Influenza pandemics remain among the most critical emergencies to which societies and governments are vulnerable. Robust planning and preparedness are needed to minimize the impact of these events. During the 20th century, 3 influenza pandemics occurred with varying severity and impact, including the 1918 pandemic, which caused approximately 50 million deaths globally.Reference Johnson and Mueller1
European national influenza pandemic preparedness plans were assessedReference Paget and Aguilera2-Reference Mounier-Jack and Coker4 before the 2009 influenza pandemic in 2001, 2005, and 2006. In 2001, Paget and Aguilera, on behalf of the European Influenza Surveillance System, reviewed the availability of pandemic plans at national and subnational levels, the availability of a domestic vaccine manufacturer or arrangements for vaccine supply, and the priority groups for vaccination in 16 countries participating in the European Influenza Surveillance System.Reference Paget and Aguilera2 In 2006, Mounier-Jack and Coker reviewed the published national pandemic influenza preparedness plans from 21 countries, including European Union (EU) countries, Norway, and Switzerland. At this time a majority of the European population (93%) was covered by a national pandemic plan, though some issues were not specified in the plans, such as maintenance of essential services, putting plans into practice, and public health interventions.Reference Mounier-Jack and Coker4
The awareness of the need of national preparedness plans was heightened following the events surrounding the rapid increase of avian influenza A (H5N1) outbreaks,Reference Snacken, Kendal and Haaheim5 with associated human cases from Asia to Europe and Africa after 2005. The need to rapidly respond at an EU level to international events such as A (H5N1) and severe acute respiratory syndrome in 2003 were some of the key arguments for establishing the European Centre for Disease Prevention and Control6,7 (ECDC) in 2005. It was only natural that pandemic preparedness was one of the key activities of ECDC during its establishment year and thereafter. Upon a request of the European Council, in 2005 to 2007 ECDC conducted country visits in the EU and European Economic Area (EEA) countries. The objectives of these missions were to update the countries on the current influenza situation, to review the pandemic plans, and to increase the motivation to continue refining the plans.Reference Nicoll and Kreidl8-10
The ECDC developed, in close collaboration with the World Health Organization (WHO) regional office for Europe, self-assessment indicators and tools for member states to ensure that all relevant areas are covered in pandemic planning.11,12 These indicators and tools built on previous WHO guidance on preparedness planning were field-tested during the assessment visits.8,13 The ECDC self-assessment tool considers national and subnational levels of planning. Key areas covered are planning and coordination, situation monitoring and assessment, prevention and reduction of transmission, health system response, and communication. In September 2006, regional workshops were also organized to stress the importance of cross-sectorial collaboration, business continuity plans, medical countermeasures, and the need for implementation at subnational levels.9
The timing of the ECDC country visits from 2005 till 2007 was ideal, as all the visits were conducted before April 2009, when the influenza A (H1N1) pandemic commenced. During the country visits, teams consisting of national key stakeholders involved in preparedness planning, national experts from neighboring countries, and ECDC experts reviewed 30 countries’ plans.Reference Nicoll and Kreidl8-10 All countries had developed a plan consistent with international guidance.10 Political commitment was perceived and a high level of awareness and motivation was observed in all countries.9 Key areas identified for further work included integrating planning across government sectors and levels, making the plans operational at local level, and an EU-wide assessment of the effectiveness of medical countermeasures.9
The response to the 2009 pandemic underlined the need for a coordinated European response regarding availability of vaccines, vaccination strategy, regulatory processes for vaccines, information and communication to the public, global coordination, and multisectorial issues.14 These lessons learnt formed the basis of the joint ECDC/WHO guidance for pandemic plan revision.15 More specifically on pandemic vaccines, a conference was organized by the Belgian Presidency of the Council of the European Union in March 2010 that identified a number of lessons learnt in the fields of vaccine licensure, prioritization of target groups, importance of communication on pandemic vaccines, implementation of vaccination, and safety monitoring.Reference Hanquet, Van Damme and Brasseur16
Typically, influenza pandemic preparedness is a priority for European countries, as it is considered to be an event of high likelihood with high societal impact. A total of 17 member states shared their national risk assessments with the European Commission in the period of 2011 to 2013, and member states are required to provide the European Commission with summaries of the main elements of their national risk assessments,17 again, at the end of 2017.
The objective of this paper is to review the elements of pandemic preparedness in European countries’ plans by considering whether key areas for improvement18-20 that were identified before and during the evaluations of the 2009 pandemic have been addressed.
METHODS
A review of 28 national pandemic influenza plans was done for plans from EU and European Free Trade Association countries that were publicly available during July 19-22, 2016.Footnote a We assessed whether essential elements, as identified in lessons learnt exercises from the 2009 pandemic, were covered in the plans. A total of 42 items were identified and grouped into 14 overarching themes and a guiding question was developed for each item (Appendix 1). The themes are ordered to represent prepandemic preparedness followed by response aspects and, finally, the recovery phase. Aspects specific to influenza pandemic planning are covered, as well as some generic preparedness activities.
A team of 5 core reviewers analyzed the plans. Support was provided by native language speakers from the ECDC staff to help review those plans in other languages.
Scoring System
To measure the level of completeness, each plan was scored based on the number of items it covered. Hence, the highest score possible was 42 for a plan that covered all essential elements from the lessons learnt exercises. In order to reflect phraseology used in different languages and countries, the search terms from the item description were expanded to include alternative or synonymous terms. The reviewers scored permissively; for example, if an item was partially met it received a point and an explanation was given to interpret the partial compliance with the item. The items were not weighted and so all 42 items scored equally.
To assess the level of pandemic influenza preparedness at the EU level, the aggregated scores of all plans were used. Hence, this review does not aim to assess individual countries, rather it aims to shed light on the wider, EU level of preparedness.
In addition to reviewing how the plans scored against the 42-item list, the frequency of the individual items across the 28 plans was also assessed in order to identify specific elements of the plans that were common or not. Hence, “scoring” refers to the general status of the plan or a group of plans, whereas the frequency of an individual item or group of items pinpoints a specific section that was covered by the plan(s).
Stratified Results
We sought to explain determinants of the plans’ scoring by stratifying the results for 4 determinants: publication date, population size, health expenditure, and health management system type. These factors can give a better understanding of the scoring results for groups of countries.
Taking into account that not all national plans were revised after the 2009 pandemic, the plans were categorized as pre-2009 and post-2009. Plans published before or during the pandemic are categorized as pre-2009 and the remaining plans were categorized as post-2009. This review only considers the most recent version of a country’s national plan.
In addition, the results were stratified by population size,21 health care expenditure as share of gross domestic product (GDP),22 and health management system type.23 For population size and health expenditure, countries were grouped in quartiles with the first quartile being the lowest. The data for population size were from 2016, and data for health expenditure were from 2015 or the nearest possible year. For the health management systems, we used the typology published by the European Committee of the Regions, which identifies 4 types of systems: decentralized, partially decentralized, operatively decentralized, and centralized.23 This typology was made for all the EU member states in 2011, thereby excluding the European Free Trade Association countries (Norway, Switzerland, and Iceland) and Croatia, which joined the EU later. Countries included in the current study, but missing from the typology, are excluded from these stratified results, as grouping them was outside the scope of the current study. A one-way analysis of variance (ANOVA) was used to test scoring differences between the 4 types of health management systems.
Statistical significance was tested in Microsoft Excel 2011 (version 14.0) with a 2-tailed t test assuming equal variance and the null hypothesis was rejected when P <.05.
4 national plans were not reviewed due to being publicly unavailable (Cyprus, Malta) or legally expired (Lithuania), and Liechtenstein aims to implement the Swiss pandemic plan. Some countries, such as the United Kingdom, have a suite of pandemic preparedness documents, in which case only the main overarching framework or strategy was reviewed. We did not review pandemic plans of subnational organizational structures or from non–health care sectors, unless they were described in the main document.
RESULTS
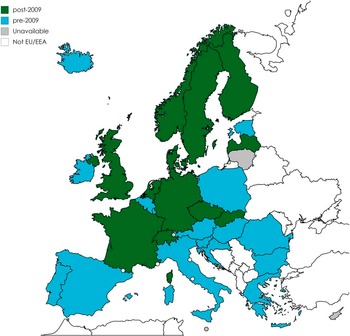
Twenty-eight EU/EEA countries have a publicly available pandemic preparedness plan. A majority of these countries’ pandemic influenza preparedness plans have not been revised since the 2009 pandemic. Plans published before 2009 were available for 16 countries and plans published after the 2009 pandemic were available for 12 (Figure 1).

Figure 1 Publicly Available Pandemic Influenza Preparedness Plans of 28 European Union / European Free Trade Association Member States in July 2016, Categorized by Plans Pulished Before (Blue) and After (Green) the 2009 Pandemic (map created with mapchart.net). Abbreviations: EU, European Union; EEA, European Economic Area.
The majority of national plans still reflect the 2005 WHO guidance,24 including those that have been reviewed following the publication of the updated interim WHO guidance25, 26 in 2013 and 2017.
In general, there is variation in the scope and approach of the national plans. Plans can be a discussion of strategy, an action plan, or combination of both; some plans are detailed and describe what will be done in response to a pandemic, whereas others are in the style of an action plan and describe what needs to be done to prepare for a pandemic. The plans range from one single document to a suite or an overarching strategy supported by operational documents and annexes, such as a separate communication strategy document. Despite the variation in plans, our methodology worked, as we tested for essential elements that any preparedness plan should include.
Several items were difficult to find in the plans, despite the reviewers knowing that these basic aspects were definitely addressed within national planning arrangements. This occurred when national level planners assumed that business-as-usual processes would be in place (eg, processes for monitoring adverse events or health care capacity). Another reason for not identifying foreseen items was that the information was provided in a separate plan.
Item Frequency and Pinpointing Specific Aspects of the Pandemic Plan
The frequency of the items in the plans varies with plans’ scores, which range from 11 to 40 out of a total of 42 (Figure 2). Items within the themes of “risk communication” and “command, control, coordination, and monitoring” scored the highest and items within the themes “special groups and settings” and “recovery and transition phase” scored the lowest.

Figure 2 Key elements (N = 42) of a national pandemic influenza preparedness plan, including frequency in the 28 reviewed plans. The highest-scoring items are highlighted in green and the lowest-scoring items are highlighted in red. For a description of the items, see Appendix, Table A1.
An exploration of key elements and themes that received high scores provides an understanding of widely accepted good practices. Nearly all plans (27 out of 28) included reference to a national planning committee, often with a description of the composition of the committee and its leadership. Many of the plans (27 out of 28) also refer to a strategy for use of antivirals; however, it was uncommon for the plans to describe a strategy of all the elements of procurement, distribution, storage, and policy. Still, this item received a high score due to our permissive scoring (eg, a plan that only mentions the procurement of antivirals and not all the other aspects listed in the item description would score a point for this item). A communication strategy and ensuring a method to coordinate communication with neighboring countries were both common aspects of the plans (27 out of 28 and 26 out of 28, respectively).
On the other hand, key elements that received low scores suggest thematic areas with less consensus or relevance in the plans. For example, only some (11 out of 28) plans make reference to specific actions for migrants, persons in transit, and hard-to-reach populations. Even fewer (10 out of 28) plans describe the roles of organizations in the third sector, with only one plan in particular describing the roles of nongovernmental organizations. Only a few of the plans describe triggers for determining the end of the pandemic (9 out of 28) and the recovery of mobilized human resources (7 out of 28).
Stratified by Publication Date of Pandemic Influenza Plan (Pre- and Post-2009)
The comparison of the plans that were published before (n = 16) and after (n = 12) the 2009 influenza pandemic shows that the post-2009 plans received higher scores. For some items (9 out of 42), the pre-2009 plans received slightly higher scores (items 2, 12, 16, 23, 28, 30, 33, 34, and 36). However, the biggest scoring differences are improvements in the post-2009 plans (Table 1). For example, a methodology to evaluate the pandemic mitigation measures was included in only 5 out of the 16 pre-2009 plans but was included in 10 out of the 12 post-2009 plans.
Table 1 Essential Elements in the Pandemic Influenza Preparedness Plans With the Largest Difference in Frequency of Mentions Between the Post-2009 and Pre-2009 Plans

Effects of Population Size
National pandemic influenza plans from countries falling within the first quartile in population size (ie, those with the smallest populations) received significantly lower scores compared to those in the other 3 quartiles (P <.05). The scores are determined by the inclusion of the 42 items (see Appendix, Table A1), and on average the plans from the 7 countries with the lowest population size include 20.3 of these items. For the other 3 quartiles, the average score is 32.3, 32.2, and 30.0, respectively, and they are not significantly different from each other (P >.05) (Figure 3).

Figure 3 Scores of National Pandemic Influenza Plans (N = 28) for Inclusion of Essential Elements, Stratified by Quartiles of Population Size
Effect of National Health Expenditure
National health expenditure, expressed as a percentage of the GDP, varies from 5.0 to 11.5 in the countries included in this review. Countries that are at the lower end of this range scored lower than countries with a higher portion of GDP spent on health. This trend can be seen in the scatterplot (Figure 4); however, the correlation is limited (R 2 = 0.12).

Figure 4 Correlation Between National Health Expenditure and National Pandemic Influenza Plan Scores in European Countries (N = 28)
Effect of Health Management System Type
The management of health systems in the EU member states, including the role of local and regional authorities, has been categorized by the EU and the Committee of the Regions.23 According to this categorization there are 4 groups: decentralized, centralized, partially decentralized (ie, countries that have several functions decentralized, but not legislation) and operatively decentralized (ie, countries where local and regional authorities have operational functions in the health management system). Countries with a more centralized health care system appear to have more comprehensive pandemic plans, while countries with a decentralized health management system score lower (Table 2). It could be relevant that the 3 countries categorized as having decentralized health management systems do not have publicly available post-2009 pandemic plans. Testing for the differences of the means of the 4 health management system types with a one-way analysis of variance (ANOVA) gives a nonsignificant result (P = .57).
Table 2 Frequency of Essential Elements in National Pandemic Influenza Plans Stratified by Type of Health Management System in Country

a According to categorization by the European Committee of the Regions.24
b Austria, Italy, Spain
c Belgium, Czech Republic, Denmark, Estonia, Finland, Germany, Hungary, Poland, Sweden
d Bulgaria, Latvia, Luxembourg, Netherlands, Romania, Slovakia, Slovenia, United Kingdom
e France, Greece, Portugal, Ireland
DISCUSSION AND CONCLUSIONS
Following the evaluation of the 2009 pandemic, the legal framework Decision No. 1082/2013/EU on serious cross-border threats to health has been adopted in the EU.27,28 This framework has a broader perspective on preparedness and response to public health emergencies, highlighting the all-hazard approach, including a joint procurement procedure for the purchase of medical countermeasures for serious cross-border threats to health. There is no public mapping of European Member States’ compliance with this legislative framework.Reference Speakman, Burris and Coker29
The legal framework on serious cross-border threats to health30 requires European countries to report every 3 years on preparedness planning,31 including International Health Regulations implementation, business continuity planning, and interoperability of plans between health and other sectors, as well as international collaboration in case of public health emergency.32 Influenza pandemics remain the most likely pandemic threat, with very serious health and socioeconomic consequences.Reference Saunders-Hastings, Reisman and Krewski33
The current review takes forward the work on the pandemic plans by describing the gaps, where the lessons learned14, Reference Hanquet, Van Damme and Brasseur16, 18-20 from the influenza A (H1N1) pandemic in 2009 remain to be included in the plans. We realize that plans are continuously being revised. For this current review we used the plans that were publicly available on the website of the country’s responsible authority in July 2016. The most recent versions of the plans can be found on the ECDC website.34
Reflecting on the available pandemic influenza preparedness plans shows 2 thematic areas that were mentioned least often in the plans: elements related to the recovery and transition phase, and special groups and settings. These are opportunities for improvement. Public health preparedness for special groups and vulnerable groups are elements not specific for pandemic preparedness and countries might have provisions for health care services to these groups in other legislative or strategic frameworks. The role of these vulnerable groups was also highlighted as a component of community preparedness.Reference Ramsbottom, O’Brien and Ciotti35 We note that these areas for improvement did not qualify among the 10 most urgent recommendations in a recent survey of EU preparedness experts.Reference Belfroid, Timen and van Steenbergen36
In addition, we found several opportunities for improvement related to coordination and communication. The handover of leadership from health to wider sector management was often unclear, even though this is important to ensure leadership continuity and a smooth response. Another opportunity for improvement we found is that few plans identified communication activities during the prepandemic phase, despite this being important to ensure all parties are aware of work underway and know the shared planning assumptions. A third issue is that while some plans allude to increasing health care capacity, very few describe the process to understand the baseline, though this may be covered in other documentation. This knowledge on the current status quo is essential to a successful response. Tools are available for countries to assess their preparedness and response capabilities.Reference MacDonald, Moen and St Louis37, 38
This manuscript identifies a number of planning deficits that remain in the national pandemic preparedness plans reviewed. As highlighted before, there are some common deficits; however, each plan has its own specific shortcomings. Countries planning to update their plan might want to prioritize which aspects to update first. To prioritize, one can reflect on the pandemic preparedness planning cycle that consists of 5 key elements of preparedness planning.15 These 5 key elements can provide guidance in prioritizing efforts to update pandemic plans. The prioritization provided by outbreak preparedness experts can also be helpful.Reference Belfroid, Timen and van Steenbergen36
Plans are organized in various manners, reflecting perhaps also the differences in framing the pandemic narrative as described by Holmberg and Lundgren.Reference Holmberg and Lundgren39 One specific manner of organizing the plan is not better; rather, in order to be effective, pandemic influenza preparedness must fit within existing overarching all-hazard plans, the national legal framework, and planning arrangements, and must serve well the existing organizational structures. From an EU perspective, the divergence in national plans could be seen as a challenge when wishing to coordinate across member states.Reference Holmberg and Lundgren39 In the current review we considered interoperability nationally and internationally as one of the essential elements that should be taken under consideration.
Countries face different challenges in the implementation and coordination of pandemic preparedness plans, which are likely due to regionalized decision-making in some countries (eg, federal states and autonomous regions). This is suggested by the fact that the few countries with decentralized health care structures scored slightly lower on average than other countries. A decentralized structure may require a lot of negotiations and consultations with local authorities as well as resolving issues of ownership and funding (including negotiations regarding human resources for the preparedness planning versus response). However, decentralization could also lead to having a hierarchical structure of emergency plans, whereas national or federal plans are strategic, leaving operational and tactical plans to the regions. The need for intersectorial collaboration for essential services and capacities can further complicate preparedness activities.
In 2005, when the bulk of pandemic preparedness was undertaken, many countries were of the view that stand-alone pandemic influenza plans were needed. Experiences from the 2009 pandemic and with other hazards (eg, Ebola, Middle East Respiratory Syndrome Coronavirus) have demonstrated the benefit of aligning plans for response to pandemic influenza more closely to existing arrangements that are used on a more frequent basis. An all-hazards approach is also taken on by the WHO interim guidance for pandemic influenza risk management.26 This ensures that responders are familiar with response arrangements and that the best outcomes should be achieved for patients and the public. Whilst a pandemic is not the same as a seasonal outbreak of influenza or common situations experienced during winter due to cold weather, such as norovirus circulation, there is certainly learning from both of these scenarios that can be built upon to ensure robust pandemic response.
Our results suggest that the limited resources available for planning at national level, due to the size of the country or low health expenditure, appear to be factors influencing the contents of the pandemic plans (Figures 3 and 4). One can argue that a small country does not need to have the same level of complexity in the plans as a larger country does due to simpler structures and planning and response processes in the country. It might be interesting to investigate if the plans have been supported by financial mechanisms for funding specific activities; however, this was beyond the scope of the current study.
The plans published after 2009 appear to have included more of the identified essential elements than those published before 2009. We suggest this is due to the lessons learnt and evaluation process undertaken in countries and at the EU and global levels and is part of a continuously evolving planning process. Similar results suggesting temporal improvement of plans were shown by Moen and colleaguesReference Moen, Kennedy and Cheng40 among 40 countries between 2008 and 2010. However, it should be noted that in our analysis we are not comparing pre- and post-pandemic plans originating from the same countries. It is likely that the countries that have had the resources to update their plans will also be more comprehensive in their plans and they may have had a more comprehensive plan prior to the post-2009 revision.
It was expected that plans updated and published following the 2009 pandemic would contain more of the key elements than those written before the pandemic. However, conversely, 9 elements are more common in plans written before the 2009 pandemic. This may be because post-2009 pandemic response arrangements are spread over numerous documents that have not been included in the analysis. Another clarification could be that post-2009 plans follow the older WHO 2005 planning guidance.
We stress that the review of written plans does not reflect the actual preparedness level, as the level of preparedness entails much more than the existence of a plan. Also, Meeyai and colleaguesReference Meeyai, Cooper and Coker41 did not find that the completeness of plans in 19 European countries was associated with measures of the pandemic intensity during 2009. We recognize that the process of developing the plan is often as important as the resulting published documentation, or even more. As for the review of the written plans, we note some limitations. The level of detail per item was not assessed. However, the level of detail of a plan is probably less important than the completeness of a plan (ie, covering all essential elements), as flexible plans are needed to respond to the next pandemic of which the parameters are unknown.Reference Napoli, Fabiani and Rizzo42 We also point out that our baseline is the WHO guidance from 2009,13 which could clarify why countries pre-2009 scored lower in this review.
The authors are aware that a lot of activities take place at different levels in Europe with regards to pandemic preparedness, such as simulation exercises and after action reviews. Also, the Joint External Evaluations that have a much wider scope than pandemics are recommended as part of the international health regulations to incorporate—in addition to self-assessment—also a peer review with domestic and external experts. Indeed, these activities increase the capacity to respond, but it is difficult to obtain evidence on these activities until lessons learned are published. Therefore, we recommend for lessons learned and good practices to be exchanged more frequently among key stakeholders.
Acknowledgments
The authors would like to thank the colleagues at the European Centre for Disease Prevention and Control (ECDC) for helping translate the national pandemic influenza preparedness plans: Kaja Kaasik Aaslav, Agne Bajoriniene, Dragoslav Domanovic, Katrin Leitmeyer, Otilia Mårdh, Paulina Nakielny, Diamantis Plachouras, Vladimir Prikazsky, and Signe Rirdance.
Appendix
Table A1 Key Elements of a National Pandemic Influenza Preparedness Plan (42 Items).