Interpersonal psychotherapy (IPT) and cognitive–behavioural therapy (CBT) are effective short-term therapies for mild to moderate depression (Reference BeckhamBeckham, 1990; Reference Jarrett and RushJarrett & Rush, 1994; Reference Persons, Thase and Crits–ChristophPersons et al, 1996). Conversely, using psychotherapy for severe depression remains a contentious issue (National Health Committee, 1996; Reference Segal, Whitney and LamSegal et al, 2001; Reference Ellis and SmithEllis et al, 2002). The National Institute of Mental Health Treatment of Depression Collaborative Research Program (NIMH TDCRP) directly compared the two therapies (Elkin et al, Reference Elkin, Parloff and Hadley1985, Reference Elkin, Shea and Watkins1989) and reported a better response to IPT than to CBT in severe depression (Reference Elkin, Gibbons and SheaElkin et al, 1995). This particular finding influenced the development of many clinical guidelines, which do not support IPT and even warn against CBT as first-line therapies for severe depression. However, authors such as Thase & Friedman (Reference Thase and Friedman1999) reviewed the evidence for response to psychotherapy in patients with melancholic depression and advocated that a skilled therapist could work successfully with a carefully chosen patient.
In the Christchurch Psychotherapy of Depression Study we compared IPT and CBT for depression. We predicted that both therapies would be equally effective in reducing depressive symptoms. We also predicted that both therapies would be less effective in severe or melancholic depression.
METHOD
Patients with a principal diagnosis of major depressive disorder were recruited from a wide variety of sources, including mental health out-patient clinics, general practitioners, self-referral and psychiatric emergency services. No advertising for patients was involved. Recruitment occurred between August 1998 and February 2003. Patients were included if they were aged 18 years or over and currently met DSM–IV criteria for a non-psychotic major depressive episode as the principal diagnosis (American Psychiatric Association, 1994). Participants were required to be medication-free for a minimum of 2 weeks, or (to allow for clearance from the bloodstream) five drug half-lives of any centrally acting drugs, except for the occasional hypnotic agent and the oral contraceptive pill. Patients were excluded if there was a history of mania (bipolar I disorder), schizophrenia, major physical illness that could interfere with assessment or treatment, current alcohol or drug dependence of moderate or greater severity (if it was considered to be the current principal diagnosis) or severe antisocial personality disorder, or if the patient had failed to respond to a recent (within 1 year) adequate trial of either of the intervention therapies. The study was approved by the local Canterbury (New Zealand) ethics committee.
Assessment
After being referred, patients were screened over the telephone by a research nurse who confirmed depressive symptoms and checked inclusion and exclusion criteria. Those who appeared suitable for inclusion were seen by a psychiatrist, senior psychiatric registrar or clinical psychologist for an initial assessment. After giving consent, the patient then attended for a detailed clinical assessment. During this assessment participants were administered the Structured Clinical Interview for DSM–III–R (SCID; Reference Spitzer, Williams and GibbonSpitzer et al, 1992), with an expansion of DSM–III–R and DSM–IV criteria for melancholic and atypical depression. Other clinician ratings were the Montgomery–Åsberg Depression Rating Scale (MADRS; Reference Montgomery and ÅsbergMontgomery & Åsberg, 1979), the Hamilton Rating Scale for Depression (HRSD; Reference HamiltonHamilton, 1967) and the Mental State Examination (MSE; Reference Parker, Hadzi–Pavlovic and WilhelmParker et al, 1994). An independent research nurse completed the HRSD, the MADRS and the MSE. This nurse also completed outcome assessments and was therefore masked to the treatment allocation. Participants also completed a series of self-report questionnaires which included the second edition of the Beck Depression Inventory (BDI–II; Reference Beck, Steer and BrownBeck et al, 1987), the Hopkins Symptom Checklist (SCL–90; Reference Derogatis, Lipman and CoviDerogatis et al, 1973), the Structured Clinical Interview for Personality Disorders Questionnaire (SCID–PQ; Reference First, Gibbon and SpitzerFirst et al, 1997), and the Temperament and Character Inventory (TCI) (Reference Cloninger, Przybeck and SvrakicCloninger et al, 1994).
A neurobiological assessment was also included and blood was drawn for analysis of routine electrolytes, renal and hepatic function, blood glucose, blood count, thyroid function tests, a neuroendocrine assessment and DNA extraction. After this assessment, patients and therapists were advised as to whether the treatment would be either IPT or CBT. Patients were randomised to the two therapeutic interventions in a 1:1 ratio based on a computerised randomisation sequence of permutated blocks of size 20. Allocation of patients was performed by a person independent of the study.
Intervention
Following randomisation participants were booked to see their therapist on an approximately weekly basis, for 50 min sessions for a period of up to 16 weeks. The minimum number of sessions allowed to fulfil the definition of sufficient therapy exposure was 8 and the maximum was 19. The mean interval between baseline and follow-up assessments was 13.75 weeks. The protocol allowed for flexibility in the scheduling of appointments, including twice-weekly sessions for patients who were initially severely depressed and/or who had significant suicidal ideation, or less than weekly to allow for marked improvement in depression or patient and/or therapist availability (e.g. sickness, holidays). Following these weekly sessions, patients then received 3–8 approximately monthly maintenance sessions over a further period of 6 months. (The data presented here concern the outcome of therapy at the end of the 16-week treatment phase.).
If at any stage of therapy there was deterioration in depressive or suicidal symptoms which interfered with the process of psychotherapy, or there was a sustained lack of improvement of severe symptoms for more than 4–6 weeks, patients could be seen for clinical review by a study psychiatrist. The decision to review was made during group discussions at supervision and was a joint decision based on Global Clinical Impression. At this stage patients would be offered adjunctive treatment with antidepressant medication if this was deemed necessary. If antidepressant medication was used or the patient was lost to follow-up, the last medication-free depression severity rating was used as the measure of efficacy for the intention-to-treat analysis (last observation carried forward). All therapy sessions were audiotaped for the purposes of treatment integrity ratings, and would also be used in supervision.
Cognitive–behavioural therapy
Cognitive–behavioural therapy was based on the manuals of Aaron and Judith Beck (Beck et al, Reference Beck, Rush and Shaw1979, Reference Beck, Steer and Brown1987). In this therapy the therapist uses techniques related to the cognitive model of depression which help the patient identify negative thoughts, views, assumptions and beliefs about themselves, the world and the future that are related to their depressive symptoms and functioning. The manual suggests session-by-session guidelines, but, the therapy is tailored to meet each patient's specific needs in terms of pace and content. During early sessions the patient is educated about depression and the cognitive model, and behavioural methods are used to increase activity and facilitate cognitive change. In later sessions the therapist helps the patient identify negative cognitions which they then evaluate and substitute. In final sessions there is a focus on relapse prevention. Techniques used within sessions include the Socratic method of questioning, testing beliefs and assumptions, cognitive restructuring and use of homework.
Interpersonal psychotherapy
Interpersonal psychotherapy was based on the manual by Klerman et al (Reference Klerman, Weissman and Rounsaville1984). This therapy helps the patient identify and explore the social and interpersonal issues that relate to and maintain their depressive symptoms. The patient and therapist work together collaboratively and therapy is tailored to meet the needs of each patient. As a general guide, in early sessions the therapist develops an interpersonal inventory which details current and past important relationships and asks questions to identify any of the four key problem areas (grief, disputes, transitions and deficits) related to the depressive symptoms. Once a focus is agreed upon from one of these problem areas, the later sessions are used to help the patient develop strategies to deal with the problem area. In final sessions there is a focus on terminating weekly therapy. Techniques used to explore and change functioning include communication analysis, problem-solving, affective exploration and role-play.
Therapists
The five therapists in the study were psychiatrists, senior registrars or clinical psychologists. Therapists had to have at least 2 years’ experience of working with people with depression as out-patients and had to treat at least two patients with both therapies, under supervision, to a satisfactory level of competence before they were deemed eligible to treat study patients.
Treatment integrity
Treatment integrity was monitored during the therapist training phase and the study itself. Adherence and competence were the two main constructs measured to ensure treatment integrity (Reference Waltz, Addis and KoernerWaltz et al, 1993). These measures ensured that the therapies were performed according to the treatment manuals, and that the therapies were distinctly different from each other, particularly since each therapist was conducting both forms of treatment. Adherence has four components which refer to the extent to which the therapist follows the psychotherapy protocol. These are the extent to which the techniques used are:
-
(a) unique to the treatment modality;
-
(b) essential but not unique;
-
(c) compatible but not necessary or unique;
-
(d) clearly proscribed (Reference Hill, O'Grady and ElkinHill et al, 1992).
The Collaborative Study Psychotherapy Rating Scale (CSPRS; Hollon et al, personal communication, 1984), which was developed specifically for use in the NIMH TDCRP to measure adherence, was used. The psychometric properties of the original 96-item version, which is able to distinguish between IPT, CBT and clinical management, have been described elsewhere (Hollon et al, personal communication, 1988). In our study the 96-item version was modified to distinguish distinguish between the two intervention therapies by omitting the 20 items pertinent to clinical management, reducing the scale to 76 items. Two postgraduate clinical psychology students were trained to use the CSPRS according to TDCRP recommendations (Reference Hill, O'Grady and ElkinHill et al, 1992). Analysis of CSPRS scores revealed that the therapists adhered to treatment protocols. Sessions were classified correctly 100% of the time and over 90% of these had strict adherence to protocol.
Competence refers to the extent to which the therapist responds appropriately to the patient's problems with strategies relevant to the form of psychotherapy, and the quality of these strategies. To assess competence, two scales were used. The Therapist Strategy Rating Form (Reference O'Malley, Foley and RounsavilleO'Malley et al, 1988) was used to rate competence in IPT and the Cognitive Therapy Scale (Reference Dobson, Dobson and ShawDobson et al, 1985) was used to rate competence in CBT. During training the supervisors each scored the competence scales according to the ‘red line’ concept, which is an average acceptable score achieved for each therapist during training (Reference Shaw, Williams and SpitzerShaw, 1984). This was subsequently used quantitatively to ensure competence was maintained during the study phase.
Supervision
Supervisors were highly experienced in both therapies. Group supervision was conducted throughout the training period and course of the study. During these sessions the therapists and supervisors of each treatment met fortnightly for 1.5–2 h. Supervision sessions followed similar formats for each therapy with an emphasis on treatment integrity. Specific difficulties encountered during therapy were addressed and general techniques practised. Each new case was formulated according to the type of therapy. In addition to the group supervision, individual supervision was conducted as required.
To ensure interrater reliability, the supervisors also rated randomly selected audiotapes from each therapist during the study on a monthly basis. All ratings had acceptable supervisor agreement of 1 point on either competency scale, and all were above the therapist's own predetermined ‘red line’.
Outcome variables
Outcome variables were defined a priori. The primary outcome variable was percentage improvement in MADRS score, which is a robust measure of change and allowed us to compare our findings with those of medication studies (Reference Mulder, Joyce and FramptonMulder et al, 2003). The secondary outcome variable was response, defined as a 60% or greater change in MADRS score, and the five tertiary variables were percentage improvement in HRSD score; percentage improvement in BDI–II score; percentage improvement in SCL–90 score; and numbers of patients achieving scores of 6 or below on HRSD, and/or 9 or below on the BDI–II.
Statistical methods
All analyses were performed on the intention-to-treat sample and the statisticians were unaware of therapy allocation. Pre-intervention demographic and clinical variables were compared between groups using independent t-tests, ω2 tests and (when frequencies were low) Fisher's exact test. The outcome change variables were compared between groups using independent t-tests and ω2 tests as appropriate. A multiple linear regression, using dummy variables for psychotherapy group, was used to test the hypothesis that pre-intervention severity and melancholia influenced the relative efficacy of the two interventions. This model included terms for the main effects of therapy, baseline severity and melancholia and the two interaction terms severity×therapy and melancholia×therapy. The study was powered to show a 15% difference in improvement on the MADRS, as this level was considered a minimum clinically significant effect. A sample size of at least 85 in each therapy group provided more than 90% power to detect this difference as statistically significant (two-tailed α=0.05) assuming a within-group standard deviation of 30%.
RESULTS
Of the 282 patients screened by telephone for eligibility, 105 were excluded for the following reasons: 35 declined therapy in the study, 11 were treated with antidepressants as a preferred option, 46 did not meet inclusion criteria and 13 did not attend for the assessment interview. Of the 177 patients randomised, 91 patients were randomised to IPT and 86 to CBT. Of the 91 patients randomised to IPT, 8 (9%) did not complete the minimum number of weekly sessions of therapy. Of the 86 patients randomised to CBT, 10 (12%) did not complete the minimum number of weekly sessions of therapy. Of the 18 patients who did not complete at least eight sessions of weekly therapy, 11 withdrew or were lost to follow up (4 IPT, 7 CBT) and 7 began antidepressant medication during therapy (4 IPT, 3 CBT).
At the end of these weekly sessions 9 patients who received IPT and 5 who received CBT commenced taking antidepressant medication owing to lack of improvement. This resulted in 74 medication-free patients commencing monthly maintenance IPT and 71 such patients commencing monthly maintenance CBT (Fig. 1). The mean number of weekly sessions was 13, ranging from 8 to 19. Of the five therapists, two psychiatrists treated 39 patients each (one 21 IPT and 18 CBT, the other 26 IPT and 13 CBT), two clinical psychologists treated 45 patients each (one 22 IPT and 23 CBT, the other 18 IPT and 27 CBT), and one clinical psychologist joined the study late and treated 9 patients (4 IPT and 5 CBT).
Table 1 presents the baseline demographic and clinical characteristics of those randomised to each therapy. The two groups are comparable in gender, age, baseline depression severity and Axis I lifetime comorbid diagnoses. The groups are also generally comparable in terms of depression specifiers, although the CBT group included 80% with recurrent depression compared with 65% in the IPT group (ω2=5.24, P=0.022). Although the finding is not statistically significant, 16% of those randomised to IPT, compared with 24% of those randomised to CBT, were classified as severely depressed, based upon a previously defined cut-off score of 30 or more on the MADRS (Reference Muller, Himmerich and KienzleMuller et al, 2003).
Table 1 Baseline characteristics of the two therapy groups.

| IPT (n=91) | CBT (n=86) | ||
|---|---|---|---|
| Female gender, % | 76 | 69 | χ2=1.15, NS |
| Age, years: mean (s.d.) | 35.2 (10.5) | 35.2 (10.0) | t=0.01, NS |
| Depression severity score, mean (s.d.) | |||
| MADRS | 23.3 (6.5) | 24.4 (6.2) | t=1.13, NS |
| HRSD | 16.0 (4.7) | 16.7 (4.6) | t=0.99, NS |
| BDI | 27.7 (9.4) | 28.7 (10.4) | t=0.65, NS |
| SCL—90 total | 1.17 (0.57) | 1.27 (0.61) | t=1.13, NS |
| Lifetime comorbidity, n (%) | |||
| Alcohol dependence | 19 (21) | 20 (23) | χ2=0.15, NS |
| Cannabis dependence | 13 (14) | 15 (17) | χ2=0.33, NS |
| Panic disorder | 11 (12) | 16 (19) | χ2=1.45, NS |
| Social phobia | 21 (23) | 22 (26) | χ2=0.15, NS |
| Specific phobia | 15 (16) | 12 (14) | χ2=0.22, NS |
| OCD | 2 (2) | 6 (7) | Fisher's P, NS |
| Anorexia nervosa | 7 (8) | 3 (3) | Fisher's P, NS |
| Bulimia nervosa | 8 (9) | 6 (7) | χ2=0.20, NS |
| Depression specifiers, n (%) | |||
| Severe (MADRS ≥ 30) | 15 (16) | 21 (24) | χ2=1.72, NS |
| Melancholic | 34 (37) | 34 (39) | χ2=0.09, NS |
| Atypical | 26 (29) | 20 (23) | χ2=0.66, NS |
| Chronic | 59 (65) | 60 (70) | χ2=0.49, NS |
| Bipolar II | 3 (3) | 3 (3) | Fisher's P, NS |
| Recurrent | 59 (65) | 69 (80) | χ2=5.24, P=0.022 |
Table 2 presents the primary and secondary outcomes for each therapy. A total of 159 patients (90%) completed at least eight sessions of weekly therapy, and 145 (82%) remained medication-free and commenced monthly maintenance therapy. On the primary outcome measure of percentage improvement on the MADRS there was no statistically significant difference between the two therapies (P=0.059). Overall improvement in depressive symptoms was about 55%. The difference between the two therapies was further examined using analysis of covariance to control for baseline severity; this was also not statistically significant (P=0.055). With a 9.5% mean difference in outcomes between therapies, the 95% confidence interval is -3.8% to 19.2%. If a 15% difference in outcomes between therapies is considered clinically significant, then with sample sizes of greater than 85 per group we had a 90% power to detect such a difference.
Table 2 Primary and secondary outcomes by therapy in the intention-to-treat sample

| IPT (n=91) | CBT (n=86) | ||
|---|---|---|---|
| Participants completing therapy, n (%) | 83 (91) | 76 (88) | χ2=0.39, NS |
| Participants commencing maintenance phase, n (%) | 74 (81) | 71 (83) | χ2=0.05, NS |
| MADRS score: mean (s.d.) | |||
| Baseline | 23.3 (6.5) | 24.4 (6.2) | t=1.13, NS |
| Final | 12.6 (9.6) | 10.5 (9.4) | t=1.44, NS |
| Primary outcome | |||
| Improvement in MADRS score, % (s.d.) | 49.5 (32.9) | 58.9 (33.0) | t=1.90, 0.059 |
| Secondary outcome | |||
| Responders, n (%) | 41 (45) | 51 (59) | χ2=3.60, P=0.058 |
On the secondary outcome measure, a categorical outcome of a 60% or greater improvement in MADRS score, there was again no statistically significant difference between therapies, with 92 (52%) being defined as responders. The 95% confidence interval on the 14% difference in response rate is –3.2% to 28.8%. Analysis of outcome was also performed using the five tertiary measures. Outcome was significantly better (P=0.046) in the group receiving CBT using percentage improvement in HRSD scores. However, HRSD categorical response was not significant. Neither dimensional nor categorical outcomes measured by BDI–II were significant and there was no difference using the dimensional change in SCL–90 scores (Table 3).
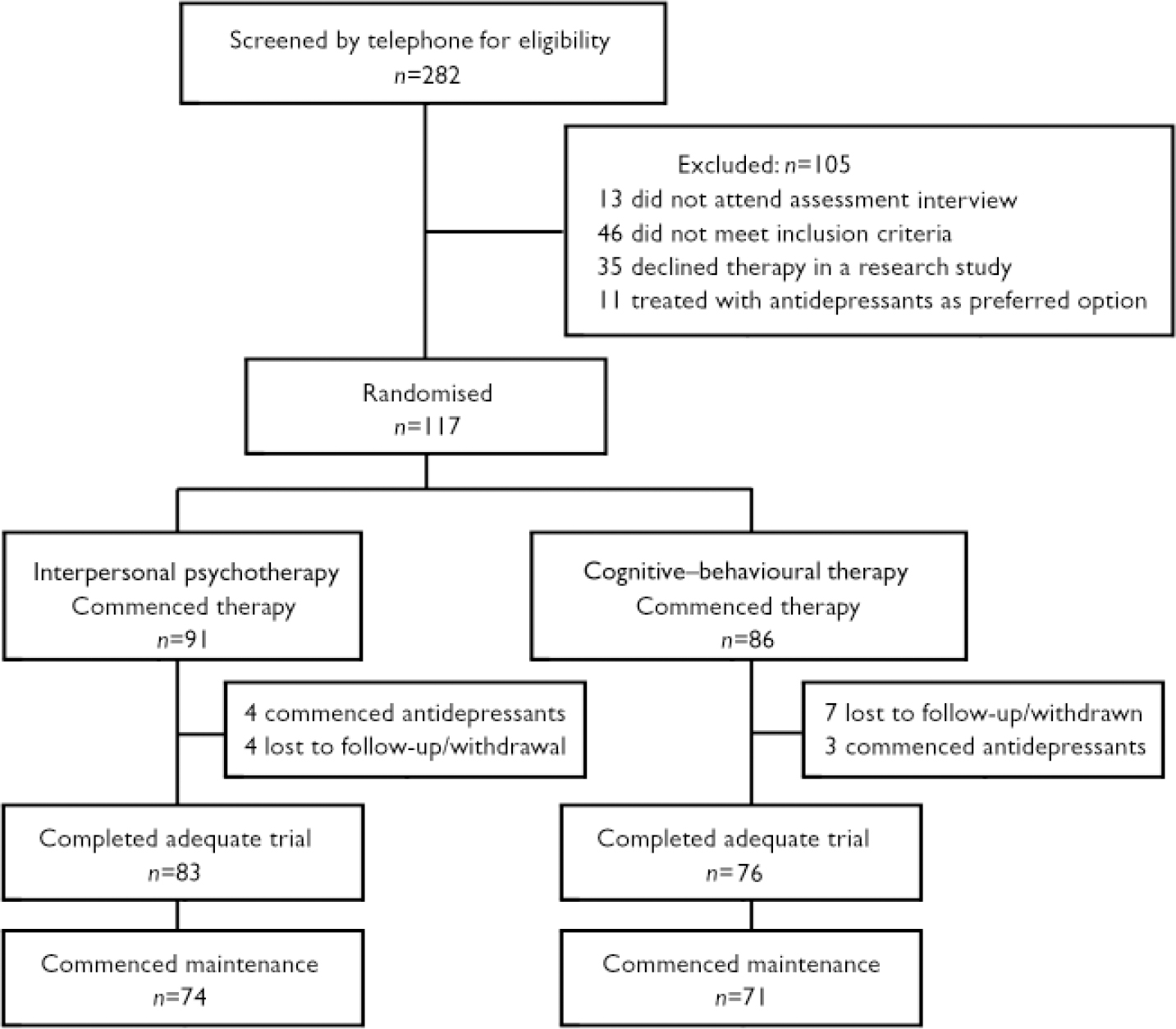
Fig. 1 Study profile.
Table 3 Tertiary outcomes by therapy using intention-to-treat sample

| IPT (n=91) | CBT (n=86) | ||
|---|---|---|---|
| HRSD | |||
| Baseline score: mean (s.d.) | 16.0 (4.7) | 16.7 (4.6) | t=0.99, NS |
| Final score: mean (s.d.) | 9.1 (7.0) | 7.6 (6.8) | t=1.48, NS |
| Improvement, % (s.d.) | 47.8 (34.0) | 58.0 (34.0) | t=2.01, P=0.046 |
| Patients with final score ≤ 6, n (%) | 40 (44) | 45 (52) | χ2=1.24, NS |
| BDI—II | |||
| Baseline score: mean (s.d.) | 27.7 (9.4) | 28.7 (10.4) | t=0.65, NS |
| Final score: mean (s.d.) | 17.1 (12.9) | 14.8 (12.4) | t=1.24, NS |
| Improvement, % (s.d.) | 42.3 (31.8) | 51.2 (34.2) | t=1.81, NS |
| Patients with final score ≤ 9 | 31 (34) | 37 (43) | χ2=1.50, NS |
| SCL—90 total score | |||
| Baseline: mean (s.d.) | 1.17 (0.57) | 1.27 (0.61) | t=1.13, NS |
| Final: mean (s.d.) | 0.72 (0.59) | 0.66 (0.60) | t=0.78, NS |
| Improvement, % (s.d.) | 43.4 (31.0) | 50.8 (34.8) | t=1.50, NS |
Table 4 shows the mean percentage improvement on the MADRS predicted by psychotherapy, severity and melancholia. Table 5 presents a multiple linear regression analysis of variables contributing to outcome. When percentage improvement is predicted from these variables severity × psychotherapy is a significant predictor (F=4.28, P=0.040) – i.e. IPT is less effective in severe depression. Notably, neither melancholia nor melancholia×psychotherapy predicted poor response to treatment.
Table 4 Impact of baseline depression severity and melancholia on final Montgomery—Åsberg Depression Rating Scale scores, by psychotherapy

| Final MADRS score, mean (s.d.) | ||
|---|---|---|
| Baseline depression | IPT | CBT |
| Severe depression1 | 35.3 (27.4) (n=15) | 62.6 (31.7) (n=21) |
| Mild to moderate depression | 52.3 (33.4) (n=76) | 57.8 (33.6) (n=65) |
| Melancholic | 54.6 (32.5) (n=34) | 60.4 (31.0) (n=34) |
| Non-melancholic | 46.5 (33.1) (n=57) | 58.0 (34.6) (n=52) |
Table 5 Multiple linear regression predicting percentage improvement using psychotherapy, baseline severity and melancholia

| F | P | |
|---|---|---|
| Psychotherapy | 7.01 | 0.009 |
| Severity | 1.77 | 0.185 |
| Melancholia | 2.09 | 0.150 |
| Severity × psychotherapy | 4.28 | 0.040 |
| Melancholia × psychotherapy | 0.99 | 0.322 |
Table 6 presents a comparison between our findings and the NIMH TDCRP findings. Since the TDCRP required higher HRSD scores for inclusion (≥14), we included only those patients who reached this cut-off point in our analysis. The TDCRP did not use MADRS scores thus comparisons are presented for our tertiary measures only. It is of note that we had slightly more patients than the TDCRP (128 v. 120) and a greater number of completers (116 v. 84), i.e. fewer withdrawals from the study, although the TDCRP required patients to attend more sessions to be deemed a completer (13 v. 8). Categorised by therapy, we had fewer withdrawals from our CBT group (n=6; 9%) than the TDCRP (n= 22; 37%). If we compare HRSD scores between studies, at baseline we had slightly lower mean scores but similar end-of-therapy scores were similar, although our patients who received CBT achieved much lower final scores (i.e. were the less depressed group at outcome). We were unable to compare our percentage of improvement in HRSD score, since the TDCRP used adjusted treatment scores. If we compare scores by the TDCRP definition of recovery (HRSD score of 6 or below), more of our CBT patients and fewer of our IPT patients achieved this. We cannot make direct comparisons between the BDI scores in each study since the TDCRP used the original version of this measure, which differs in scoring from the BDI–II, but scores are presented for interest.
Table 6 Comparison with outcomes of the National Institute of Mental Health Treatment of Depression Collaborative Research Program

| Christchurch study1 | TDCRP | |||
|---|---|---|---|---|
| IPT (n=63) | CBT (n=65) | IPT (n=61) | CBT (n=59) | |
| Patients completing trial, n (%) | 57 (90) | 59 (91) | 47 (77) | 37 (63) |
| Intention-to-treat sample | ||||
| HRSD | ||||
| Baseline score, mean (s.d.) | 18.4 (3.3) | 18.7 (3.2) | 19.6 (4.6) | 19.6 (3.9) |
| Termination score, mean (s.d.) | 10.7 (7.1) | 7.9 (6.4) | 9.8 (7.9) | 10.7 (7.9) |
| Improvement, % (s.d.) | 44.7 (31.5) | 58.1 (31.9) | ||
| Patients with final HRSD ≤ 6, n (%) | 21 (33) | 31 (48) | 26 (43) | 21 (36) |
| BDI/BDI—II2 | ||||
| Baseline score, mean (s.d.) | 30.2 (8.8) | 31.5 (9.4) | 26.0 (7.8) | 27.0 (7.9) |
| Termination score, mean (s.d.) | 19.9 (13.0) | 15.3 (11.6) | 12.0 (10.6) | 13.4 (10.6) |
| Improvement | 37.8 (28.9) | 52.1 (31.2) | ||
| Patients with final BDI/BDI—II score ≤ 9, n (%) | 17 (27) | 24 (37) | 34 (56) | 29 (49) |
DISCUSSION
This paper reports no significant difference in efficacy of IPT and CBT for depression, and although those receiving the latter therapy had a slightly higher response this was not significant. The overall improvement in depressive symptoms is about 55% in each group and about 55% of patients responded to therapy, based on a 60% or greater improvement in their MADRS scores over 16 weeks of therapy. Our results are consistent with the evidence that IPT and CBT are comparably effective therapies for people receiving out-patient treatment for major depression (Reference BeckhamBeckham, 1990; Reference Jarrett and RushJarrett & Rush, 1994; Reference Persons, Thase and Crits–ChristophPersons et al, 1996).
Psychotherapy for severe depression
Our hypothesis was that neither of the two psychotherapies would be particularly effective in participants with severe depression. Using a baseline MADRS score of 30 or more to categorise severe depression (Reference Muller, Himmerich and KienzleMuller et al, 2003), which is more stringent than cut-off points of 20 on the HRSD or 30 on the BDI–II, we have reported that CBT is significantly superior to IPT in this subgroup. Although the level of severity we chose may be on the lower end of a clinician's experience of depression, we were unable to explore outcome for those with higher MADRS scores since numbers were too small. Despite the ‘severe’ subgroup being only 20% (n=36) of our sample, those receiving CBT had a better outcome than those receiving IPT on both our primary dimensional outcome variable of percentage improvement and our secondary categorical outcome variable of response. Only 20% of patients with severe depression responded to IPT, whereas 57% of patients with severe depression responded to CBT. Furthermore, this response rate of 57% to CBT in severe depression compares favourably with the response to either type of therapy in mild or moderate depression. Our study therefore adds important data to the use of psychotherapy in severe depression. Our results contradict the findings of Elkin et al (Reference Elkin, Shea and Watkins1989), but are consistent with reviews by McLean & Taylor (Reference McLean and Taylor1992), Shapiro et al (Reference Shapiro, Barkham and Rees1994) and DeRubeis et al (Reference DeRubeis, Gelfand and Tang1999), and do not support the use of IPT for severe depression. We speculate that in severe depression the early behavioural activation in CBT favours symptom resolution, whereas the early exploratory approach of IPT hinders such resolution.
Psychotherapy for melancholic depression
Although we predicted that patients with melancholic depression would respond poorly to psychotherapy, this subtype of depression was not associated with poor outcome. This result challenges the notion that such patients should be treated cautiously with psychological treatments and will only respond to medication (Reference Thase and FriedmanThase & Friedman, 1999). It should be noted that our participants with melancholia were out-patients; in-patients might have had a different outcome. Our findings certainly raise the possibility that patients with melancholia can benefit from CBT and IPT.
Strengths and weaknesses of the study
This was an out-patient study, so to continue receiving psychotherapy patients had to be willing and motivated, which might bias our findings for patients with melancholia and severe depression. It is possible that our therapists were particularly experienced, and the supervisory process allowed for support and encouragement in managing difficult aspects of therapy which contributed to the positive outcome in these patients.
This is the largest trial ever conducted comparing these two psychotherapies for depression. The trial was conducted within a university-based out-patient clinical research unit, and patients were not sought by advertising. Despite the relatively young age of the sample, over two-thirds had chronic (i.e. more than 2 years of depression in the past 5 years) and/or recurrent depression. Our clinical research unit has previously undertaken trials of antidepressant medication (Joyce et al, Reference Joyce, Mulder and Cloninger1994, Reference Joyce, Mulder and Luty2002), but during this psychotherapy trial we were not simultaneously involved in any antidepressant studies so that there was no inclination to exclude severely depressed patients from this study and enter them into an antidepressant trial. During the trial only seven patients were prescribed antidepressants, which indicates a willingness, but seldom a need, to use these as alternative therapy. Conversely, we did not require a minimum score on the MADRS or HRSD for entry into the study, just that patients met DSM–IV criteria for a major depressive episode. Thus, we have included milder cases of depression, which were typically excluded from earlier studies such as the TDCRP. We therefore have the full range of out-patient depression severity within our sample.
During this study just five therapists in a single setting undertook all the therapy. Two were psychiatrists and three were clinical psychologists. The two psychiatrists commenced with prior training in – and thus possible ‘allegiance’ to – IPT, and required training in CBT; the three clinical psychologists began with prior training in – and thus possible ‘allegiance’ to – CBT and required training in IPT. When outcomes were examined according to therapist, there was no significant outcome effect due to therapist, professional training or prior experience of each therapy. The fact that the therapists were required to deliver both therapies, and had supervision to ensure that they were adhering to the specific therapy, argues against therapist effects having influenced our results.
In conclusion, IPT and CBT were comparable short-term out-patient psychotherapies for major depression, despite each having different models and techniques. Cognitive–behavioural therapy was superior in patients with severe depression, and this is further evidence that this therapy (but not IPT) might be a reasonable first-line treatment option for severe depression. It is noteworthy that patients with melancholia responded equally well to both psychotherapies. This suggests that patients with melancholia who want psychotherapy should not be denied it, as it is a potentially effective treatment option.
Acknowledgements
This research was funded by grants from the Health Research Council of New Zealand. We thank Robyn Abbott, Isobel Stevens and Andrea Bartram for help with patient care and data management. Thanks also to the therapists, trainers and supervisors: Dr Janet Carter, Dr Sue Luty, Dr Jenny Jordan, Dr Alma Rae, Ms Jenny Wilson, Ms Eileen Britt, Dr Jan McKenzie and Dr Gini McIntosh.










eLetters
No eLetters have been published for this article.