Although sodium is an essential nutrient, most people consume more than they require for good health and more than dietary guidelines recommend. Few countries meet the WHO-recommended population dietary target of a maximum of 5 g of salt daily( Reference Brown, Tzoulaki and Candeias 1 ). New Zealand's mean population intake is likely to be about 3500 mg Na/d (equivalent to about 9 g salt/d) according to 24 h urinary assessments in 1998 and spot urinary sampling in 2008/09( Reference McLean, Williams and Mann 2 , 3 ). These estimates are consistent with data from similar countries, such as Australia and the USA, and with the conclusion that excessive sodium intake is a global nutrition problem( Reference Webster, Dunford and Huxley 4 – Reference Peralez Gunn, Kuklina and Keenan 7 ).
Population-wide dietary salt-reduction strategies would efficiently and cost-effectively reduce mortality and morbidity from CVD (particularly stroke and IHD), and thus reduce health-care costs( Reference Bibbins-Domingo, Chertow and Coxson 8 ). Modelling of the health impact of a 15 % and 25 % reduction in sodium intake from processed foods in New Zealand and Australia in 2008 has estimated that this would result in a 10 % reduction in total burden of disease from stroke and a 12 % reduction of the total burden of disease from myocardial infarction by 2018( Reference Goodall, Gallego and Norman 9 ).
In Western diets, about three-quarters of sodium consumed comes from processed foods, while only 10–15 % is added in the home during cooking or at the table( 10 , Reference Mattes and Donnelly 11 ). These data suggest that measures to reduce the salt ingested via processed foods are essential to reducing salt intake.
The UK Food Standards Agency's salt risk-management strategy has been identified as a leader in population salt reduction around the world( Reference He and MacGregor 12 ). This strategy attempts to reduce salt intake using two approaches: altering the food supply and changing consumer demand for high-salt foods. Reformulating processed food to contain less salt represents a simple measure that does not require behaviour change by consumers. However, because reformulation requires cooperation from the food industry, it may take longer to deliver population-level benefits and, for this reason, attention has also focused on interventions that would shape demand. Demand-oriented initiatives such as consumer education also have the ability to increase consumer interest in lower-salt foods, which provides an incentive for the food industry to reformulate.
Demand-oriented initiatives (which encourage individual consumers to moderate their intake) in the UK have included a sustained public-awareness campaign that aims to educate consumers about the adverse health effects of a high salt intake and show them how to interpret food labels and identify low-salt options( 13 ).
A number of labelling options exist for communicating nutrition information about salt. The Nutrition Information Panel (NIP), mandatory in New Zealand, is usually found on the back or side of a package( 14 ). It is detailed and numeric, and usually uses very small font. The Percentage Daily Intake (PDI) label has been developed by the food industry and is situated on the front of many products available in New Zealand( 15 ). The Multiple Traffic Light (MTL) label is a voluntary front-of-pack labelling system that has been used in the UK, where it has been an important tool for communicating sodium information( Reference McLean, Hoek and Hedderley 16 , Reference Malam, Clegg and Kirwan 17 ). In New Zealand the term ‘sodium’ is used on the NIP and PDI, whereas the currently permitted nutrition claims are ‘low salt’ and ‘reduced salt’( 18 ). The MTL, currently not in use in New Zealand, uses the term ‘salt’. Figure 1 shows examples of these nutrition information formats.
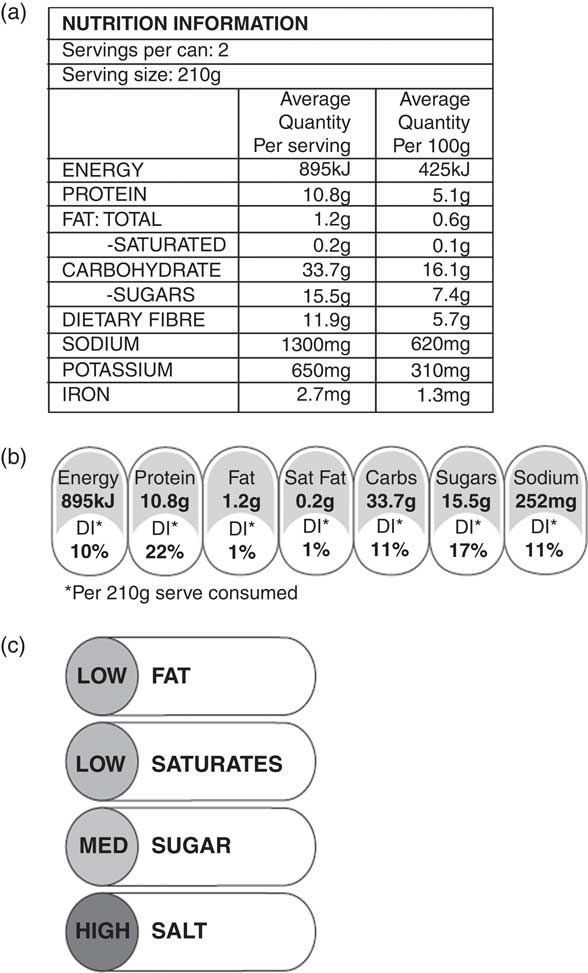
Fig. 1 Examples of the three nutrition labelling formats shown to participants: (a) the Nutrition Information Panel (NIP), (b) the Percentage Daily Intake (PDI) label and (c) the Multiple Traffic Light (MTL) label
Yet, despite the public health benefits of reducing sodium intake and the apparent success of campaigns such as the Food Standards Agency initiative( Reference Sadler, Nicholson and Steer 19 ), critics have argued that governments and health promoters should not advocate dietary change. Instead, they regard food choice as a matter of personal responsibility( Reference Feltin 20 , 21 ) and claim ‘it is easy to choose less salt’( Reference Smith 22 ). More generally, these arguments assume that consumers:
-
1. are aware of the potential health risks associated with different levels of salt intake;
-
2. have ready access to low-salt foods (which in reality are often not available)( Reference McLean 23 );
-
3. can distinguish between products with high and low salt options;
-
4. are able to determine their salt intake by interpreting nutritional information on packaged foods; and
-
5. choose to maintain their current dietary salt intake.
According to these assumptions, consumers must engage in ‘high involvement’ processing when making food choices. However, consumers’ processing of information occurs along a continuum, such as the one described in the heuristic–systematic processing model( Reference Chaiken 24 ). Consumers engaged in systematic processing require knowledge, cognitive capacity and high motivation to amass, consider and then use information when making deliberate choices. By contrast, heuristic processing bypasses ‘detailed information processing’( Reference Chaiken 24 ) and relies on simple rules or simple visual cues. This route requires less motivation and cognitive capacity, thus it may involve ‘learned knowledge structures’( Reference Zuckerman and Chaiken 25 ) such as those arising from often-repeated behaviours, including habitual food choices.
Recent empirical and theoretical evidence questions the assumption that consumers make decisions informed by the available information. For example, consumers overestimate their use of nutritional information on food labels( Reference Ni Mhurchu and Gorton 26 , Reference Tanner and Carlson 27 ) and make little use of it because they find the details too time consuming to read( Reference Signal, Lanumata and Robinson 28 ). Furthermore, many consumers lack the mathematical ability and nutritional knowledge to understand and use the information provided( Reference Ni Mhurchu and Gorton 26 , Reference Rothman, Housam and Weiss 29 ). The rapid decision making typical of supermarket purchases may also preclude adequate label review( Reference Hutchinson and Alba 30 ), encouraging consumers to employ heuristic, or cue-based, decision making when making food purchases( Reference Hamlin 31 ). Limited time, distracting environments and pressure to make multiple simultaneous decisions, typical of supermarket shopping environments, may thus preclude systematic processing and predispose heuristic processing( Reference Zuckerman and Chaiken 25 , Reference Feunekes, Gortemaker and Willems 32 ).
While, in principle, consumers may control their salt intake by identifying foods with healthier nutrition profiles( Reference Wilkinson and Marmot 33 ), their backgrounds and choice contexts may militate against the systematic processing required to achieve this outcome. The assumption that consumers engage in systematic decision making may lead to illogical conclusions about the information they require, particularly at the point of purchase. If, as the evidence suggests, consumers engage in heuristic processing, they need simple labelling formats to compensate for their incomplete nutrition knowledge and the limited time they have to analyse and interpret complex nutrition information.
To examine this question further, we drew on the heuristic–systematic processing model to investigate consumers’ behaviour in relation to salt intake. We used a convenience sample of New Zealand adult grocery shoppers to explore the following research questions:
-
1. What factors influence consumers’ food choices?
-
2. What role does nutrition knowledge and nutrition information/labelling play in food choice?
-
3. How do consumers understand sodium/salt intake and labelling?
-
4. How do consumers perceive alternative label formats and their presentation of sodium information?
Methods
Study design
We conducted face-to-face semi-structured interviews in April 2010 with sixteen adults (ten women and six men) aged 28–63 years who had at least some responsibility for grocery shopping (at least once per month) within their household. Participants were recruited through community organisations and networks, public advertising and some snowball sampling. Sampling continued until few new insights were achieved from subsequent interviews( Reference Daly, Willis and Small 34 ). One researcher conducted all sixteen interviews. Each interview lasted approximately 40 min, was recorded with consent and then transcribed verbatim. Participants were offered a $NZ 20 supermarket voucher as a token of appreciation. A Department of Marketing Ethics reviewer with delegated authority from the University of Otago Ethics Committee reviewed and approved the research procedures; participants were informed of their rights and gave written consent prior to participating in the research.
Materials
We first discussed how participants made food choices, their general use of nutrition information and specific use of salt or sodium information. We also explored participants’ understanding of the difference between sodium and salt (sodium chloride), as both terms are used on existing nutrition labels: ‘sodium’ on the NIP and PDI labels, and ‘salt’ on nutrition-related claims and MTL labels (see Fig. 1). We then examined participants’ knowledge of health risks associated with sodium and sought their views on three different types of food labels (Table 1 summarises the interview protocol).
Table 1 Overview of the semi-structured interview protocol: main sections and questions
Analysis
Two researchers reviewed the transcripts, analysed the data and identified themes. We identified themes using thematic analysis as described by Braun and Clarke, where ‘thematic analysis involves searching across a data set … to find repeated patterns of meaning’( Reference Braun and Clarke 35 ). Thematic analysis also allows for interpretation of the data according to the judgement of the researcher( Reference Braun and Clarke 35 ); in this case, we used heuristic–systematic processing theory to interpret themes within the data set.
Results
Table 2 shows the demographics of participants. Mean age was 41 (sd 10) years. When participants were asked to report their highest level of education, four (25 %) reported school qualifications, nine (56 %) reported that they had bachelor's degrees, certificates or diplomas, and three (19 %) had postgraduate qualifications. Eighty-one per cent (n 13) reported their ethnicity as New Zealand European.
Table 2 Demographic characteristics of participants (a convenience sample of sixteen adult grocery shoppers)
F, female; M, male; NZ, New Zealand.
We identified four key themes: (i) the dominance of price and habit; (ii) the challenge posed by nutrition information; (iii) salt as a mysterious ingredient; and (iv) breaking the code of nutrition labels.
Dominance of price and habit as choice determinants
Participants reported that practical considerations dominated their food purchase decisions. Most used a list when shopping, although many also looked for ‘specials’ or price-reduced items. Price was the most salient feature both when choosing what to buy and when selecting between competing products:
‘I try and shop for major things like meat – whatever is on special. … Price is important.’
Participants also deliberately looked for brands they knew, or had purchased and used before, and often associated familiarity with quality and value for money:
‘You might stick with a brand even though it is more expensive.’
There was sometimes a tension between price and perceived quality, and several participants used a lower price to infer a poorer-quality product. While many referred to food quality as important, they typically judged quality by price and taste rather than nutritional content:
‘Because sometimes with the cheaper price you do compromise quality of the product … sometimes you know for example if you are shopping at Countdown and Woolworths there is home brand, which is a generic product at a reasonable price, but then you compromise on some quality of the product. So if you go to the higher brands you will possibly get a better product. But mainly I guess it is taste preference. I guess with the brands that are in the middle that are very similar, that is distinguished on price I guess. So there is those two factors, quality and price.’
This tension emerged strongly when consumers reported purchasing a ‘new’ or unfamiliar product, in which case they would deliberately not choose the cheapest product, which they assumed would be of poor quality, and instead would opt for a mid-price product or a familiar brand:
‘The ones we know, we pick those or have used before. If it was a new product we hadn't tried I would probably pick something from the top end, I think, rather than the lower end in price.’
‘We go by what we know and if it is an unknown brand you might take price into consideration. But generally stick with what you know.’
In other words, participants used the simple cues of price and brand familiarity to support their food purchase decisions; none reported using nutrition information or referring to the NIP or saw either as a determinant of quality.
The challenge posed by nutrition labelling
After commenting on the general factors they considered when purchasing food, participants were then asked general questions about nutrition labelling, and more specific questions about sodium and salt labelling and different label formats (see Table 1). Although many participants (n 13) recalled having seen nutritional information on foods, most (n 9) did not pay particular attention to it. The few who had examined nutrition information were generally unable to interpret or understand the details provided and, because of this, noted that it had not influenced their food choices:
‘… occasionally I will have a look. But I don't think I change any purchasing decision on what I see.’
Regardless of whether participants looked at nutritional information or not, neither the NIP nor the PDI appeared to influence their food choices. Yet, despite not using food labels, participants reported that they paid attention to eating healthy food and saw this as important. Paradoxically, participants’ belief that they ate healthy food meant that they did not need to refer to nutrition information:
‘You have already thought about the nutritional value of the whole meal. So I guess the components individually don't really factor. But in terms of say buying a one-off product I don't tend to turn over and look at the nutritional information.’
For example, in answer to the question ‘Have you ever noticed nutrition information on food products that you buy?’, participants reported relying on simple rules (such as ‘I eat healthily’) to obviate the need to make sense of details that are not intuitive:
‘Never. And I think the reason is. I eat very, very healthy, but funnily enough I never read the things on the side.’
‘… because I can never remember what it all means. I worked in science for 23 years and I know all the things to do with % weight volume etc. But you look at this and it says 50 kilojoules of what? Not very meaningful. I know that they have talked about it on TV about people don't know what all this stuff means.’
The minority (n 4) who reported routinely reading nutrition information did so in relation to particular macronutrients such as fat and sugar, and because of specific nutritional requirements (such as a need to check sugar content for a diabetic family member). However, on probing, even participants who catered to specific dietary needs did not have a systematic approach to using and interpreting nutrition information to make purchase decisions.
Salt – a mysterious ingredient
When asked specifically about salt, no participant had the background knowledge required to interpret the nutrition information present in existing labels. While most (n 10) recognised that salt content was labelled as sodium, they did not understand the relationship between the two (namely, that salt is sodium chloride and that by weight sodium is only 40 % of salt). Their comments suggest sodium may be alternatively a refined version of salt or the raw ingredient from which salt is manufactured and display a very limited understanding of this ingredient:
‘Sodium's chemical formula is Na, salt is NaCl, so you don't get a lot of pure sodium. Well I guess you do. Don't know.’
‘Is it [sodium] the raw product? I don't know.’
Few participants understood the relationship between sodium and health risks. Even when asked specifically if they had heard of any health problems associated with salt intake, many (n 10) loosely linked sodium intake and blood pressure, but few (n 5) could clearly articulate this relationship. Thus, while most recognised that too much dietary salt could be harmful, they did not understand why this was so and only a minority related salt intake to heart disease, high blood pressure or kidney disease. Ironically, participants were more concerned they might be consuming inadequate quantities of salt, which they believed could be bad for their health:
‘It used to be because of heart problems, heart disease and high blood pressure. Funnily enough science has turned backwards … Same with salt, if you stop taking salt then you get cramps so you do virtually need some. The key rule is moderation.’
Participants also confused the health-related effects of salt and iodine intake. In New Zealand, some table salt is iodised, while rock or sea salt is generally not iodised, and with the exception of most breads, most manufactured food contains non-iodised salt. Despite the fact their diets were likely to contain largely non-iodised salt, several participants conflated adequate iodine intake with salt intake and could not differentiate between the two nutrients. This confusion was most striking when participants explained why they thought there is a maximum recommended daily intake for salt:
‘For prevention of goitre isn't it? And hypothyroidism. I think that's what it is for. Or the heart condition. I say the salt intake would be hypertension, or people who have heart disease, or obese. I guess is why they would have those guidelines.’
‘Goitre is lack of iodine isn't it which is part of the whole salt thing?’
Not surprisingly, given this confusion, none of the participants could quantify the recommended upper level of dietary intake for either sodium or salt. Their confusion has important practical implications as the NIP expresses sodium content in milligrams or milligrams per serving, figures that are meaningless unless they can be interpreted in the context of a recommended or expected dietary intake. While the PDI presents the milligram amount as a percentage of a recommended daily intake, participants thought this information was only useful for consumers with a high degree of nutritional knowledge and motivation, unlike the ‘average’ consumer.
Although a few participants reported noticing some nutritional information regarding sodium, none used a systematic approach to evaluate these details; nor could any explain how they interpreted the sodium content in food:
‘I look at it as I go down and think it is rather high but don't know what the recommendations are.’
‘Square table on the back … per unit weight. Not normally easy to work out.’
Even if they were motivated to use nutrition information, participants lacked the knowledge and ability required to interpret these details. Most had little knowledge of healthy sodium intake or how they should interpret the information on labels regarding sodium. Some did not know where to find information about a product's sodium content and incorrectly reported that the best place to look for this information was in the ingredients list or somewhere ‘on the back’ of a package (rather than specifically identifying the NIP). Even those who had noticed information about sodium on food labels lacked the ability to interpret it meaningfully. As a result, they could only engage in heuristic decision making where they used past choices and relied on self-reflexive beliefs to inform their behaviour.
Further, participants believed that only people other than themselves should be concerned with their salt intake. While some correctly identified population groups that may be particularly adversely affected by a high salt intake (obese people, people with heart disease or high blood pressure, those over 40 years of age), none appeared aware that most people's intake exceeded dietary guidelines. Participants were not concerned with their own salt intake, largely because they believed their healthy eating patterns, low consumption of processed foods and practice of not adding salt during cooking meant they consumed little salt. Participants consistently relied on rationalised heuristics such as ‘I eat healthily’ to justify their beliefs, despite their inability to interpret nutrition information.
When asked how they would reduce dietary salt, participants suggested adding less salt in cooking, limiting salty snacks and taking salt off the table. While some advised checking nutrition labels, they lacked confidence in their ability to understand or interpret existing nutrition information:
‘I guess you would have to start looking at the nutritional information on the back of products, but also I guess limit your intake of known salt foods. Or limit your usage of salt on food. But I guess you would have to start monitoring how much salt you are using or eating in manufactured products … I don't find either [nutrition labels] easy to read … I think that a lot of people, just average Joes like myself, wouldn't connect salt and sodium together if they hadn't been told or picked it up as general knowledge. So for them if they were looking for salt it would mean nothing to them.’
Breaking the code: interpreting nutrition labels
Participants were shown and asked to interpret NIP, PDI and MTL labels. Despite the widespread use of the former two labels in New Zealand, participants were unable to interpret the nutrition information present. While some thought the detailed numerical information might be useful to people paying particular attention to their salt intake, none of this relatively educated sample could interpret the information themselves. Several noted they would need to learn more before they could interpret and use a PDI label. Participants favoured instead the MTL label, which is not currently used in New Zealand. They noted how easily they could interpret the traffic light colour scheme and preferred the fact this label referred to ‘salt’ rather than ‘sodium’:
‘The traffic light because you see traffic lights all the time, and if red is bad that is bad. I think that that would be pretty much an appealing option. If I knew more about them, probably the percent daily intake.’
‘That is exactly what you need. The green for go and the red for stop. I think that is very good … Yes. It is good to see and catches the eye. Just a quick scan down. Your average person, you ask them what is a milligram? They have no idea. So I tend to think what we do is make it very scientific instead of an easy way. I think the visual green, orange and red is better … [the PDI] gives you more information, but I don't think they will understand it unless you specifically know about it.’
Traffic light labels use a visual heuristic to communicate complex information, something participants clearly preferred as they could access, understand and use the colours to assess alternative products. Visual labels make fewer cognitive demands on consumers and so require neither the detailed systematic processing consumers must engage in to interpret the heavily numeric NIP and PDI nor the background knowledge they must bring to this task.
Discussion
The evidence that reductions in sodium intake will bring about public health benefits is strong, but debate continues over the best way to achieve this goal. While mandatory changes in food supply could bring about rapid changes in sodium consumption, governments have been reluctant to impose measures on the food industry. Many countries (including the UK( Reference Sadler, Nicholson and Steer 19 ), Canada( 36 ) and Australia( 37 )) have instead instituted the setting of voluntary sodium-reduction targets. Evaluation of the comprehensive salt-reduction programme in the UK has shown a nearly 15 % reduction in population sodium intake between 2000–01 and 2011( Reference Sadler, Nicholson and Steer 19 ). Educational approaches, such as nutrition labelling of food, are also widely endorsed. However, the labels currently used in many countries make considerable demands on consumers, assume systematic processing occurs, and overlook the exigencies consumers face when making food choices.
Despite some claims that consumers are aware of their salt intake and its consequences, and manage this using nutrition information( Reference Feltin 20 – Reference Smith 22 ), the consumers we interviewed had low awareness of dietary sodium and little understanding of current food labels. They compensated for this lack of background knowledge by using simple rules to reassure themselves they followed a healthy diet, thus exempting themselves from risk. While concerned to eat a healthy diet, participants believed this was already the case and so had little motivation to monitor their salt intake. Participants used ‘learned knowledge structures’ that support heuristic processing, relying on simple rules (such as ‘I eat healthily’) to obviate the need to make sense of details that are not intuitive. As a result, they made food choices using price, familiarity and perceived quality heuristics, from which they inferred healthful attributes. For these particular individuals the strategies they outlined may be justified, but as the population-level data for sodium intake indicate, they are not successful strategies in general.
Even if our participants had been highly motivated to assess the salt levels in their diet, they lacked the knowledge required to interpret information currently available on packaging in New Zealand (the NIP and PDI). They were also unaware of current nutrition guidelines, including recommended upper intake levels, and so could not interpret sodium content in any context. Despite the PDI label's attempt to place nutrient content in the context of a daily diet, participants regarded the PDI as useful only to those with expert knowledge and high motivation, rather than the ‘average consumer’.
Participants’ inability to interpret nutrition information regarding sodium content meant they were unaware of their own intake and would be unable to use current on-pack nutrition information to lower this if required. The limited influence of numeric information provided in NIP and PDI supports earlier arguments that few consumers engage in systematic processing when making food choices( Reference Hamlin 31 ). Participants’ response to the simple visual cues provided by traffic light labels highlights the role heuristics play in their decisions and suggests an opportunity for policy makers to implement measures that correspond to consumers’ actual behaviour. The logic of using labels such as the NIP and PDI, which require systematic processing, is flawed, given the evidence that consumers rarely engage in this level of analysis when making supermarket food purchases.
A substantial body of international evidence supports the introduction of front-of-pack MTL format nutrition labelling in order to enhance consumers’ ability to interpret information regarding a range of nutrients on nutrition labels( Reference Cowburn and Stockley 38 ). A review of front-of-pack label formats in the UK found that a combination of MTL and PDI information enhanced comprehension and consumer awareness of the nutritional content of foods( Reference Malam, Clegg and Kirwan 17 ). New Zealand research also supports the use of MTL formats to enhance consumers’ ability to understand nutrition information and discriminate between similar products with different nutritional profiles( Reference Maubach, Hoek and Gendall 39 – Reference Gorton 41 ).
Our results are consistent with quantitative survey results about consumer attitudes and knowledge related to salt consumption in many other countries. A recent Australian survey showed that while most consumers were aware of a relationship between dietary salt and adverse health consequences, fewer than half of those surveyed understood the relationship between sodium and salt, and only one-fifth reported regularly using nutrition information about salt content to inform purchasing behaviour( 42 ). Similarly, surveys in Canada and other Central and South American countries have shown that despite widespread awareness that a high-salt diet is associated with adverse health outcomes, consumers had a limited understanding of how to restrict their own salt intake( Reference Papadakis, Pipe and Moroz 43 , Reference Claro, Linders and Ricardo 44 ). Evidence from the UK has shown increased consumer efficacy, with less salt added at the table and improved ability to select low-salt foods following extensive public-awareness campaigns( Reference Sutherland, Edwards and Shankar 45 ).
There are some limitations to the generalisability of the present research. We used a convenience sample that is not necessarily representative of the wider community. Its relatively small size meant we could not explore knowledge, perceptions or preferences among people of different ethnicities or socio-economic status. Participants were relatively well educated and predominantly of New Zealand European ethnicity. For example, 75 % of our sample had a tertiary education qualification, compared with an estimated 41 % of the New Zealand population aged 25–64 years( 46 ). Well-educated consumers are more likely to be concerned about health and nutrition and more likely to have the knowledge and skills to interpret nutrition information. Our findings are therefore likely to overestimate consumers’ ability to interpret information on salt content since education has been shown to be positively correlated with label use( Reference Baltas 47 ). Participants were asked to record their ethnicity, with 81 % reporting they were of New Zealand European ethnicity, compared with only 60 % in the most recent (2006) New Zealand census( 48 ). In particular, indigenous Māori and Pacific people are not represented, who make up 14 % and 6 % of the population, respectively( 48 ). Surveys have shown that Māori and Pacific consumers use available nutritional information (NIP and PDI formats) less than New Zealand European consumers, and are less able to interpret information on these formats( Reference Signal, Lanumata and Robinson 28 , Reference Gorton, Ni Mhurchu and Chen 49 ). As a result, we suggest that the need to recognise how consumers make food decisions, and to provide information in a format they can actually use, is even greater than indicated in our study.
The present results show a need for education of New Zealand consumers if dietary sodium reduction is to be achieved. This should include information about the health benefits of sodium reduction and information about how this can be achieved, including information about how to interpret nutrition information on food labels. Unfortunately, even optimal label formats, such as traffic light labels, may have a limited effect on sodium intake if consumers’ choices remain high in sodium. Population-level reductions in salt intake will be difficult to achieve while salt remains widely used in processed foods and consumers have few low-salt options available to them( Reference McLean 23 ). Thus, while policy makers should implement label formats that help consumers in discriminating between high- and low-salt foods( Reference McLean, Hoek and Hedderley 16 ), they should also consider supply-based changes which do not require behaviour change by consumers.
Acknowledgements
Sources of funding: This work was supported by a grant from the Health Research Council of New Zealand. Conflicts of interest: There are no conflicts of interest. Authors’ contributions: R.M. conducted the interviews and wrote the manuscript; R.M. and J.H. designed the study and analysed the transcripts; both authors have contributed to the final manuscript.





