No CrossRef data available.
Published online by Cambridge University Press: 23 March 2020
In DSM-V, catatonia is individualized as a disease of its own. The priority is to look first for organic causes like intoxication. We present a clinical case diagnosed with intellectual disability (ID) and catatonia.
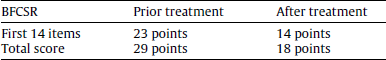
To study a case of catatonia which underwent testing using Bush-Francis Catatonia rating scale (BFCRS) prior/after clinical intervention. We therefore study catatonia's etiology in ID population.
To study the etiology of catatonia (and its clinical complications) in ID.
Our patient is 48-year-old female with DI. Considering her clinical features of catatonia (using BFCRS) and clinical examination (fever and hypoxia), the case orientated towards a secondary diagnosis. Work-up tests revealed pneumonia in the lower lobe of the right lung (chest radiography showed opacities and blood tests showed Leuokocytosis with a left shift). The case further received a course oral levofloxacin (500 mg/day) and haloperidol was stopped. Valproic acid was also added to a dose of 600 mg/day, which led to clinical improvement. Remaining psychotropic treatment (duloxetine 60 mg/day, lorazepam 15 mg/day, diazepam 35 mg/day) was not modified.
After 1 month, the patient improved according to BFCSR score.
We presented a case of presence of catatonia in other psychiatric conditions and undiagnosed general medical conditions. Haloperidol is contraindicated those circumstances and it may have worsened her clinical state (it should be used cautiously in DI). Other medications (gabaergic drugs) should be considered in such settings and rare causes related to hypoxia cannot be ruled out (Table 1).
The authors have not supplied their declaration of competing interest.
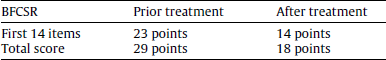

Table 1
Comments
No Comments have been published for this article.