Following the initial Wuhan outbreak in Hubei province, China, COVID-19 has rapidly diffused into a global pandemic. 1 Given the salience of human psychological and behavioral factors to disease prevention and mitigation, it is crucial to evaluate their role in propagating or impeding behavioral responses.Reference Bish and Michie 2 , Reference Wise, Zbozinek and Michelini 3 Many studies reported on mental and behavioral responses during an outbreak of an acute respiratory infection.Reference Li, Yang and Dou 4 ‒Reference LV and Yang 6 People quarantined at home or at another location may have experienced boredom, anger, and loneliness, which in turn elicited a personal behavioral response.Reference Severance, Dickerson and Viscidi 7 , Reference Yang 8 COVID-19 is a new disease, and the 2019 outbreak in Wuhan and elsewhere in China may have been stressful. An epidemic of a highly lethal disease can overwhelm people emotionally and physically and induce strong mental and behavioral responses in both adults and children.Reference Lunn, Belton and Lavin 5 , Reference Cullen, Gulati and Kelly 9 , Reference Greenberg, Docherty and Gnanapragasam 10
According to the Stimulus, Cognition and Response (SCR) model, various stimuli (S) affect internal states of people through cognition (C), which in turn elicits mental and behavioral responses (R).Reference Yang 8 , Reference Mehrabian and Russell 11 COVID-19 is a potent stimulus that plausibly induces people to perceive high risk of infection with potentially severe health consequences. Health belief theory proposes such perceptions may generate a behavioral response.Reference Yang 8 Some studies found an association between strong risk and threat perceptions and excess mental and behavioral problems during outbreaks of the severe acute respiratory syndrome (SARS) and Ebola.Reference Dorfan and Woody 12 ‒Reference Yang and Chu 14 A recent study revealed that individuals’ perceived severity of the COVID-19 epidemic was related to undesirable emotional and behavioral outcomes among the Chinese public.Reference Li, Yang and Dou 4 Perceived risk and severity of COVID-19 may also induce irrational beliefs about its prevention.Reference Rabalais 15 , Reference Ellis, David and Lynn 16 Rational action theory proposes that all action is fundamentally “rational” in terms of what the actor believes to be true, but in his or her practice comprises irrational as well as rational elements.Reference Jaeger, Webler and Rosa 17 Irrational beliefs are rigid, inaccurate, and illogical, but are used defensively to process external events. Unlikely to find empirical support, these beliefs are self-defeating, unconditional, and in conflict with reality.Reference Bridges and Harnish 18 Many studies found that that the more irrational the belief, the more negative the health behaviors.Reference Rabalais 15 , Reference Bridges and Harnish 18 , Reference Kaygusuz 19 Irrational beliefs commonly manifest in many social and health arenas.Reference Yang 8
Survival is a biological imperative for humans, and self-protection is the common behavioral response for confronting a mortal crisis. In sudden major crises, coping can induce excess self-protective behavior (EPB). COVID-19’s evolution on the world scene has not been paralleled by any other communicable disease since the 1918/19 Spanish Flu pandemic; a catastrophic phenomenon that killed an estimated 50-100 million people globally.Reference Bratspies 20 The dire threat to personal health and survival, posed by the COVID-19 pandemic, has quickly promoted perceptions of high risk for infection with potentially severe outcomes. In turn, these responses can be a strong stimulus for EPB. Meanwhile, EPB may be disproportionate and not recommended as an effective response to the actual threat; thus, overburdening individuals and society and sparking diversion of scarce critical resources away from places where need for assistance is most acute.Reference Cullen, Gulati and Kelly 9 In cognitive science, EPB emanates from people’s fear and distorted view of the world.Reference Yang 8 Irrational beliefs or subscription to myths about COVID-19 prevention measures could stimulate pervasive EPB. This type of behavior consumes a high degree of personal physical energy, and in the process diminishes disease immunity. Excessive protective measures can overstress health care facilities and other resources, and consequently exert a strong negative impact upon the economy and society as a whole.Reference Garfin, Silver and Holman 21 For example, panic buying of essential consumer items like toilet paper, first aid kits, bottled water, and hand sanitizer, in response to COVID-19, has led to global shortages and price gouging of consumer staples.Reference Garfin, Silver and Holman 21 This response impedes disease prevention and economic recovery. However, this issue has generated little discussion and debate,Reference Garfin, Silver and Holman 21 and no previous empirical studies have addressed EPB in relation to COVID-19 or other acute infectious respiratory diseases.
This study has three key objectives:
-
1. To examine levels of EPB by the Chinese amid the COVID-19 epidemic.
-
2. To evaluate temporal trends in EPB during that epidemic.
-
3. To study the association between perceived risk and severity of COVID-19, and belief in related prevention myths, respectively, and EPB.
This study may yield information important in formulating policy and health education initiatives aimed at reducing EPB, with the goal of improving the design and targeting of effective interventions for preventing and mitigating COVID-19.
Methods
Study Design
We conducted a prospective longitudinal observation study to examine temporal trends and changes in EPB, and its associations with selected perceptions and beliefs during the COVID-19 pandemic.
Participants
Participants were recruited via a survey advertisement from social media groups on WeChat and Douban, two of the most popular social media platforms in China. Inclusion criteria were membership in a common community; being in the age group 20-60 years; having access to a Smartphone; knowing the Chinese language; and being willing to participate in the panel study and provide follow-up information at the scheduled observation points. Participants were excluded if they refused to provide this information or had a medical condition that could limit or preclude their participation. Within the registration system, potential participants were screened to ascertain eligibility. Upon consent, participants received an electronic questionnaire and instructions on how to proceed. After reading the instructions, they were asked to provide an e-consent by tapping the “Confirmation and Authorization” button and were then directed to the questionnaire. A special administrative WeChat group was established to manage the follow-up data collection, using a unique QR code for each respondent. The QR code was the vehicle not only for identifying unique participants but prohibiting non-participants from taking the survey. After scanning the QR code, survey participants could enter the investigation group without further preconditions.
This panel study analyzed 5 waves of data collected over 1 month: Wave 1(5/Feb/2020), Wave 2(12/Feb/2020), Wave 3(19/Feb/2020), Wave 4 (26/Feb/2020), and Wave 5(4/March/2020). The entire observation period covered the peak and trough of the COVID-19 epidemic in China. The corresponding number of reported confirmed patients was 3887, 2015, 394, 433, and 133 in each wave, respectively. 25
Data Collection
An online survey was implemented on Wenjuanxing (www.wjx.cn), a survey service website similar to Qualtrics or SurveyMonkey, but tailored to Chinese users. Each wave of the survey had a dedicated electronic questionnaire access link. The online questionnaire link was posted to the respondent group, centrally managed in a WeChat group, and accessible every Wednesday from 10:30 a.m. to 4:30 p.m. In cases where participants missed their survey appointment, follow-up procedures were initiated by data collectors. Participants who did not respond by 11:00 a.m. the following Monday were classified as lost to follow-up. Data collectors and facilitators were third-year doctoral students in a public health program. All responses were anonymous. The questionnaire took approximately 10 minutes to complete, and the same survey protocol was used for every wave of the survey to assure homogeneity of data administration and collection. As appropriate, a token of appreciation, a total of 30 RMB was given to those participants who completed all 5questionnaires.
Measurement
In this study, basic individual demographic characteristics were tapped: age, gender, ethnicity, education level, marital status and occupation. Perceptions of risk and disease severity were respectively captured through the items “continual fear of infection by COVID-19” and “becoming infected by COVID-19 is a serious misfortune.”
This study addressed personal harboring of myths or irrational beliefs about effective COVID-19 prevention measures that were not founded upon reality and science. They reflected 5 common misconceptions that circulated during the COVID-19 epidemic in China: (1) Smokers are not susceptible to COVID-19, (2) Consuming alcohol can prevent the spread of the virus, (3) People should avoid people from Hubei province, where COVID-19 first manifested in China, in order to prevent contraction of the disease, (4) It is reasonable for employers to dismiss Hubei employees to prevent the spread of the novel virus, and (5) People who move away from an affected area should be deported back to their place of origin. Items were rated on a 5-point Likert-type scale, which ranged from 1 (strongly disagree) to 5 (strongly agree). Item scores were summed to attain a total score for belief in COVID-19 prevention myths. The higher that score, the greater the level of irrational prevention belief. The Cronbach’s α coefficient was 0·70, suggesting the questionnaire had acceptable reliability. Consistent with prior practices, a cutoff score of 15 or above signified strong acceptance or belief in prevention myths.Reference Yang 8 EPB was a common coping mechanism for confronting the COVID-19 epidemic in China. Currently, there is no protocol for determining EPB in this situation. We identified them empirically from social norms perspective.Reference Yang 8 Through an online survey, study participants stated which of 16 types of behavior, aimed at preventing COVID-19, they would categorize as EPB. Complete responses were obtained from 116 participants. Where there was 80% agreement on a type among these participants, we preliminarily categorized it as EPB. These selections were then reviewed and approved by 12 health experts, and the 5 that received universal acceptance by the participants and experts were classified as EPB. They included in this study: (1) Clothing disinfected every 1 or 2 days (Disinfecting clothes), (2) Frequent hand washing beyond the regular washing before and after meals or after work (Washing hands), (3) Frequent use of a disinfectant when washing hands at home (Sanitizing hands), (4) Hoarding masks, alcohol, and other forms of protective products (Hoarding products), and (5) Making arrangements for another or others to handle their family and occupational responsibilities if, and when, they contracted COVID-19 (Transferring responsibilities).
Data Analysis
All data were entered into a database using Microsoft Excel. They were then imported into SAS (9.3 version) for statistical analysis. Across survey waves, descriptive statistics were calculated for belief in prevention myths, perceived high risk for contracting the disease, perceived high severity of disease consequences, and EPB prevalence. The CATMOD program was used to conduct repeated measures analysis of variance to determine changing trends across the 5 observation points, and to examine the association between perceived disease risk and severity, and belief in prevention myths, respectively, with EPB using the method of weighted least squares.Reference Inc 22
Results
One hundred-and-fifty participants were recruited at baseline. The baseline was linkable and there were 3 intermediate and a final observation point, with 102 participants available for analysis throughout; 99 came from 24 provinces located across China, differentiated by region. The remaining 3 were international.
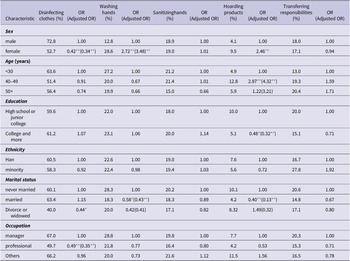
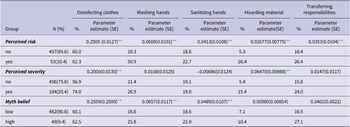
Of the study sample, 61.8% were female and 93.3% were Han Chinese. The average age of participants was 39.1 years (SD: 12.5), 43%, were never married, and 50.0% were married. The prevalence of belief in COVID-19 prevention myths was higher among males than females (adjusted OR: 0.14) and increased with age (adjusted OR: 8.25, 12.56). Married people had a lower prevalence of high perceived risk (OR: 0.36), and the middle-aged (40-49 years) had a higher prevalence of perceived disease severity than comparison groups (OR: 1.86) (Table 1). Disinfection of clothes was less prevalent among females than males (adjusted OR: 0.34), and among professionals than people in other occupational groups (adjusted OR: 0.35). Hand washing was more prevalent among females than males (adjusted OR: 3.48) and less prevalent among the married than the never married (adjusted OR: 0.43). Hoarding products was more prevalent among the middle-aged (adjusted OR: 4.32), the least educated (adjusted OR: 0.32), and the married than their respective demographic counterparts (adjusted OR: 0.13) (Table 2).
Table 1. Sample characteristics and prevalence of prevention myth belief, perceived disease risk, and severity

* P<0.05
** P<0.01
Table 2. Sample characteristics and prevalence of excessive self-protective behavior
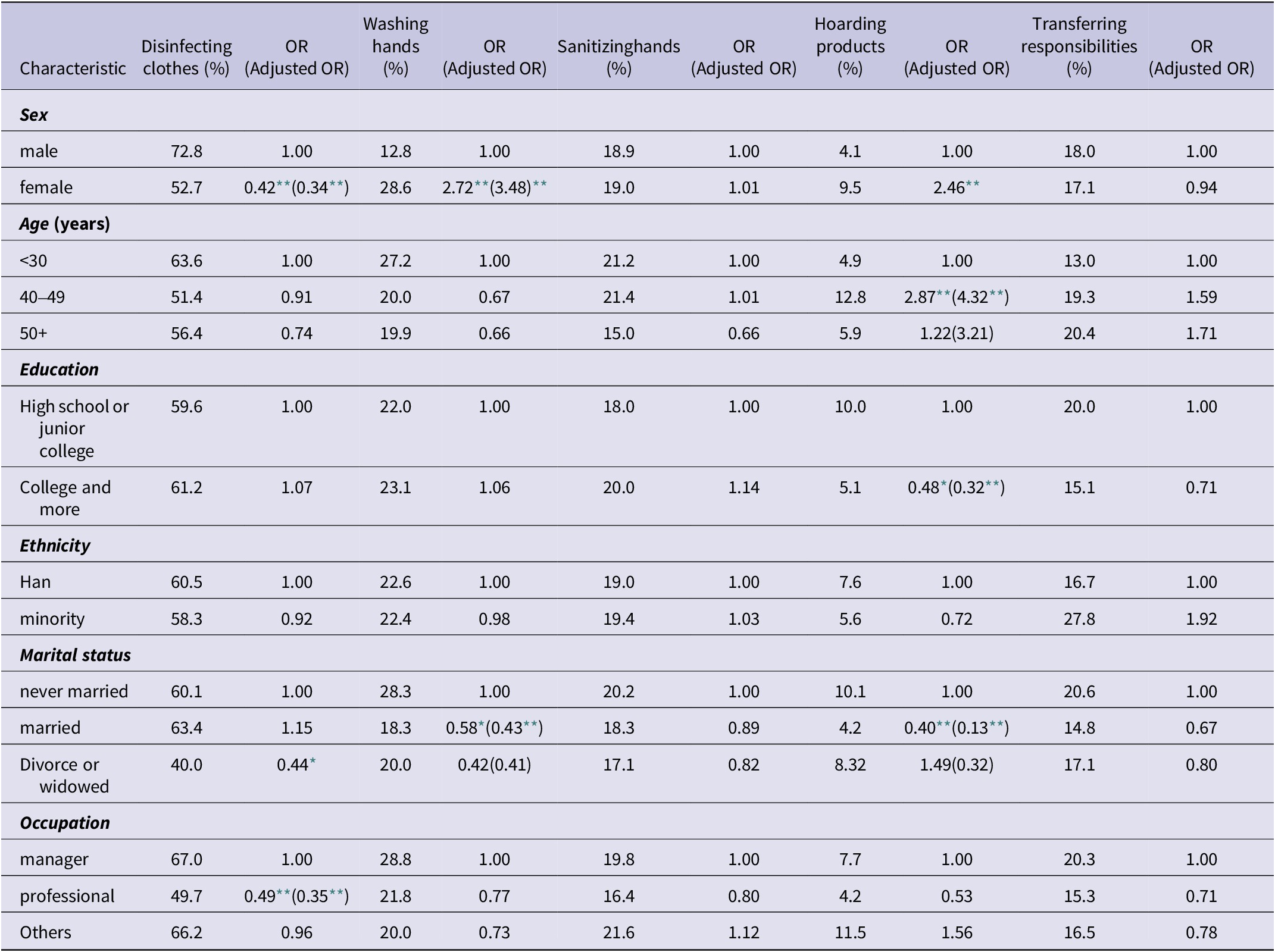
* P<0.05
** P<0.01
All participants knew the disease had attained epidemic proportions and was highly contagious at the time of the first survey was implemented. The prevalence at baseline of the perceptions of high risk of contracting COVID-19 and disease severity was 18.6% and 25.5%, respectively, and declined to 4.9% and 17.6% by the last observation point, with a statistically significant change. The prevalence of the 5 types of EPB showed a statistically significant downwards trend across the total observation period of this panel study. Simultaneously, there was a statistically significant upwards trend in belief in COVID-19 prevention myths (Table 3).
Table 3. Time change trend in prevention myth belief, perceived disease risk and severity, and excessive self-protective behavior

* P<0.05
** P<0.01
Perceived high risk for contracting COVID-19 was positively associated with each type of selected EPB, and perception that the disease had severe consequences was positively associated with disinfection of clothes and hoarding of products. Belief in the disease prevention myths was positively associated with disinfection of clothes and both hand washing and sanitization (Table 4).
Table 4. Association of perceived disease risk and severity and prevention myth belief with excessive self-protective behavior
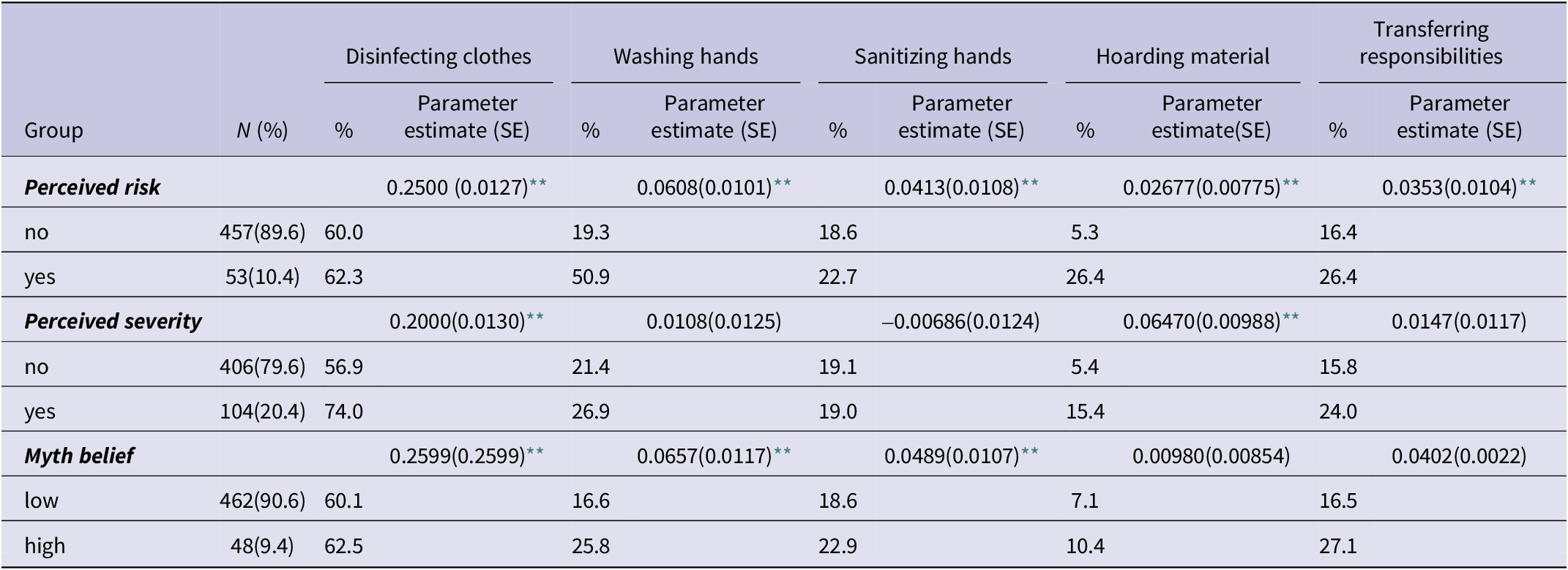
* P<0.05
** P<0.01
Discussion
At baseline, this study found that 18.6% and 25.5% participants, respectively, believed they were at high risk of contracting COVID-19, and that this disease seriously threatened their health. Turning to previous studies, 1 found approximately 10-30% of the general public were very worried or moderately worried about the possibility of contracting influenza during an outbreak.Reference Rubin, Potts and Michie 23 Another reported that during the period February 1 through 10, when disease cases were increasing dramatically, 15.3% of Shanghai and Wuhan residents perceived COVID-19 as a very serious disease.Reference Qian, Wu and Wu 24 Our research commenced at the peak of the epidemic, and one-fifth to one-quarter of study participants perceived the disease was very serious and their risk of contraction was high. COVID-19 is a new disease, and the epidemic may profoundly impact people mentally and behaviorally. Viewed as a stimulus, this disease can be overwhelming and elicit strong mental and behavioral responses. Many studies have found that COVID-19, now a global pandemic, generates negative mental and behavioral outcomesReference Cullen, Gulati and Kelly 9 , Reference Greenberg, Docherty and Gnanapragasam 10 that may include inappropriate health-protective and help-seeking behaviors.Reference Garfin, Silver and Holman 21
Addressing a gap in the literature, this Chinese study found changing temporal trends in perceived high risk of contracting COVID-19, perception of severe adverse consequences of the disease, belief in prevention myths about the disease, and EPB during the epidemic. Prevalence of perceived risk and severity declined over the observation period, a trend consistent with the decline in the actual risk of infection. The new reported COVID-19 patients in China across the 5 observation points numbered 3887, 2015, 394, 433 and 133, respectively. 25 As COVID-19 was reaching epidemic proportions, there were increases in the prevalence of perceptions of personal risk for contracting the disease and the severity of its health consequences. The prevalence of the five types of EPB, highlighted in this study, showed a statistically significant decreasing trend over the observation period. EPB is typically considered a behavioral overreaction in China and increases with perceived disease risk and severity. Plausibly then, high perceived risk and severity induce EPB. Contrasting with our findings about the perception data, belief in COVID-19 prevention myths manifested a statistically significant increasing trend over the observation period. The explanation may inhere in an “energy consumption” mechanism.Reference Posner and Rothbart 26 People likely functioned rationally as they mobilized all their physical and mental energy to cope with COVID-19 at the beginning of the epidemic. However, as time passed, such energy waned and rational thinking diminished as belief in prevention myths became more common. This information is useful for formulating prevention policy and educational programming.
The risk of disease or injury and the severity of outcomes are crucial themes in individual health behavior. This study provided new evidence that perceived risk of contracting COVID-19 and perception of the severity of its consequences were both positively associated with several types of EPB, findings generally compatible with those from some other studies.Reference Wise, Zbozinek and Michelini 3 , Reference Li, Yang and Dou 4 , Reference Dorfan and Woody 12 We found a negative association between belief in prevention myths and some of the constituents of EPB. Affirmation for our findings, other investigators also found a relationship between such a belief and negative health behaviour.Reference Rabalais 15 , Reference Bridges and Harnish 18
EPB transcends normal self-protective behaviors, with special significance from a disease prevention perspective. For effective prevention, it is necessary both to avoid inadequate prevention measures that increase the likelihood of a disease epidemic, and to avoid excessive activities that waste personal and social resources. These two scenarios may vary across cultures. Inadequate prevention may be a prominent problem in Western culture and excessive prevention in Eastern culture.Reference Yang 8 , Reference Christopher Perry, Bekes and Starrs 27 , Reference Berg and Lin 28 A related dimension of such cultural variance is societal “rigidity” versus “porousness.”Reference Van Bavel, Baicker and Boggio 29 “Rigid” cultures, such as those of Singapore, Japan, and China, have strict social norms and punishment for deviance, whereas “porous” cultures, such as those characterizing the U.S., Italy, and Brazil, reflect weaker social norms and greater permissiveness.Reference Gelfand, Raver and Nishii 30 “Qǐ rén yōu tiān” from ancient China is a tale about a person who worried every day the sky would collapse. This study found that in the COVID-19 epidemic there was pervasive over-prevention among members of the public. Excessive prevention consumes too much personal energy and societal resources, and hence impedes disease control and economic recovery. Government and society at large must give this issue more attention. Reforms in health policy and health education will be essential for minimizing the adverse effects of belief in prevention myths and associated deleterious behavior.
There are two study limitations. Firstly, our sample size is small. Nevertheless, the sample originated from 24 provinces covering diverse regions and a wide array of demographic characteristics. Also, sample attrition may introduce a “cluster” bias because many longitudinal studies likely over-represent some of these characteristics, such as high educational attainment. A more sophisticated design and representative sample would be necessary to resolve this problem. A second limitation in this study is the lack of a clear definition of EPB. We operationalized this concept through empirically identifying 5 constituents from a social norms perspective. Operationalization of the concept of belief in prevention myths may so be thought as an external criterion for measuring the validity of EPB.Reference Yang 8 , Reference Rabalais 15 , Reference Kaygusuz 19 Belief in prevention myths was significantly associated with 3 of the 5 types of EPB in this study. This finding enhances the validity of our measure of EPB. The concept and its operationalization require further research.
Conclusion
This study provides new information on the relationship between belief in COVID-19 prevention myths and EPB among the Chinese public, in the context of perceived risk of contracting the disease and perception of the severity of its consequences during the epidemic. As the virus spreads relentlessly around the globe, our findings could guide similar research outside China in less and more developed countries. They harbor important implications for understanding and decreasing EPB, as appropriate, during this new global pandemic.
Data availability statement
Data are available on reasonable request to the corresponding author.
Author contribution
Tingzhong Yang: Conceptualization, Methodology, Writing- Original draft preparation; Sihui Peng: Investigation, Resource, Writing - Review & Editing, Data curation, Supervision; Ian R.H. Rockett: Writing - Review & Editing.
Competing interest
The authors declare no competing interests.
Funding statement
This study was supported, in part, by the National Nature Science Foundation of China (Major Project 71490733).
Ethical standard
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation the Ethics Committee at the Medical Center, Zhejiang University (No.2014:1-017) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Verbal consent was obtained from all participants for being included in the study.
All participants received an electronic questionnaire and instructions on how to proceed. After reading the instructions, they were asked to provide an e-consent by tapping the “Confirmation and Authorization” button and then directed to the questionnaire.