverse sinus, knowledge of which, along with other potential anatomical variations, is important to avoid mislabeling it as pathology, as well as to the endovascular surgeon to prevent surgical complication.
Data Availability Statement
This manuscript contains no data. Any images are available upon request.
Code Availability
Not applicable.
Statement of Authorship
All authors contributed to the study conception and design. Material discovery was performed by RA and DAM. The first draft of the manuscript was written by DAM, and all authors commented on previous versions of the manuscript. DAM continued to review and edit the manuscript until it reached a final state, under the direct supervision of RG. All authors read and approved the final manuscript.
Funding
The authors declare that this research was not funded.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Ethical Approval
No ethics approval was required for this manuscript.




