Dear Sirs,
We have read with interest the paper ‘Differentiation between cholesteatoma and inflammatory process of the middle ear, based on contrast-enhanced computed tomography imaging’ by A Trojanowska et al. Reference Trojanowska, Trojanowski, Olszanski, Klatka and Drop1 Numerous articles have demonstrated the strength of magnetic resonance imaging (MRI) – including delayed post-gadolinium T1-weighted imagesReference Williams, Ayache, Alberti, Heran, Lafitte and Elmaleh-Berges2 and/or echo-planar diffusion-weighted images in demonstrating middle-ear cholesteatoma.Reference Vercruysse, De Foer, Pouillon, Somers, Casselman and Offeciers3 In an era of increasing interest in reducing patient irradiation, it is puzzling to see that the 17 selected patients had three consecutive computed tomography (CT) scans for the demonstration of a residual or recurrent cholesteatoma, without approval by an ethical committee. Recently, the strength of echo-planar diffusion-weighted images in the diagnosis of acquired middle-ear cholesteatoma has been described.Reference Vercruysse, De Foer, Pouillon, Somers, Casselman and Offeciers3 However, the value of echo-planar diffusion-weighted images remains limited in the diagnosis of pre-second-look residual cholesteatoma, due to the often very small size of these residual cholesteatomas.Reference Vercruysse, De Foer, Pouillon, Somers, Casselman and Offeciers3 The size limit for detection of middle-ear cholesteatoma in this paper has been set on 5 mm. Moreover, recent reports have highlighted the additional value of non-echo-planar diffusion-weighted sequences in the demonstration of middle-ear cholesteatoma.Reference Dubrulle, Souillard, Chechin, Vaneeclo, Desaulty and Vincent4, Reference De Foer, Vercruysse, Pilet, Michiels, Vertriest and Pouillon5 Non-echo-planar diffusion-weighted images sequences are able to demonstrate cholesteatoma with a size limit of 5 mm.Reference Dubrulle, Souillard, Chechin, Vaneeclo, Desaulty and Vincent4 We reported our preliminary findings on a new non-echo-planar diffusion-weighted images sequence with a higher resolution and a complete lack of artifacts, which look very promising for demonstration of middle-ear cholesteatoma.Reference De Foer, Vercruysse, Pilet, Michiels, Vertriest and Pouillon5 The most challenging task for radiologists still remains the differentiation of a completely opacified mastoidectomy cavity. We would like to illustrate the strength of this new non-echo-planar diffusion-weighted images sequence and its value compared to CT in two cases (three ears).
Case one: A 56-year-old male with prior surgery for cholesteatoma on the left side presented for pre-second-look evaluation. On axial high resolution CT, it is virtually impossible to differentiate the entirely opacified middle ear (Figure 1) and mastoidectomy cavity (Figure 2). On late post-gadolinium enhanced T1-weighted image a hypointense non enhancing tissue in the middle ear was laterally delineated by the enhancing tympanic membrane (Figure 3). A clear hyperintense aspect of the middle ear was seen on T2-weighted images. On the axial late post-gadolinium enhanced T1-weighted image a completely enhancing mastoidectomy cavity was seen (Figure 4). The coronal non-echo-planar diffusion-weighted images revealed a complete lack of hyperintensity, excluding the presence of a cholesteatoma (Figure 5). At surgery, glue was found in the middle ear and scar and granulation tissue was found in the mastoidectomy cavity. The presence of glue explains the non-enhancement of the material in the middle ear. On standard MRI sequences as well as on CT – even enhanced – this lesion can easily be misdiagnosed as a cholesteatoma due to the lack of enhancement. In this case, only the non-echo-planar diffusion-weighted images gave the solution, excluding the presence of cholesteatoma.

Fig. 1 Case one: axial high resolution CT: it is virtually impossible to differentiate the entirely opacified middle ear (arrow).

Fig. 2 Case one: axial high resolution CT: it is virtually impossible to differentiate the mastoidectomy cavity (asterisk).

Fig. 3 Case one: late post gadolinium enhanced T1-weighted image showing hypointense non-enhancing tissue in the middle ear, laterally delineated by the enhancing tympanic membrane (arrow).

Fig. 4 Case one: axial late post-gadolinium enhanced T1-weighted image showing a completely enhancing mastoidectomy cavity (arrows).
Fig. 5 Case one: The coronal non-echo-planar diffusion-weighted images revealing a complete lack of hyperintensity, excluding the presence of a cholesteatoma.
Case two: A 40-year-old female with prior surgery for cholesteatoma on the right side four years ago and on the left side one years ago. Axial CT shows a modified radical mastoidectomy on the right side with irregular peripheral soft tissue density, anterior to the sigmoid plate (Figure 6). The coronal non-echo-planar diffusion-weighted images sequence clearly shows an oval 0.9 cm large hyperintensity in the flow void region of the right temporal bone (Figure 7). It corresponds to a non-enhancing recurrent cholesteatoma just anterior to the sigmoid sinus on the late post-gadolinium T1-weighted MR image (Figure 8). There was a lot of enhancing inflammatory tissue around the cholesteatoma. Surprisingly, a small nodular hyperintensity under the tegmen was found on the left side (Figure 7). On the late post-gadolinium T1-weighted coronal MR image a small nodular hypointensity was found (Figure 8), corresponding to a small nodular soft tissue density on CT, directly under the tegmen (Figure 9). MRI – both the non-echo-planar diffusion-weighted images and late post-gadolinium T1-weighted images – clearly demonstrated the 9 mm recurrent cholesteatoma on the right side and the 3 mm small residual cholesteatoma on the left side, whereas CT only clearly demonstrated the small residual cholesteatoma on the left side. In our current protocol we use a combination of a non-echo-planar diffusion-weighted images sequence and a late post-gadolinium T1-weighted sequence. We hope that this combination of sequences will be able to demonstrate small residual cholesteatomas pre-second-look as well as (larger) recurrent cholesteatomas in mastoidectomy cavities, avoiding the need for repetitive irradiating CT scans of the middle ear.

Fig. 6 Case two: axial CT showing a modified radical mastoidectomy on the right side with irregular peripheral soft tissue density (arrows), anterior to the sigmoid plate.

Fig. 7 Case two: the coronal non echo-planar diffusion-weighted images sequence clearly shows an oval 9 mm large hyperintensity (arrow) in the flow void region of the right temporal bone and a 3 mm small hyperintensity on the left side (arrow).
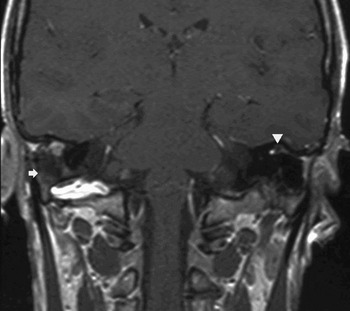
Fig. 8 Case two: late post-gadolinium T1-weighted MR image showing a non-enhancing recurrent cholesteatoma just anterior to the sigmoid sinus on the right side (arrow) and a small nodular hypointense residual cholesteatoma on the left side (arrow head) under the temporal lobe.

Fig. 9 Case two: CT scan showing small nodular soft tissue density directly under the tegmen (arrow).
Authors’ reply
The authors declined to make a response.


