Social cognition involves the perception, interpretation and processing of social information that underlies social interactions and includes emotion perception, social perception, social knowledge and attributional bias (Reference Penn, Addington, Pinkham, Lieberman, Stroup and PerkinsPenn et al, 2005a ). In this study we examine social knowledge and social perception. People with schizophrenia are less sensitive to interpersonal cues (social knowledge) (Reference Corrigan and GreenCorrigan & Green, 1993a ; Reference Corrigan, Garman and NelsonCorrigan et al, 1996b ; Reference CorriganCorrigan, 1997) and established difficulties in social perception have been associated with both poor social functioning (Reference Toomey, Wallace and CorriganToomey et al, 1997) and cognitive impairment (Reference Corrigan, Green and ToomeyCorrigan et al, 1994; Reference Sergi and GreenSergi & Green, 2002; Reference Vauth, Rusch and WirtzVauth et al, 2004; Reference Wynn, Sergi and DawsonWynn et al, 2005). Deficits in cognition have been associated with poor outcome in schizophrenia and may exert an influence on social functioning via social cognition outcome (Reference Penn, Bentall and CorriganPenn et al, 1997; Reference Vauth, Rusch and WirtzVauth et al, 2004; Reference Sergi, Rassovsky and NuechterleinSergi et al, 2006).
METHOD
Design
The purpose of this study was to test the hypotheses that (a) deficits in social perception were associated with deficits in social functioning and cognition and (b) that social perception mediated between cognitive and social functioning. A longitudinal design was used to determine the stability of social perception. The control group allowed us to ascertain whether the relationships between cognition, social cognition and functioning were affected by psychosis.
Participants
There were three groups of participants. The first comprised 50 people with first-episode psychosis (30 men, 20 women), consecutively admitted to the Calgary Early Psychosis Program, which serves an urban population of 930 000 (Reference Addington and Adding tonAddington & Addington, 2001). The participants had not received more than 3 months of adequate treatment previously (Reference Larsen, McGlashan and MoeLarsen et al, 1996). Exclusion criteria included a history of neurological disorders, head injury or epilepsy, or not speaking English well enough to adequately complete the assessments. The majority of the participants were single (88.0%), with a mean age of 25.1 years (s.d.=8.0), had completed grade 12 (66.0%), lived at home (78.0%), and were White (78.0%). At the time of the two assessments, 41 (82.0%) and 44 (87.5%), respectively, were reportedly taking second-generation antipsychotics (mean dose in chlorpromazine equivalents of 307 mg/day and 380 mg/day respectively). Diagnoses were completed at baseline and then repeated at 1 year; 1-year diagnoses were as follows: schizophrenia 32 participants (64.0%), schizophreniform 12 (24.0%), delusional disorder 1 (2.0%), brief psychotic disorder 1 (2.0%), psychotic disorder not otherwise specified 3 (6.0%) and schizoaffective disorder 1 (2.0%).
The second, multi-episode group consisted of 53 people (38 men, 15 women) who attended a specialised out-patient programme for schizophrenia in a psychiatry department of a general hospital. These had received a diagnosis of schizophrenia at least 3 years previously and had a chronic course of schizophrenia with on average five hospital admissions. The majority were single (41, 77.4%), with a mean age of 35.5 years (s.d.=7.2), had completed grade 12 (38, 71.7%), lived at home (24, 45.3%) and were White (49, 92.5%). At the time of both assessments, 52 (98.1%) were reportedly taking second-generation antipsychotics (mean dose in chlorpromazine equivalents of 715 mg/day and 665 mg/day respectively). They all met criteria for schizophrenia.
The third group of 55 local controls without psychiatric illness were matched for gender (33 men, 22 women), age (mean age 21.7 years, s.d.=6.1), and education (40, 72.7% completed high school) to the first-episode sample. Structured Clinical Interview for DSM–IV (SCID; Reference Spitzer, Williams and GibbonSpitzer et al, 1992) criteria were used to exclude current or past psychiatric disorder.
Measures
Social perception
The ability to understand and appraise social roles, rules and context was assessed by the Social Cue Recognition Test (SCRT; Reference CorriganCorrigan, 1997). This requires individuals to use social cues to make inferences about the situational events that generated the particular social cue or to identify interpersonal features in a given situation. The SCRT consists of eight videotaped 2- to 3-min vignettes of 2–3 people talking (e.g. friends gossiping while assembling a puzzle, a husband and wife arguing about their children). Participants watch each scene and then answer 36 true-or-false questions per vignette about the presence of concrete cues (i.e. what the actor said and did) and abstract cues (i.e. inferences about the rules, affect and goals guiding the actors’ behaviours). Two indices are determined for each condition: correct identification rate (number of items the participant judged to be true that were in fact true, divided by total possible true items) and false-positive rate (number of items the participant judged to be true that were in fact false, divided by total possible false positives). Correct identification and false-positive rates representing abstract and concrete cue recognition have been matched for item difficulty and consistency on standardisation and cross-validation samples of healthy controls (Reference CorriganCorrigan, 1997). The validity of the abstract–concrete dimension represented by SCRT items has been examined in a separate study (Reference Corrigan, Buican and ToomeyCorrigan et al, 1996a ; Reference Corrigan and NelsonCorrigan & Nelson, 1998). We generated three scores for this task: a score for concrete cues, a score for abstract cues and an overall score.
Social knowledge
Awareness of rules, goals and the roles that characterise social situations in order to identify social cues (Reference Corrigan and GreenCorrigan & Green, 1993a ) was assessed with the Situational Features Recognition Test (SFRT; Corrigan et al, Reference Corrigan, Buican and Toomey1996a ,Reference Corrigan, Garman and Nelson b ). The SFRT is a paper-and-pencil measure that requires participants to identify features from a list of descriptors that describe five familiar situations (e.g. taking a test, reading in a library, driving a car) and four unfamiliar situations (e.g. building an igloo, performing surgery). Participants are presented with a list of features for each situation, corresponding to actions, roles, rules and goals. Each list includes six features and eight distracters. The SFRT has been shown to have good psychometric properties (Reference CorriganCorrigan, 1997). The validity of the abstract–concrete dimension represented by SFRT items has been examined in a separate study (Reference Corrigan, Buican and ToomeyCorrigan et al, 1996a ). This task generated two scores: one for concrete features and one for abstract features, since those with schizophrenia are less sensitive to the more abstract features such as goals than to the concrete features such as actions or rules (Reference Corrigan and GreenCorrigan & Green, 1993b ; Reference Corrigan, Garman and NelsonCorrigan et al, 1996b ).
The battery used for the assessment of cognitive functioning has been well described elsewhere (Reference Addington, Saeedi and AddingtonAddington et al, 2005) and includes: letter fluency (Controlled Oral Word Association Test; COWAT; Reference Benton and HamsherBenton & Hamsher, 1983); category fluency (category instances; Reference Tombaugh, Kozak and ReesTombaugh et al, 1999); verbal memory (logical memory sub-tests of the Wechsler Memory Scale – Revised, LMI, LMII; Reference WechslerWechsler, 1987); Rey Auditory Verbal Learning Test, (RAVLT; Reference LezakLezak, 1995); visual memory (Rey Complex Figure Test; Reference ReyRey, 1958); working memory (letter–number span; Reference Gold, Carpenter and RandolphGold et al, 1997), Wisconsin Card Sorting Test (WCST; Reference HeatonHeaton, 1981); attention degraded stimulus continuous performance test (DS–CPT; Reference Nuechterlein, Steinhauer, Gruzelier and ZubinNuechterlein, 1991); early information processing or span of apprehension (SPAN; Reference Asarnow, Granholm, Sherman, Steinhauer, Gruzelier and ZubinAsarnow et al, 1991); visual–constructional ability (copy of the Rey Complex Figure); visuomotor sequencing (trails A and trails B; Reitan & Wolfson, 1998); psychomotor speed (grooved pegboard; Reference Mathews and KloveMathews & Klove, 1964); and the Stroop task (Reference GoldenGolden, 1978).
Social functioning was assessed by two measures: the Quality of Life Scale (QLS; Reference Heinrichs, Hanlon and CarpenterHeinrichs et al, 1984), which is a widely used interviewer-rated scale of social, interpersonal and role functioning; and a measure of social problem-solving, the Assessment of Interpersonal Problem Solving (AIPPS; Reference Donahoe, Carter and BloemDonahoe et al, 1990). The AIPPS is a videotaped vignette test used to assess the social skills of people with schizophrenia. The test measures a person's ability to describe an interpersonal social problem, to derive a solution to the problem and to enact a solution in a roleplayed simulation test. This analysis implies a problem-solving model of social skills. First, recognising the existence of a problem requires skills of problem identification. The ability to describe both the goal and the obstacle is problem description. Together, problem identification and problem description are called receiving skills. Second, various alternatives must be identified, the consequences considered and the best alternative chosen. These are processing skills. Third, the solution has to be enacted. Sending skills consist of content skills and performance skills. The constructs measured by the instrument are operationally defined as receiving–processing–sending (RPS) skills (Reference Donahoe, Carter and BloemDonahoe et al, 1990).
The AIPPS has been shown to have adequate psychometric properties (Reference Donahoe, Carter and BloemDonahoe et al, 1990). It consists of 13 short videotaped interactions. Ten interactions involve problems defined as one person preventing another from obtaining a desired goal (e.g. a waitress writes down an order incorrectly) and three present no problems (e.g. two friends enjoying a card game). Participants watch the videotape and are instructed to identify with one of the actors in each of the vignettes. After each vignette, participants are asked a series of questions about the scene from the perspective of this actor. ‘Is there a problem in the scene? What is the problem?’ (receiving skills); ‘What would you do about the problem?’ (processing skills). Participants are then asked to roleplay their response to the problem situation (sending skills); they become familiar with the AIPPS during a practice scene in which questions and role-play are demonstrated. Responses are recorded by the examiner and subsequently scored using a manual of correct responses. The AIPPS was scored using the specific scoring option, which means that if participants do not identify the existence of a problem they are only rated on items observed.
Symptoms were assessed with the Positive and Negative Syndrome Scale for Schizophrenia (PANSS; Reference Kay, Fiszbein and OplerKay et al, 1987).
Procedures
Formal consent was obtained from all participants. Testing of the control group took place in two sessions, usually on the same day. For the first-episode and multi-episode groups, the assessments were completed in three sessions within a 7-day period. All assessments were repeated 1 year later. All raters for the SCID, PANSS and QLS were experienced research clinicians who demonstrated adequate reliability at regular intervals. Cognitive and social perception tests were administered by trained psychometricians under the supervision of J.A. Independent raters completed the cognitive battery, the social perception tasks and the social functioning and were masked to the results of the other assessments. Participants were clinically stable at the time of each follow-up and did not present with acute psychotic symptoms.
Statistical analyses
Paired t-tests were used to assess change over time in all variables. One-way analyses of variance (ANOVAs) were used to compare groups on all variables. Principal components factor analysis was used to reduce cognitive data. To determine whether social cognition mediates the relationship between cognition and social functioning, a series of regression analyses were performed according to the method outlined by Baron & Kenny (Reference Baron and Kenny1986).
To establish mediation we use regression models and the following conditions.
-
(a) The independent variable (cognition) must correlate significantly with the mediator variable (social cognition).
-
(b) The mediator variable (social cognition) must correlate significantly with the dependent variable (social functioning).
-
(c) When the effects of the mediator are controlled for, a previously significant correlation between cognition and social functioning must be greatly attenuated (Reference Baron and KennyBaron & Kenny, 1986).
Perfect mediation is demonstrated if the independent variable (cognition) has no effect on the dependent variable (social functioning) when the effect of the mediator (social cognition) is controlled. Thus, if we have significant relationships between cognition, social cognition and social functioning, we can then perform the final test of examining the change (if any) in the relationship between cognition and social functioning after controlling for social perception (Fig. 1).
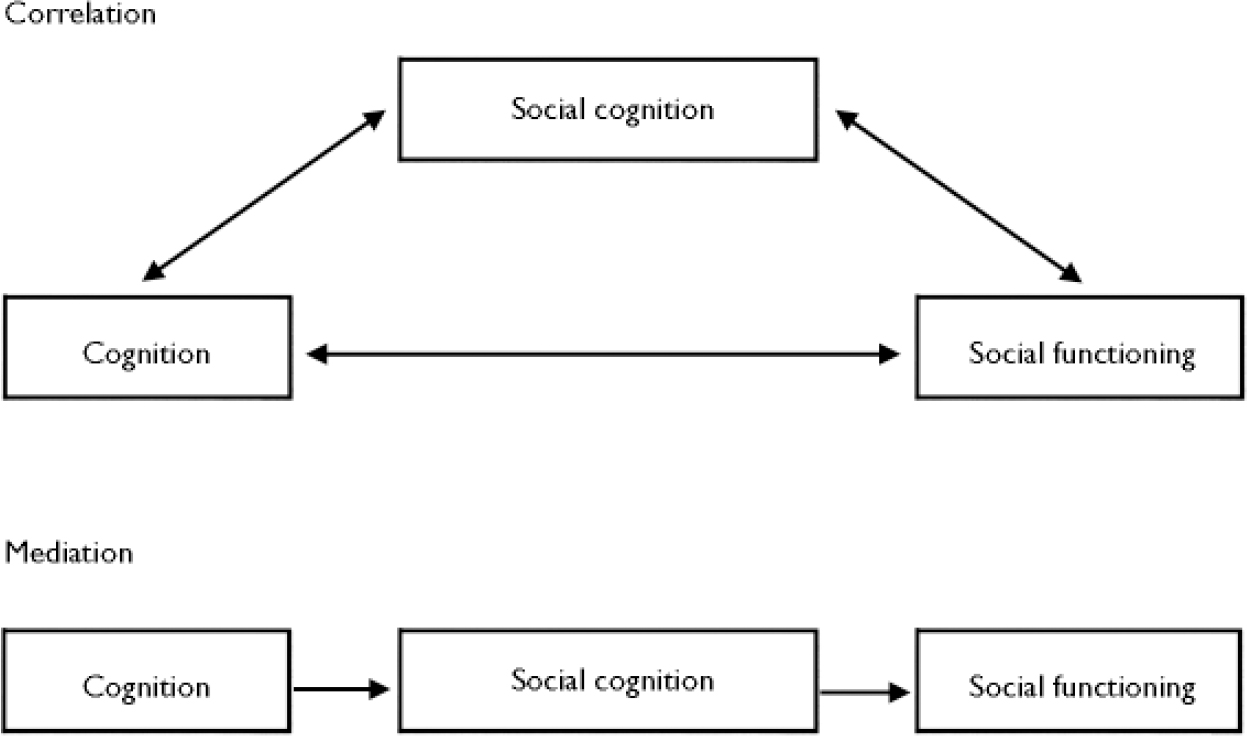
Fig. 1 Mediational model.
RESULTS
Data reduction
All three groups performed significantly better on the concrete component of the SFRT compared with the abstract component. Since this was not a significant advantage, we used just one overall score for the SCRT. We reduced the cognitive data with factor analyses. Using principal components analysis, we determined that the data were suitable for factor analysis (Bartlett's test was significant, P<0.0005, and the Kaiser–Meyer–Olkin index=0.80). There were six factors with eigenvalues greater than 1. The tests all loaded on one factor, with most of the variance being accounted for by the first factor. The factor analysis was then conducted forcing one factor. This finding of one factor replicates earlier studies with large samples with first-episode psychosis (Reference Keefe, Seidman and ChristensenKeefe et al, 2004; Reference Addington, Saeedi and AddingtonAddington et al, 2005).
Change over 1 year
Paired t-tests were used to assess change over time. There was no significant change in any of the social cognition measures for either the first-episode group or the multi-episode group over time. There was a significant improvement for the control group (SCRT: t=–3.13, P<0.01; SFRT (concrete): t=–4.04, P<0.0005). There was a significant improvement over time on the QLS for the first-episode group (t=–4.23, P<0.0001). This was concomitant with an improvement in positive symptoms for the first-episode group over time. There was minimal change over 1 year on the separate cognitive measures, but no change on the global cognitive factor. Measures were generally stable over time except for the QLS and positive symptoms in the first-episode group.
Group differences
One-way ANOVAs were used to compare groups on all variables. All three groups differed significantly on the QLS at baseline, with the controls having superior performance and the first-episode group being most compromised. By 1 year there were no differences between the two episodic groups, with the control group having superior performance. On the AIPPS at both assessments the controls had superior performance relative to both episodic groups. At baseline the first-episode group had more positive symptoms than the multi-episode group (t=3.87, P<0.0001), but this was reversed at 1 year (t=2.09, P<0.05). For the SCRT and the SFRT at both assessments there were no differences between the episodic groups, and significant differences between the episodic groups and the controls (F values ranged from 9.45 to 18.60, P<0.0001 for each model). Interestingly, the two tasks were highly associated in the episodic groups at both assessments but not in the controls (r values ranged from 0.51 to 0.73, P<0.0001). On all cognitive tasks the control group outperformed the episodic groups. This was also true for the cognitive factor at both assessments (F=36.6, P<0.0001; F=46.6, P<0.0001). Thus, since the episodic groups did not differ on any task, they were combined as a single patient group for all further analyses. In summary, the patient groups performed significantly more poorly than the control group on all tasks.
Mediation
In the patient group poor scores on all social cognition tasks were significantly associated with:
-
(a) positive and negative symptoms at both assessments (r values ranged from 0.27, P<0.01, to 0.38, P<0.0005);
-
(b) QLS at both times (r ranged from 0.25 to 0.39, P<0.01);
-
(c) AIPSS at both assessments (r ranged from 0.33, P<0.011, to 0.45, P<0.0005);
-
(d) the cognitive factor at both times (r ranged from 0.37 to 0.51, P<0.0005).
Furthermore, almost all of the individual cognitive tests were significantly associated with the social perception tasks.
In the control group there were very few significant correlations between the social cognition tasks and QLS and the AIPPS, suggesting that these may be occurring by chance because of multiple correlations. Correlations between social cognition and the cognitive factor were more consistent (r ranged from 0.33 to 0.42, P<0.01). In summary, for patient groups social cognition, cognition and social functioning were all intercorrelated. Similar trends were noted for the controls.
Since all of the above results held for both the SCRT and the SFRT tasks, we used transformed z-scores to combine these two tasks into a composite variable social perception. Results of the regression analyses for QLS as the dependent variable are presented in Table 1 and for the AIPPS in Table 2. There were significant associations between social perception, cognition and social functioning (QLS and AIPPS) at both assessments for the patient group. For the control group, at baseline the AIPPS was not associated with social perception or cognition and at 1 year the QLS was not associated with social perception. These results mean that we test for mediation on both measures at both times for the patient group and for the controls, at baseline for QLS and at 1 year for the AIPPS. For mediation we want to see in condition 3b in Tables 1 and 2 significant reductions in r 2 change and in the standard beta.
Table 1 Testing for mediation between the Quality of Life Scale (QLS) and cognition
| Patients at baseline | Patients at 1 year | Controls at baseline | Controls at 1 year | ||
| Condition 1: regress the mediator (social perception) on the independent variable (cognition) | |||||
| r=0.47**** | r=0.50**** | r=0.46** | r=0.48**** | ||
| Condition 2: regress the dependent variable (QLS) on the mediator (social perception) | |||||
| r=0.28** | r=0.39**** | r=0.47**** | r=0.17 | ||
| Condition 3a: regress the dependent variable (QLS) on the independent variable (cognition) | |||||
| r=0.27** | r=0.36**** | r=0.40** | r=0.44*** | ||
| Condition 3b: change in relationship between QLS (dependent variable) and cognition (independent variable) after controlling for social perception (mediator) | |||||
| r 2 change before and after controlling for social perception | Standard beta before and after controlling for social perception | ||||
| Patients at baseline | 0.07** | 0.02 | 0.27** | 0.18 | |
| Patients at 1 year | 0.13**** | 0.04* | 0.36**** | 0.22* | |
| Controls at baseline | 0.11** | 0.04 | 0.33** | 0.23* | |
Table 2 Testing for mediation between Assessment of Interpersonal Problem-Solving (AIPPS) and cognition
| Patients at baseline | Patients at 1 year | Controls at baseline | Controls at 1 year | ||
| Condition 1: regress the mediator (social perception) on the independent variable (cognition) | |||||
| r=0.47**** | r=0.50**** | r=0.46**** | r=0.48**** | ||
| Condition 2: regress the dependent variable (AIPPS) on the mediator (social perception) | |||||
| r=0.44**** | r=0.49**** | r=0.24 | r=0.30* | ||
| Condition 3a: regress the dependent variable (AIPPS) on the independent variable (cognition) | |||||
| r=0.33** | r=0.34**** | r=0.25 | r=0.31* | ||
| Condition 3b: change in relationship between AIPPS (dependent variable) and cognition (independent variable) after controlling for social perception (mediator) | |||||
| r 2 change before and after controlling for social perception | Standard beta before and after controlling for social perception | ||||
| Patients at baseline | 0.11** | 0.02 | 0.33** | 0.16 | |
| Patients at 1 year | 0.12**** | 0.02 | 0.34*** | 0.13 | |
| Controls at 1 year | 0.10* | 0.04 | 0.31* | 0.21 | |
In the first set of regressions, after controlling for social perception, cognition continued to have a very small significant effect on QLS for the patients at 1 year and for the controls at baseline. For the patient group, at baseline there was a small reduction in the effect of cognition on social functioning, suggesting partial mediation.
However, in the second set of regressions with the AIPPS as the dependent variable, there was a significant reduction in the effect of cognition on social problem-solving, particularly for the patient group. This suggests that social perception is a potential mediator between cognition and social problem-solving.
DISCUSSION
This is the first study to examine measures of social perception and social knowledge in an early psychosis sample, and to the best of our knowledge no previous study has examined these tasks longitudinally. This study supports previous research findings that, compared with healthy controls, people with schizophrenia have deficits in social knowledge and social perception. These deficits were evidenced to the same degree in both a sample of people presenting with a first episode of psychosis and in a sample of those with chronic schizophrenia. Furthermore, the deficits remained stable over time in both patient groups. Of particular note is that the deficits were stable in the first-episode group over the first year after admission to the early psychosis programme despite an improvement in positive symptoms. Previous studies have suggested that other measures of social cognition, such as facial affect recognition, may be deficit traits (Reference Kee, Green and MintzKee et al, 2003; Reference Kucharska-Pietura, David and MasiakKucharska-Pietura et al, 2005; Reference Addington, Saeedi and AddingtonAddington et al, 2006). An important implication of our results is that social cognition, in general, may be a stable deficit trait.
Our data also support a strong longitudinal association between the social cognition tasks and poor cognition in the three groups, which suggests cognitive underpinnings to social perception and social knowledge. In this study, social perception and social knowledge combined appeared to act as a mediator of the relationship between cognition and interpersonal problem-solving. However, for social functioning, as assessed by the QLS, there was only partial mediation for the patient group. Earlier correlational studies have only implied an indirect role for social cognition, in that it was related to both social functioning and cognitive functioning. The results of this study are consistent with an earlier study that examined the role of social perception in the relationship between an early visual processing task and social functioning (Reference Sergi, Rassovsky and NuechterleinSergi et al, 2006).
The limitations of this study are that the assessment of social functioning was restricted to one general measure of social functioning (QLS) and a laboratory-based measure of social problem-solving. There is no one way to measure social functioning and the range of measures may have given a more comprehensive assessment. However, we did see different patterns of mediation with the two different outcome measures, suggesting that although cognitive deficits may be rate-limiting in terms of outcome, there are many other factors such as educational and work opportunities, and other illness factors that contribute to poor ratings on a general measure of functioning. A second limitation is that we limited our assessment of social perception and social knowledge to one task for each.
The strengths of the study are first that we used both individuals with a first episode of psychosis and those with a more chronic course; second, it was a 1-year longitudinal study; and third, it used a control group longitudinally.
There are clinical implications, in that the recognition of the importance of social cognition has led to the development of interventions to specifically address social cognition. Targeted interventions can focus on a specific social cognitive ability, such as facial affect (Reference Silver, Goodman and KnollSilver et al, 2004). Alternatively interventions may be broad-based and as such include cognitive remediation (Reference Hogarty, Flesher and UlrichHogarty et al, 2004). One such intervention has been developed by Penn et al (Reference Penn, Roberts and Munt2005b ) focusing on key social cognitive domains such as emotion perception, attributional style and theory of mind. This approach includes work on facial affect recognition, cognitive–behavioural strategies and application of strategies to real-life situations.
Pilot data from this approach were positive, particularly with respect to the cognitive–behavioural components. Cognitive–behavioural therapy has been advocated for people with first-episode schizophrenia (Reference Addington and GleesonAddington & Gleeson, 2005) as well as those with a more chronic course of illness. Strategies that help individuals to define and identify emotions and cues more carefully rather than jumping to conclusions, to examine the veracity of delusional beliefs (e.g. reality-testing social cues), and to conduct behavioural experiments in the context of social cues and perceptions, may help improve social cognition.
In conclusion, this study adds to the evidence that cognition is important in determining outcome, and the exciting finding of potential mediators such as social cognition hold promise for both increasing our understanding of psychosis and improving our interventions, although the potential of such treatments is in the early stages of development. Furthermore, there is now a need to clearly define the relevant areas of social cognition, to refine the measures being used and to develop an agenda of research that includes both animal and human studies, as advocated by the MATRICS group (Measurement and Treatment Research to Improve Cognition in Schizophrenia; Reference Green, Olivier and CrawleyGreen et al, 2005).






eLetters
No eLetters have been published for this article.