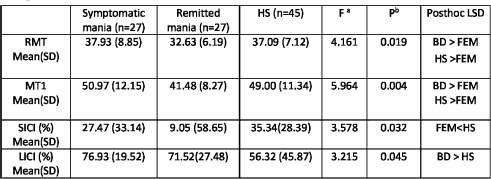
Table 1 Measures of motor threshold and CI across the three groups.
aDegrees of freedom 2,96.
bProbability error for the omni-bus test.
Published online by Cambridge University Press: 23 March 2020
Cortical inhibition (CI) is a neurophysiological outcome of the interaction between GABA inhibitory interneurons and other excitatory neurons. Transcranial magnetic stimulation (TMS) measures of CI deficits have been documented in both symptomatic and remitted bipolar disorder (BD) suggesting it could be a trait marker. The effects of medications and duration of illness may contribute to these findings.
To study CI in BD.
To compare CI across early-course medication-naive BD-mania, remitted first episode mania (FEM) and healthy subjects (HS).
Symptomatic BD subjects having < 3 episodes, currently in mania and medication-naive (n = 27), remitted FEM (n = 27; YMRS < 12 and HDRS < 8) and 45 HS, matched for age and gender, were investigated. Resting motor threshold (RMT) and 1-millivolt motor threshold (MT1) were estimated from the right first dorsal interosseous muscle. Paired-pulse TMS measures of short (SICI; 3ms) and long interval intracortical inhibition (LICI; 100ms) were acquired. Group differences in measures of CI were examined using ANOVA.
Symptomatic mania patients had the highest motor thresholds and the maximum LICI indicating a state of an excessive GABA-B neurotransmitter tone. Remitted mania patients had deficits in SICI indicating reduced GABA-A neurotransmitter tone. Putative changes in GABA-A neurotransmitter system activity with treatment may be investigated in future studies. CI has received less attention in BD as compared to schizophrenia and is a potential avenue for future research in this area.
The authors have not supplied their declaration of competing interest.
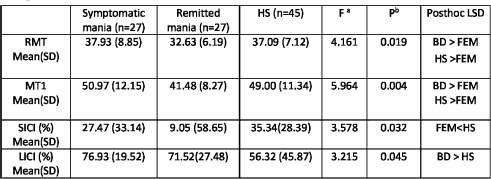
Table 1 Measures of motor threshold and CI across the three groups.
aDegrees of freedom 2,96.
bProbability error for the omni-bus test.

Table 1 Measures of motor threshold and CI across the three groups.aDegrees of freedom 2,96.bProbability error for the omni-bus test.
Comments
No Comments have been published for this article.