TAKE HOME:
• Aconite toxicity, resulting from depolarization of sodium channels, can result in respiratory arrest and ventricular dysrhythmias
• Technologic innovations can be applied at the point of care to focus patient care and avoid unnecessary treatments
INTRODUCTION
Aconitum, also known as aconite, monkshood, and wolfsbane is a genus of over 300 species of flowering plants belonging to the Ranunculaceae family.Reference Nyirimigabo, Xu, Li, Wang, Agyemang and Zhang1 Given its unregulated use in Traditional Chinese Medicine (e.g., topical analgesic, antirheumatic, etc.), mistaken identification for similar appearing nontoxic edible plants (e.g., parsley, horseradish), and narrow therapeutic range, multiple case reports of aconite toxicity have been previously documented in the literature with variable outcomes.Reference Nyirimigabo, Xu, Li, Wang, Agyemang and Zhang1,Reference Li, Liu, Zhu and Liu2
Aconite, an alkaloid known to depolarize voltage-gated sodium channels, primarily targets muscle, neural, and cardiac tissues, resulting in symptoms ranging from nausea, vomiting, weakness, and paresthesias to dysrhythmias (brady- and tachy-dysrhythmias) and hypotension.Reference Nyirimigabo, Xu, Li, Wang, Agyemang and Zhang1,Reference Lin, Chan and Deng3 However, management is primarily supportive.
Our case describes the use of a photo-based plant identification smartphone application in the emergency department to rapidly identify this dangerous plant, direct appropriate management, and avoid unnecessary treatments.
NARRATIVE
A 53-year-old male began to experience nausea and recurrent bouts of vomiting after ingesting what he thought to be parsley from his backyard at approximately 21:00 on the day of presentation. The patient's home medications included bisoprolol 5 mg by mouth (PO) once a day (OD) for hypertension and sildenafil 50 mg PO OD as needed for erectile dysfunction; he had only used his bisoprolol as prescribed that day.
Initial examination at 23:00 demonstrated a pulse of 50, blood pressure of 73/47 mm Hg, respiratory rate of 32, oxygen saturation of 100% on room air, temperature of 35.9°C, blood glucose of 5.8 mmol/L, and a Glasgow Come Scale score of 15. Clinically, his pupils were 4 mm bilaterally and reactive. He was diaphoretic, tearing, had multiple episodes of vomiting (with evidence of the ingested plant in his vomitus), and uncontrolled diarrhea. Electrocardiograms revealed episodic bouts of sinus tachydysrhythmias (see the online Appendix Figure 1). As a poisonous plant ingestion was suspected, consideration was given to organophosphate poisoning or cardiac glycoside toxicity. However, the patient had lived in his home for years and denied any pesticide application to his garden. While several features did not fit with digoxin toxicity (i.e., supraventricular tachydysrhythmias, hypotension, intact cognition, low-normal serum potassium), we planned to empirically treat with Digibind.
Fortunately, his family presented with a sample of the plant. One emergency physician used a photo-based plant identification application (“PictureThis - Plant Identifier”) on his smartphone to identify the plant as Monkshood (Aconitum napellus) (Figure 1; online Appendix Table 1). With the plant identified, the poison control center was able to advise on management of aconite toxicity, and we avoided the use of Digibind.
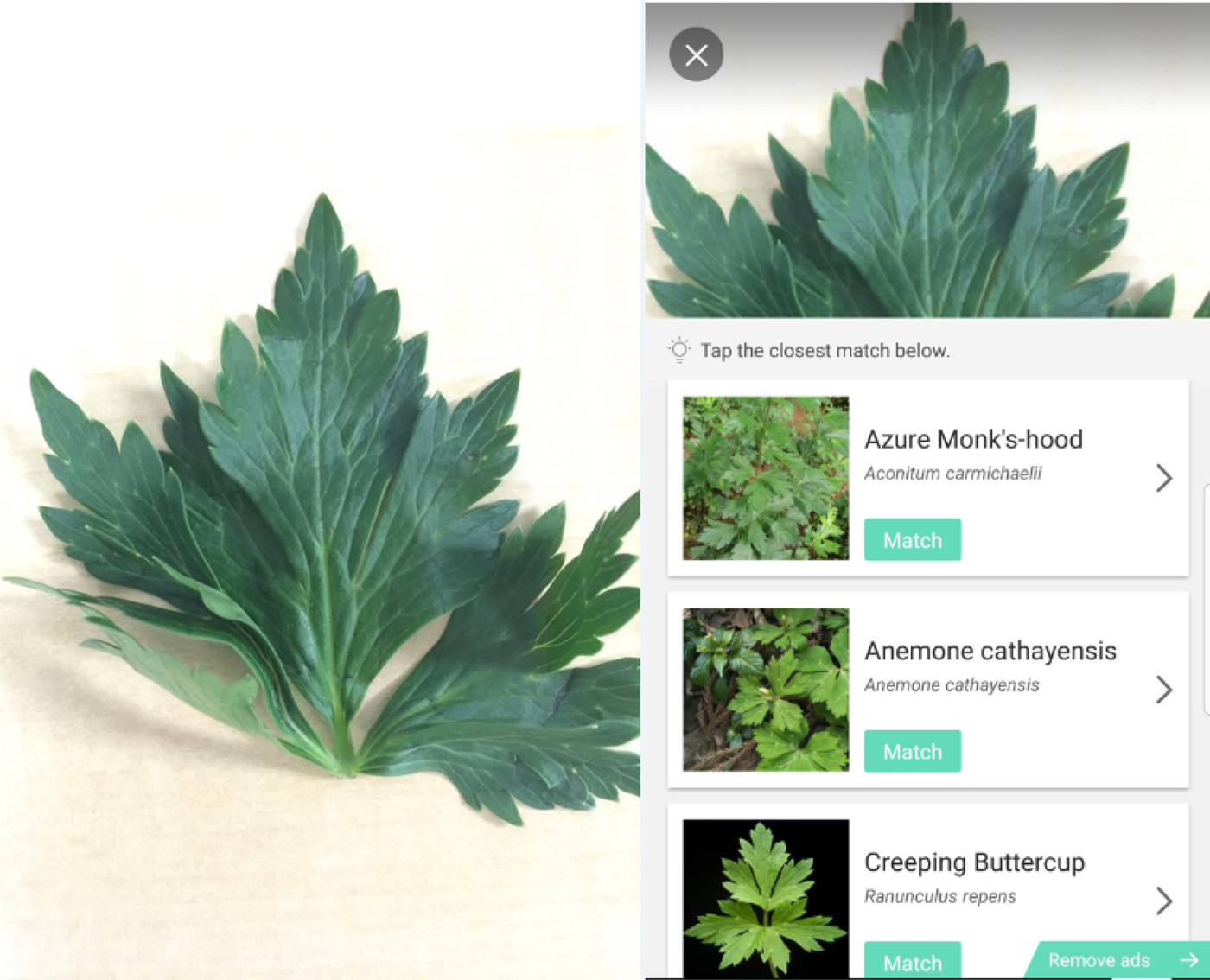
Figure 1. Plant sample provided to the ED (left). PictureThis Plant Identifier application output (right).
Despite resuscitation, the patient remained hypotensive and, thus, was started on a norepinephrine infusion of 5 μg/minute. Pertinent initial investigations are detailed in the online Appendix Table 2. Given the risk of dangerous ventricular dysrhythmias and respiratory arrest, he was dispositioned to the intensive care unit for ongoing observation. During the subsequent 4 hours, he remained on a norepinephrine infusion at 5 μg/minute for persistent hypotension. He was slowly weaned and normotensive over the next 24 hours. He otherwise remained in normal sinus rhythm without any evidence of dysrhythmias for the remainder of his stay.
Subsequent to the patient's discharge, a picture of the plant leaf was examined by 2 botanists and identified as a leaf from a plant in the genus Aconitum (see Appendix 1).
DISCUSSION
This case illustrates the dramatic and potentially life-threatening consequences of aconite toxicity, which has previously been well documented in the literature. As such, the pathophysiology and management are described elsewhere.4 However, this case also highlights the use of a photo-based plant identification smartphone application to assist in the identification of a toxic plant. The use of this resource dramatically changed management in our emergency department, as by utilizing this application and successfully identifying this plant, we averted the empiric use of Digibind, its associated cost (10 vials Digibind × $4,336 USD per vial = $43,360), and potential side-effects.5
Currently, there are a several photo-based identification applications that help users identify a multitude of plants, insects, snakes, rashes, and pills. In our experience, these applications are uncommonly used on the frontlines of medical care; however, we believe they have the potential to significantly alter patients’ treatment in the emergency department by assisting clinicians in identifying uncommon presentations to rapidly focus management.
Nevertheless, we recognize that there are inherent risks in using such applications (known as a Software as a Medical Device [SaMD]), including false negative results (i.e., falsely identifying a toxic plant as nontoxic) and false positive results (i.e., misidentification resulting in delayed, unnecessary, or no treatment). To mitigate these risks, we believe SaMDs should be treated in manner similar to diagnostic tests with + rigorous evaluation with development and validation studies, and approval by a regulatory health body before their use in clinical care. Both the United States Food and Drug Administration and Health Canada have recognized this challenge and have endeavored to regulate this developing sector by publishing guidelines on their use.6,7 Furthermore, end-users require formal education and training on the characteristics of SaMDs to appropriately use them in clinical care. This poses a unique challenge as most SaMDs are freely and readily available for download from many application stores. Thus, we believe the onus is on developers to educate end-users on the safe use of a SaMD, possibly by building-in education or requiring certification.
Our case study is limited by two factors. First, the lack of a digoxin level on presentation to exclude digitalis toxicity. While this would have helped with possibly ruling out alternative diagnoses, digoxin toxicity is treated empirically on presentation and thus a digoxin level was not requested. Second, as “PictureThis – Plant Identifier” is a private corporation, we were unable to elucidate details of their machine learning algorithm.
Despite these limitations, we believe researchers and clinicians should consider further development of innovations such as photo-based identification smartphone applications as they can assist with rapid identification of uncommon and dangerous etiologies, help guide appropriate care, and avoid unnecessary treatments. Future work should endeavor to elucidate the accuracy of such applications to enable informed use at the bedside.
Supplemental material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2020.30.
Acknowledgements
We thank Ms. Nadia Cavallin and Mr. Jon Peter from the Royal Botanical Gardens for their support in confirming plant identification, as well as the support staff at Glority LLC for details on the application.
Competing interests
None.
Financial support
None.



