Impact statement
This study provides crucial insights into the mental health status and risk factors faced by multicultural families (multi-CFs) in South Korea, a racially homogeneous country where such families face unique challenges. The findings reveal that multi-CFs experience significantly higher levels of stress, extreme sadness and despair compared to monocultural families (mono-CFs). These mental health disparities are exacerbated by precarious socioeconomic environments, unhealthy health behaviors and social isolation. Specifically, economic disadvantages, unstable marital statuses and risky health behaviors such as smoking and insufficient physical activity further worsen mental health outcomes among multi-CFs. The study highlights the urgent need for tailored intervention strategies that address these specific challenges. Key recommendations include promoting physical activity, enhancing social support networks and removing cultural and socioeconomic barriers to accessing mental health care. Furthermore, the household-level nature of mental health vulnerabilities in multi-CFs suggests that interventions should target entire families rather than focusing solely on individual members. This holistic approach is essential for breaking the cycle of disadvantage and improving overall well-being within these families. Despite certain limitations, such as the exclusion of individuals with poor Korean language skills and children under 19, this study contributes valuable knowledge to the understanding of mental health disparities in multi-CFs within a unique sociocultural context. The results underscore the importance of developing culturally sensitive, family-centered mental health interventions to address the specific needs of multi-CFs in South Korea and other similarly homogeneous societies.
Introduction
Amid globalization, multicultural families (CFs) are increasing and becoming common worldwide. The US is a representative multicultural society that has experienced a rapid increase in immigrants, who comprised 13.9% of the total U.S. population in 2022 (Migration Policy Institute, 2024). As of January 2023, 6.1% of people living in EU countries are non-EU citizens (Eurostat, 2024). Even countries that have historically had monocultural populations are no exception.
Social context of South Korea
South Korea has long emphasized ethnic and genealogical homogeneity, but since the late 20th century, the number of multi-CFs have risen owing to an influx of foreign workers, increased immigration through international marriages and globalization (Kim, Reference Kim2007). As of 2022, there are approximately 399,000 multi-CFs in South Korea, accounting for 1.83% of the total number of households (Statistics Korea, 2023). As of 2022, school-aged children from multi-CFs number approximately 169,000. Although the total student population in Korea declined by 7.9% during the 2017–2022 period due to the declining fertility rate, the number of students from multi-CFs increased by 54.2% during the same period (Ministry of Gender Equality and Family, 2023a).
However, multi-CFs in South Korea are distinct from their counterparts in immigrant-based countries with a highly heterogeneous population and multiculturalist societies, such as the US and Canada. The majority are formed through marriages between female migrants and Korean men, with the gender ratio of marriage migrants being 78.6% female and 21.4% male. Additionally, marriage migrants are primarily from other Asian countries, particularly China (51.3%), Vietnam (21.8%) and the Philippines (5.4%), with these countries accounting for about 82% of all countries of origin (Ministry of Gender Equality and Family, Reference Division2023b). In terms of the Korean sociocultural context, these families face significant challenges in acculturating. An international survey on national identity indicates that 71.2% of South Koreans consider ancestry an essential criterion for being a genuine country member, strikingly higher than the percentages in Switzerland (35.5%) and the US (42.2%) (ISSP Research Group, 2015). Furthermore, 69.8% of marriage migrants and naturalized citizens have reported facing discrimination in their workplace solely for being a foreigner (Ministry of Gender Equality and Family, 2022).
High risk of mental illness on migrants and ethnic minorities
Thus, mental health disorders of multi-CFs and migrants are a major public health concern. Owing to the cultural milieu and socioeconomic adversities they face, ethnic minorities are at a heightened risk of a range of mental illnesses such as stress, anxiety and depression, and exhibit a higher incidence of suicide and admission for suicide or self-harm (Karlsen and Nazroo, Reference Karlsen and Nazroo2002; Ngwena, Reference Ngwena2014; Wyatt et al., Reference Wyatt, Ung, Park, Kwon and Trinh-Shevrin2015; Forte et al., Reference Forte, Trobia, Gualtieri, Lamis, Cardamone, Giallonardo, Fiorillo, Girardi and Pompili2018). Indeed, rates of psychosis among immigrants are much higher than those among native populations, with an incidence rate ratio more than three times higher (Castillejos et al., Reference Castillejos, Martín-Pérez and Moreno-Küstner2018). For displaced populations such as refugees, psychiatric disorders, including post-traumatic stress disorder (PTSD), anxiety and depression, are more prevalent (Blackmore et al., Reference Blackmore, Boyle, Fazel, Ranasinha, Gray, Fitzgerald, Misso and Gibson-Helm2020; Bedaso and Duko, Reference Bedaso and Duko2022). Additionally, marriage migrants, who are already encumbered by their identity as an ethnic minority, experience gender vulnerability and family conflicts, which collectively engender a higher risk of social exclusion, depression and suicide (Wyatt et al., Reference Wyatt, Ung, Park, Kwon and Trinh-Shevrin2015; Kim, Reference Kim2018). Even offspring of immigrants experience higher risk of depression compared to the host population, resulting from their adverse socioeconomic status (SES) and perceived ethnic discrimination (Stronks et al., Reference Stronks, Şekercan, Snijder, Lok, Verhoeff, Kunst and Galenkamp2020).
Despite the high need for mental health care among migrants and ethnic minorities, they have poor access to and limited use of mental health services. Lack of trust in healthcare providers, cultural beliefs, concerns about potential stigmatization, lack of insurance, language barriers and challenges in seeking help may be influencing factors (Heredia Montesinos, Reference Heredia Montesinos2015; Derr, Reference Derr2016; Mohammadifirouzeh et al., Reference Mohammadifirouzeh, Oh, Basnyat and Gimm2023). Such delayed help-seeking often results in treatment delays and subsequently affects treatment outcomes in psychotic disorders (Albert et al., Reference Albert, Melau, Jensen, Hastrup, Hjorthøj and Nordentoft2017).
Study objectives and necessity
In South Korea, multi-CFs refer to households with at least one member who is an ethnic minority. Marriage migrants can become naturalized Korean citizens when they fulfill the stipulated requirements, which includes duration of stay in the country. The Korean government enacted the Multicultural Families Support Act in 2008 and has operated 230 centers for multi-CFs nationwide. However, the government support program mainly focuses on Korean language education for marriage migrants and basic academic skills for their children. The Korean public has consistently reported a low level of receptiveness to multiculturalism (Ministry of Gender Equality and Family, 2023a). Furthermore, in terms of the national identity, Korean people tend to place more value on ancestry over country of birth or naturalization (ISSP Research Group, 2015), raising concerns about perpetuation and generational transmission of adverse social experiences. Moreover, research on mental health and racial minorities has mainly been conducted in multiethnic countries such as the US, and thus may not be applicable to mono-ethnic or monoracial countries such as South Korea. Accordingly, the current study may serve as a prime example of research for mono-ethnic countries.
This study aims to compare stress recognition, the experience of sadness or despair and depressive symptom prevalence between mono- and multi-CFs. In addition, we identify the risk factors of these indicators in multi-CFs. We subsequently provide countermeasures for improving mental health equity in multi-CFs.
Theoretical background
As the notion of an immigrant encompasses a complex construal of distinct nationality, culture, race and ethnicity, contextual factors affect their mental health, ranging from personal abilities (e.g., language competency), family, neighborhood and social position to social experiences (Alegría et al., Reference Alegría, Álvarez and Dimarzio2017). Immigration is a critical process that can be influenced by these social and institutional factors and, at the same time, lead to changes in each domain. Therefore, migrants’ health needs to be investigated through the lens of social determinants of health, incorporating behavioral, cultural and structural frameworks (Castañeda et al., Reference Castañeda, Holmes, Madrigal, Young, Beyeler and Quesada2015).
Additionally, the relation between social exclusion and mental health arises through the psychosocial stress process, indicating that cumulative exposures to social isolation and discrimination stress affect brain neurotransmitter systems and amplify psychotic and affective disorders (Brandt et al., Reference Brandt, Liu, Heim and Heinz2022). It is worth noting that both income inequality and minority status among immigrants synergistically impair the chances for social participation, thereby increasing social exclusion (Heinz et al., Reference Heinz, Zhao and Liu2020).
A great deal of previous studies have explored the effects of discrimination, acculturative stress, social exclusion and family conflict on migrants’ mental health. Migrants undergo a process of acculturation, wherein they are integrated into a culture by accepting the values, beliefs and attitudes of the culture, and the cultural conflict and acculturative stress they experience serve as major barriers to their mental health (Hovey and Magaña, Reference Hovey and Magaña2003; Nazroo, Reference Nazroo2003; Heredia Montesinos, Reference Heredia Montesinos2015; Wyatt et al., Reference Wyatt, Ung, Park, Kwon and Trinh-Shevrin2015; Forte et al., Reference Forte, Trobia, Gualtieri, Lamis, Cardamone, Giallonardo, Fiorillo, Girardi and Pompili2018). Language proficiency is associated with mental disorders in migrants, including mood, stress, anxiety and psychotic disorders (Montemitro et al., Reference Montemitro, D’Andrea, Cesa, Martinotti, Pettorruso, Di Giannantonio, Muratori and Tarricone2021). Particularly in South Korea, Korean language proficiency in multi-CFs has been linked to the risk of social exclusion (Kim, Reference Kim2018). Moreover, migrants’ experiences of interpersonal racism, institutional discrimination and household socioeconomic disadvantage have been identified as crucial contributors to the level of their depression, suicide risk and psychosis (Karlsen and Nazroo, Reference Karlsen and Nazroo2002; Nazroo, Reference Nazroo2003; Juang and Cookston, Reference Juang and Cookston2009; Stein et al., Reference Stein, Kiang, Supple and Gonzalez2014; Heredia Montesinos, Reference Heredia Montesinos2015; Wang et al., Reference Wang, H-C and Wong2021). In terms of social status, migrants who experience a downward shift in social status as a result of their relocation to another country compared to that in their home country are at a greater risk of developing common mental disorders (Das-Munshi et al., Reference Das-Munshi, Leavey, Stansfeld and Prince2012). Beyond economic capital, social capital can have profound implications for migrants’ mental health. Social exclusion, social isolation, disruption of social networks, lack of social support and separation from family, all following migration, increase the risk of depressive disorders, suicidal acts and suicide among migrants (Hagaman et al., Reference Hagaman, Sivilli, Ao, Blanton, Ellis, Lopes Cardozo and Shetty2016; Alegría et al., Reference Alegría, Álvarez and Dimarzio2017). Meanwhile, immigrants’ cultural resilience serves a protective role in preventing the onset of depression, and their high levels of religiosity and faith sometimes act as coping strategies (Cervantes et al., Reference Cervantes, Gattamorta and Berger-Cardoso2019; Lusk et al., Reference Lusk, Terrazas, Caro, Chaparro and Puga Antúnez2021).
Particularly concerning familial factors, they can act as both stressors and buffers for migrants’ mental health. Familial and interpersonal problems, such as domestic violence and pressures from the community, were major risk factors for suicide among migrants and ethnic minorities (Heredia Montesinos, Reference Heredia Montesinos2015). In the context of multi-CFs in Korea, marriage migrant mothers’ experiences of discrimination influence maternal depression, which in turn affects their parenting behavior and their children’s psychological adjustment (Chung and Lim, Reference Chung and Lim2016). Meanwhile, family reunification and familism during post-migration tend to decrease the risk of depressive symptoms for immigrant parents (Ornelas and Perreira, Reference Ornelas and Perreira2011). Parental support attenuates migrant children’s issues such as identity confusion and psychological well-being (Walsh et al., Reference Walsh, Edelstein and Vota2012). Similarly, adolescents from multi-CFs in Korea benefit from support from family, friends and teachers, which facilitates higher acculturation. As their acculturation progresses toward social integration, they report greater life satisfaction (Yoo, Reference Yoo2021).
Methods
Data and participants
We used data from the Community Health Survey (CHS) of Korea. CHS surveys 900 adults over 19 years of Korean citizenship by district unit by Korea Disease Control Prevention and Control Agency (KDCA) and local governments since 2008, surveying approximately 230,000 people yearly. To produce representative statistics, CHS conducts household unit surveys through a multistage stratified sample design. In addition, the survey on multi-CFs, which is the main research group of our study, has been conducted every 3 years from 2019. Therefore, the study subjects were 228,952 adults aged 19 and older in 2019, of which 3,524 responded that they were from multicultural households. CHS classifies a multicultural household a family comprised of people from different nationalities, races and cultural backgrounds. A family is also classified as multi-CF if it includes a person who emigrated from a foreign country even though they acquired Korean nationality, or if the respondent was born in Korea but at least one parent was born in a foreign country and answered that they consider themselves to be multicultural.
Variables
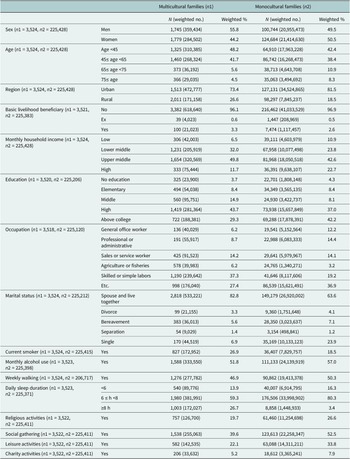
To compare the level of mental health in mono- and multi-CFs, we selected stress recognition, experience of extreme sadness or despair and depressive symptoms as the primary dependent variables. These variables were chosen based on their relevance to mental health as indicated in previous research. For instance, stress recognition has been consistently linked to mental health outcomes, where higher levels of perceived stress are associated with increased risks of anxiety and depression (Cohen et al., Reference Cohen, Kamarck and Mermelstein1983; Lazarus, Reference Lazarus1984). Similarly, experiences of extreme sadness or despair are critical indicators of mental health status, often predictive of depressive disorders (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Koretz, Merikangas, Rush, Walters and Wang2003). Depressive symptoms themselves are widely recognized as core measures of mental health, reflecting both the presence and severity of depression (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). Therefore, selecting these variables allows for a comprehensive assessment of mental health, capturing a range of emotional and psychological states that are crucial for understanding overall well-being. Additionally, consultation with experts due to stress and consultation with experts due to sadness or despair were considered key mental health-related outcomes. We incorporated multiple social determinants of health for multi-CFs as independent variables. These range from demographics and health-promotion behaviors to household characteristics, SES and social capital, all of which are associated with potential discrimination, social experiences and coping strategies (Castañeda et al., Reference Castañeda, Holmes, Madrigal, Young, Beyeler and Quesada2015; Alegría et al., Reference Alegría, Álvarez and Dimarzio2017). Household and socioeconomic factors include sex, age, region, beneficiary status for basic livelihood, monthly household income, education, occupation and marital status. Additionally, current smoking, monthly alcohol use, weekly walking and daily sleep duration were selected as health-related behaviors. Religious activities, social gatherings, leisure activities and charity activities were chosen as indicators of social capital (Table 1).
Table 1. Definition of variables

Statistical analysis
We performed descriptive statistics to compare the characteristics of mono- and multi-CFs. In addition, a chi-squared test compared the indicators related to stress and depressive symptoms in the two groups, and multiple logistic regression identified risk factors related to stress and depressive symptoms in multi-CFs. All analyses were performed by reflecting the multi-stratified cluster sampling with SAS for Windows 9.4 (SAS Institute Inc., NC, USA).
Results
Descriptive statistics
Of 228,952 respondents, 3,524 (1.9%) were from multi-CFs. The percentage of men (55.8%) was higher among multi-CFs, while the percentage of women (50.5%) was higher among mono-CFs. The most common age was <45 in both groups, and there were more people from urban regions than rural regions. The percentage of basic livelihood beneficiaries was higher among multi-CFs (3.3%) than mono-CFs (2.6%). By income level, upper middle class was the most common in both groups. In terms of education, high school (43.7%) was the most common among multi-CFs, while college or higher (42.2%) was that among mono-CFs. Skilled or simple labor (37.3%) and other (36.9%) were the most common occupations among multi-CFs and mono-CFs, respectively. The highest number of people lived with their spouse in both groups (multi-CFs: 82.8%; mono-CFs: 63.6%). The percentage of current smokers was higher among multi-CFs (multi-CFs: 26.9%; mono-CFs: 18.5%), while the percentages of people engaging in monthly alcohol drinking (multi-CFs: 51.8%; mono-CFs: 57.0%) and weekly walking were higher among mono-CFs (multi-CFs: 46.9%; mono-CFs: 50.3%). The most common daily sleep duration was 6–8 h in both groups. Finally, proxies of social activities, namely religious activities, social gathering, leisure activities and charity activities were higher in mono-CFs than multi-CFs (Table 2).
Table 2. Descriptive analysis

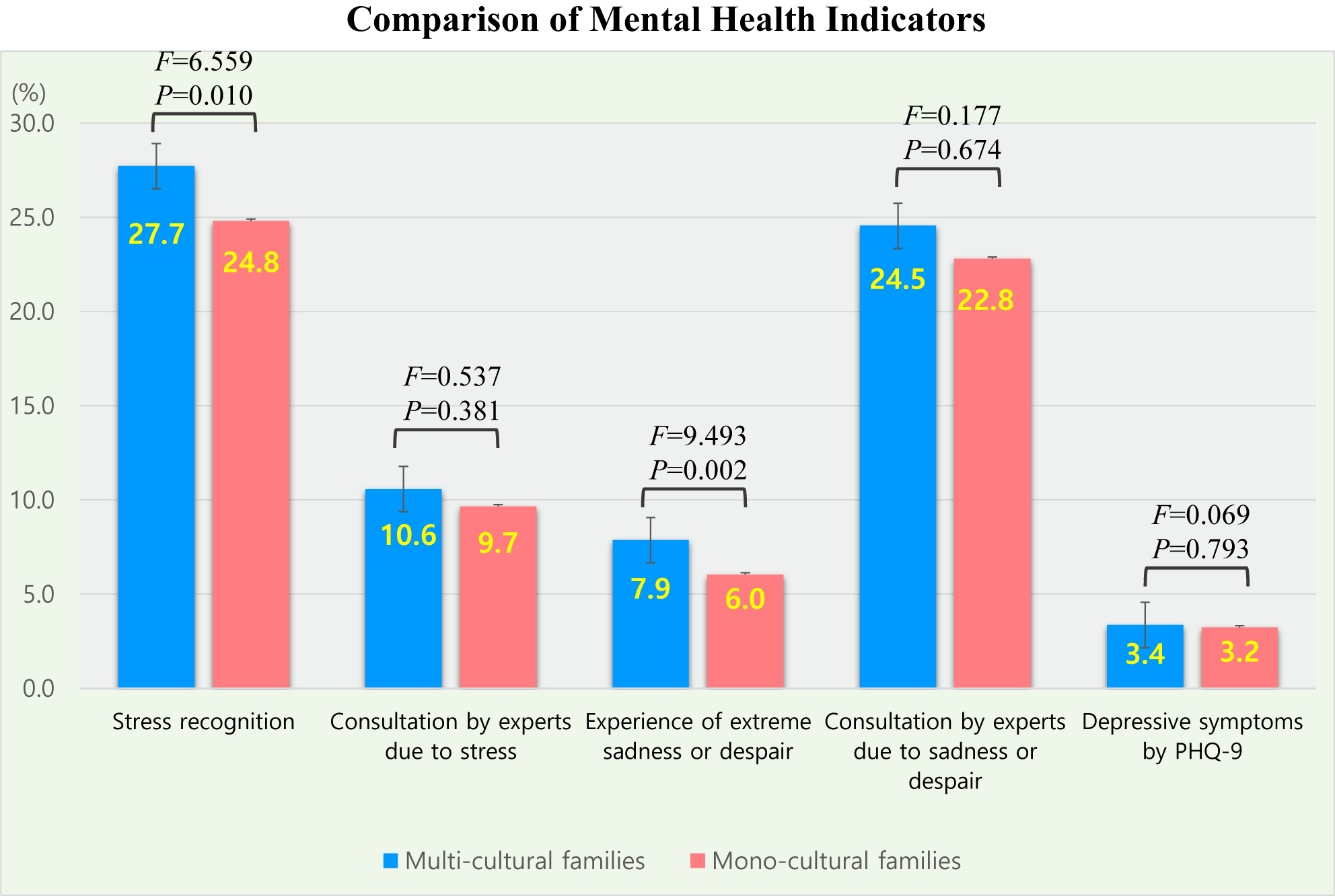
Stress recognition, experience of extreme sadness or despair and depressive symptoms between multicultural and monocultural families
Stress recognition was significantly higher among multi-CFs (27.7%) than mono-CFs (24.8%) (F = 6.559, P = 0.010), while the resulting rate of counseling did not differ significantly between the two groups. The percentage of individuals who have experienced extreme sadness or despair was significantly higher among multi-CFs (7.9%) than mono-CFs (6.0%), but the resulting rate of counseling did not differ significantly between the two groups. Finally, the prevalence of depressive symptoms was higher in multi-CFs (3.4%) than mono-CFs (2.9%) but not to a significant extent (Figure 1).

Figure 1. Comparison of stress recognition, sadness or despair and depressive symptoms of multicultural and monocultural families.
Risk factors in stress recognition, experience of extreme sadness or despair and depressive symptoms in multicultural families
Stress recognition did not differ between genders. The odds for stress recognition were higher (OR = 2.93) in the ≥75 years group than the <45 years group, in the urban region (OR = 1.14) than rural region, and among current beneficiaries (OR = 1.93) than non-beneficiaries. Stress recognition did not differ significantly according to household income. Regarding those with a college degree or higher, the odds for stress recognition were higher among those without education (OR = 1.72) but lower among those with middle school (OR = 0.66) and high school education (OR = 0.84). The odds for stress recognition among office workers were lower among those in agriculture or fisheries (OR = 0.59). In terms of marital status, the odds were higher among those who are divorced (OR = 1.82) or separated (OR = 1.50) than those who live with their spouse. The odds were higher among current smokers (OR = 1.19) and those who do not walk weekly (OR = 1.25). Moreover, the odds were higher among those who sleep fewer than 6 h a day (OR = 3.48) than those who sleep 6–8 h a day, higher among those who do not have social gatherings (OR = 1.36) and lower among those who do not engage in leisure activities (OR = 0.84).
The odds for sadness or despair were higher among men than women (OR = 1.57) and highest among the 45–64 years group compared to the ≥75 years group (OR: 4.00). However, depressive symptoms did not differ significantly according to sex and age. By region, the odds for depressive symptoms were higher in the urban region (OR = 1.48). The odds for sadness or despair (OR = 1.50) and depressive symptoms (OR = 4.75) were higher among the current basic livelihood beneficiary group than the non-beneficiary group, while the odds were 2.51 and 5.60 in the ex-beneficiary group compared to the non-beneficiary group, respectively. In terms of household income, the odds for sadness or despair (OR = 2.50) and depressive symptoms (OR = 3.22) were higher in the low-income group compared to the high-income group. Regarding those with a college degree or higher, the odds for sadness or despair were higher among the no-education (OR = 1.37) and elementary groups (OR = 2.19), while those for depressive symptoms were lower in the middle school group (OR = 0.38). With reference to office workers, with the exception of the professional or administrative group having no significant differences, all other occupations had significantly lower odds for both sadness or despair and depressive symptoms. In terms of marital status, the odds for sadness or despair were higher in the bereaved group (OR = 1.64) than the group living with their spouse. Further, for the group living with their spouse, the odds for depressive symptoms were higher in the separated group (OR = 2.06) but lower in the divorced group (OR = 0.2). There were no significant differences according to current smoking and drinking status. In terms of weekly walking, the odds for sadness or despair and depressive symptoms were both higher in the “no” group. For the group who sleep 6–8 h a day, the <6 h group had higher odds for sadness or despair (OR = 2.24) and depressive symptoms (OR = 6.87). The odds for depressive symptoms were higher (OR = 1.75) in the no religious activities group, and the odds for sadness/despair (OR = 2.00) and depressive symptoms (OR = 5.32) were higher in the social gathering group (Table 3).
Table 3. Results of multiple logistic analysis of stress, extreme sadness or hopelessness and depressive symptoms in multicultural families

Discussion
Multi-CFs in South Korea are vulnerable groups with higher levels of stress and experiences of extreme sadness or despair relative to mono-CFs. Additionally, multi-CFs are likely to be positioned in risky environments regarding lower SES, a high prevalence of smoking, a shortage of walking practice, abnormal sleeping times and social isolation, all of which are directly linked to a decrease in mental health. Interventions must promote health activities and help families from different ethnic backgrounds get involved in their communities.
Stress recognition and extreme sadness or despair among multi-CFs were significantly higher than mono-CFs, but there was no difference in the level of depressive symptoms and specialist consultation rate. This result contradicts previous studies and reveals the mental health characteristics of migrant women in multi-CFs in the social context of South Korea. According to review papers comparing mental health levels of immigrants and nonimmigrants, the results for suicidal behavior and death by suicide were inconsistent, with no difference or better than nonimmigrants in some cases (Forte et al., Reference Forte, Trobia, Gualtieri, Lamis, Cardamone, Giallonardo, Fiorillo, Girardi and Pompili2018).
Vulnerabilities in women or younger people from multi-CFs regarding mental health
In our analysis of mental health risks among multi-CFs, stress and sadness or despair were more prevalent in women compared to men and in younger adults compared to older age. Previous studies have also discussed the impact of sociodemographic factors on migrants’ mental health. Migrants’ country of origin was significantly associated with suicide rate (Bhui and McKenzie, Reference Bhui and McKenzie2008; Wong et al., Reference Wong, Vaughan, Liu and Chang2014; Forte et al., Reference Forte, Trobia, Gualtieri, Lamis, Cardamone, Giallonardo, Fiorillo, Girardi and Pompili2018), and younger female immigrants (Montesinos et al., Reference Montesinos, Heinz, Schouler-Ocak and Aichberger2013); in particular, young female immigrants from South Asia have been identified as a major vulnerable group for mental health (Spallek et al., Reference Spallek, Reeske, Norredam, Nielsen, Lehnhardt and Razum2015). In a study of South Asian (SA) immigrants in the US and UK, SA women and SA youth exhibited poor treatment-seeking patterns due to low trust in practitioners and adherence to collectivist family norms. Experiences of domestic violence, financial pressure and low self-esteem further exacerbate gender and age disparities in depression. For SA youth, poor acculturation and discrimination increase stress (Karasz et al., Reference Karasz, Gany, Escobar, Flores, Prasad, Inman, Kalasapudi, Kosi, Murthy, Leng and Diwan2019). In the Korean context, a study sheds light on age and time concerns among Asian female marriage migrants in Korea. It reported better acculturation with longer residence in Korea, while individuals aged 30–45, compared to older individuals, experienced significantly higher levels of acculturative stress, even after adjusting for other demographics (Kim et al., Reference Kim, Ham, Cho, Ej and Lee2022). These recurring tendencies underscore the importance of cultural norms and duration of residence related to acculturation, rather than biological reasons.
Impact of economic disadvantages and unstable marital status on multi-CFs
Regarding SES factors, economic disadvantages, such as families receiving benefits or having low household income, were significant risk factors for extreme sadness or despair and depressive symptoms in this study. Interestingly, middle/high school graduates showed some protective effects on mental health compared to college graduates. Office workers had a higher risk, whereas other occupations were associated with lower risks of mental illness, contrasting with previous findings. According to a WHO survey, higher education levels in high-income countries improve treatment compliance for severe or moderate mental disorders (Evans-Lacko et al., Reference Evans-Lacko, Aguilar-Gaxiola, Al-Hamzawi, Alonso, Benjet, Bruffaerts, Chiu, Florescu, de Girolamo and Gureje2018). In the UK, migrants from ethnic minorities, with low household income, and not economically active had more than five times the odds ratio of common mental disorders compared to nonmigrant white British individuals with professional occupations, high income and education (Goodwin et al., Reference Goodwin, Gazard, Aschan, Maccrimmon, Hotopf and Hatch2018). Our results highlight the greater importance of economic concerns for the mental health of multi-CFs compared to other aspects of SES, such as occupation or educational achievement.
The impact of marital status on mental health was inconsistent for different parameters. In general, unstable marital status adversely affected mental health of multi-CFs, but the risk of depressive symptoms was significantly lower among the divorced group compared to the living with spouse group. This may be because spousal conflicts among non-divorced families may cause depressive symptoms. A total of 21.2% of marriage migrants in South Korea have experienced discrimination from family members because of their foreign origin (Ministry of Gender Equality and Family, 2022), highlighting the serious level of discord within families. Indeed, the primary concern for marriage migrants in Asia is the relationship among extended family members, unlike in Western countries, which are predominantly interested in race and ethnic integration (Yeung and Mu, Reference Yeung and Mu2020). In a comparison of intra-Asian countries, Vietnamese marriage migrants in South Korea, compared to those in Taiwan, experience more rigid gender expectations related to the family role as daughters-in-law. These gender systems and cultural norms subject female migrants to gender-based and ethnic discrimination (Chang, Reference Chang2020).
Need for enhancing health behaviors and social participation
Regarding health behaviors, multi-CFs exhibited higher rates of smoking, lower levels of physical activity (walking) and unhealthy sleep durations compared to Korean families, and these health risk behaviors have emerged as significant factors influencing their mental health. Based on a study in South Korea, Park et al., Reference Park, Lee, Park and Lee2018 reported that, compared to those from mono-CFs, children from multi-CFs display higher rates of alcohol use, smoking and drug use, alongside an increased prevalence of psychological problems such as depressed mood, suicidal ideation and attempts (Park et al., Reference Park, Lee, Park and Lee2018). We can also consider the possibility of somatization. Untreated mental illnesses are often presented as somatic rather than mental symptoms, manifesting as physical issues like sleep abnormalities, bodily pains or gastrointestinal problems (Karasz et al., Reference Karasz, Gany, Escobar, Flores, Prasad, Inman, Kalasapudi, Kosi, Murthy, Leng and Diwan2019). In essence, health behaviors in multi-CFs in South Korea are notably suboptimal, and the amelioration of these health behaviors is crucial for enhancing both physical and mental health.
Social participation has been reported to have positive effects on mental health. The main channels through which migrants receive social support and seek help regarding their mental health are family, friends or religious leaders, and social support from these individuals lowers immigration stress (Derr, Reference Derr2016; Sanchez et al., Reference Sanchez, Diez, Fava, Cyrus, Ravelo, Rojas, Li, Cano and De La Rosa2019). Furthermore, social capital mediates the association between immigrant status (i.e., time since immigration, asylum status) and psychological distress (Johnson et al., Reference Johnson, Rostila, Svensson and Engström2017), and immigrants with rich social networks in Korean society are at a low risk of social exclusion (Kim, Reference Kim2018). Moreover, social capital in multi-CFs is important because maternal social capital leads to children’s physical growth and health. Social networks function as crucial information channels, enabling mothers to obtain essential knowledge about parenting attitudes, nutrition and child-rearing practices that can profoundly impact their children’s nutritional status (De Silva and Harpham, Reference De Silva and Harpham2007). We observed a correlation between increased leisure activity participation and higher stress recognition. Despite this association, due to the limitations of the cross-sectional design in establishing causal relationships, it can be interpreted that people with high stress levels are more likely to engage in leisure activities to manage stress.
Implication and limitations
In summary, we observed social deprivations among multi-CFs in Korean society, accompanied by elevated levels of stress recognition and experiences of extreme sadness or despair compared to mono-CFs. Considering their lower SES and social isolation, as well as its strong association with mental distress in this study, the mental health of multi-CFs could worsen over time if there are no adequate interventions. Intervention strategies should be prioritized toward mitigating economic hardship, improving their health behaviors and increasing social participation, thereby helping them break the cycle of disadvantages. These goals can be achieved efficiently by promoting physical activity and expanding opportunities to participate in more social gatherings. Finally, since the scope of analysis was limited to members of multi-CFs as opposed to individual immigrants, our results depict the mental health status in household units. In the same context, mental health vulnerability is likely to be linked to the household characteristics of multi-CFs rather than individual issues, so we argue that household-level interventions, and not individual-level interventions, are needed for immigrant families.
This study has several limitations. First, in the case of nationality acquired through marriage, those with poor Korean communication skills were excluded from the survey. In the case of marriage migrants, the proportion of women is much higher (Ministry of Gender Equality and Family, Reference Division2023b). Therefore, this result may be an underestimation of the mental health outcomes of immigrant and ethnic minorities (mainly women). Second, the cross-sectional CHS data we used has limitations in investigating overall life-course perspectives. It does not cover children under 19 and is not suitable for further subdividing multi-CFs by age group due to the small sample size. Given that risk factors can vary by age and that childhood experiences of youth in multi-CFs can impact their adulthood mental health, future studies need to consider age segments or generational effects. Accumulating data over several years can enable the acquisition of a sufficient sample size and more precise study targets. Third, in our study, responses related to stress or anxiety were measured using a Likert scale or ‘yes or no’ format. However, using more sophisticated tools such as the Perceived Stress Scale (PSS) or the Depression Anxiety Stress Scales (DASS) could allow for a more robust and in-depth analysis. Lastly, the absence of information on immigrants’ countries of origin made it impossible to discriminate ethnic differences in detail or reflect them in the investigation. However, despite these limitations, this study is meaningful in that it identified the mental health status and risk factors of multi-CFs in the sociocultural context of a homogeneous country, which is different from the existing US and European countries.
Conclusions
Multi-CFs exhibited higher levels of recognition of stress and experience of extreme sadness or despair than mono-CFs. Even within multi-CFs, since the problems of groups with relatively low SES were greater, this group should be considered as the priority group for intervention. This group is placed in a socially, economically and culturally vulnerable environment, and low SES and poor social activities and networks increase stress and despair. Social isolation should be improved, and social integration and health equity should be achieved by supporting multi-CFs’ diverse social participation. This study is meaningful in that it derived findings about the mental health problems experienced by multi-CFs in a homogeneous country and expands the variation of the sociocultural context.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2024.108.
Data availability statement
The data are available from KDCA website. If you need the processed data, please contact the corresponding author to request the data.
Author contribution
M.-B.P. initiated the idea, led the formal analysis and reviewed and edited the final draft of the article. E.K. wrote the original draft and reviewed and edited the article.
Competing interest
The authors declare none.
Ethics statement
This study was conducted in accordance with the Declaration of Helsinki, and all of the materials used in the article were only publicly available data. Moreover, all of those data are non-identifying data and anyone can use it.