There is evidence that maximum efficacy for typical antipsychotics occurs at 70-80% of dopamine receptor occupancy and that these levels can be achieved at doses substantially lower than has previously been thought necessary (Reference McEvoy, Hogarty and SteingardMcEvoy et al, 1991; Reference Stone, Garver and GriffithStone et al, 1995; Reference Kapur, Remington and JonesKapur et al, 1996). Doses in excess of these result in enhanced side-effects and can be especially hazardous when more cardiotoxic drugs are used. The benefits of using a potentially toxic high dose regime have therefore been increasingly questioned (Reference ThompsonThompson, 1994; Reference LaderLader, 1997). Early reviews and audits of antipsychotic prescribing used chlorpromazine equivalents (CPZE) to evaluate total antipsychotic dose (Reference Peralta, Cuesta and CaroPeralta et al, 1994; Reference Warner, Slade and BarnesWarner et al, 1995; Reference Krasucki and McFarlaneKrasucki & McFarlane, 1996; Reference Morgan, Haw and AngierMorgan et al, 1996) and high doses were defined as those in excess of 1000 mg CPZE/day.
There are a number of theoretical and practical problems in using CPZEs which include:
-
(a) Published conversion tables become out of date quickly and are not available in all clinical settings.
-
(b) The range of values of equivalent doses quoted in the literature can differ by 500% (Reference Dewan and KossDewan & Koss, 1995).
-
(c) Published conversion factors are based on equivalence of antipsychotic effect, toxicity can have a different dose-response relationship for individual drugs.
-
(d) Dose-response relationships may be non-linear.
-
(e) The risks associated with high-dose therapy do not stem from the antipsychotic activity of the drug but from the toxic side-effects.
-
(f) Different receptor occupancy profiles of atypical antipsychotics may make the use of CPZEs misleading.
Toxicity studies for new drugs are carried out at an early stage of development and include acute, sub-acute and chronic toxicity evaluations. Data from these studies are used in determining the upper dose range of a drug though the upper limit may be changed as new evidence on toxicity emerges, as was the case with pimozide. The potency of a drug is quite different and is a measure of the dilution at which it causes a specified effect, usually measured in an in vitro experimental system. The British National Formulary (BNF; BNF, 1995) is updated twice a year and BNF maximum doses are unequivocal, and generally based on toxicity rather than efficacy data. The BNF maximum has, therefore, been suggested as a better method for calculating total antipsychotic dose (Reference Yorston and PinneyYorston & Pinney, 1997). There have been no published comparisons of the two methods of identifying high-dose patients. The current study sought to do this in a naturalistic setting and explore differences between the high-dose groups identified by each method.
The study
The study was carried out at Amersham Hospital, South Buckinghamshire between July and October 1995. The prescription charts for all in-patients were examined over a 14-week period in two general and two old age psychiatry wards, in two community-based rehabilitation units and for all patients attending depot clinics run by community psychiatric nurses. The full methodology and results have already been described (Reference Yorston and PinneyYorston & Pinney, 1997). The antipsychotic dose was calculated in CPZEs using the conversion table in Bazire (Reference Bazire1995), and as a percentage of the BNF maximum recommended dose. For patients prescribed more than one antipsychotic, the CPZEs or percentages were summed to give a total dose also expressed in CPZEs or as a percentage. Trifluoperazine has no recommended upper limit in the BNF, so a daily dose of 45 mg was chosen for the purposes of this study. High doses were defined as more than 100% of the BNF maximum or more than 100 mg CPZE/day.
Findings
Of the 258 patients who had been prescribed antipsychotics during the study period, 30 were identified as receiving either more than 100% of the BNF maximum or more than 1000 mg CPZE/day. Twelve of these patients taking high doses were identified by both methods, six were identified by the percentage BNF maximum method only, and another 12 by the CPZE method only. The concordance between the two methods for all patients was 93%.
There is no simple linear relationship between CPZEs and percentage BNF maximum for high-dose patients (see Fig. 1). The Spearman's rank correlation was 0.241.
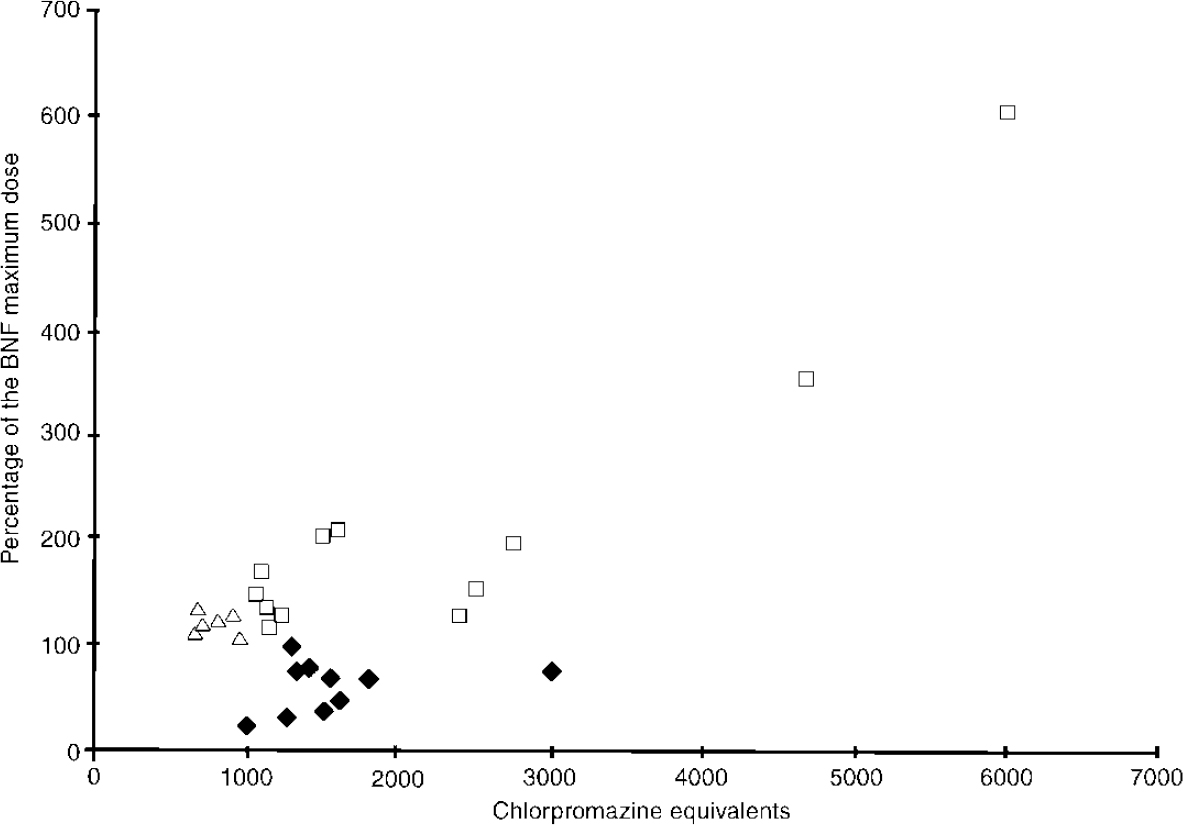
Fig. 1 Percentage of the British National Formulary (BNF) maximum compared with chlorpromazine equivalents; ⧫, Group A; □, Group B; Δ, Group C.
These patients can be divided into three groups:
Group A
Those in the bottom right-hand portion of the graph who received in excess of 1000 mg CPZE/day but were below the BNF maximum dose.
Group B
Those in the top right-hand portion of the graph who received high doses by both methods.
Group C
Those in the top left-hand portion of the graph who received doses in excess of the BNF maximum recommended dose yet were below 1000 mg CPZE/day.
The drugs prescribed to the patients falling into these groups are summarised in Table 1.
Table 1. Range of antipsychotics prescribed for patients taking high doses
| Number of patients | |||
|---|---|---|---|
| Choice of therapy | Group A (n = 12) | Group B (n = 12) | Group C (n = 6) |
| Depot | |||
| Flupenthixol decanoate alone | 6 | — | — |
| Flupenthixol decanoate plus different oral | 3 | — | — |
| Fluphenazine decanoate alone | — | 1 | — |
| Fluphenazine decanoate plus different oral | — | 3 | — |
| Haloperidol decanoate alone | — | — | 1 |
| Haloperidol decanoate plus different oral | — | 1 | — |
| Zuclopenthixol decanoate alone | — | — | — |
| Zuclopenthixol decanoate plus same oral | — | — | 2 |
| Zuclopenthixol decanoate plus different oral | — | 5 | 2 |
| Oral | |||
| One antipsychotic | 2 | — | — |
| Two antipsychotics | 1 | 2 | 1 |
Comment
The majority of patients were prescribed relatively low doses of antipsychotic medication, well below both 1000 mg CPZE/day and the BNF maximum dose. The correlation between the percentage of the BNF maximum dose and CPZEs was close for some drugs and preparations, for example, thioridazine and oral flupenthixol. For others large differences existed, such as oral haloperidol and flupenthixol decanoate. In practice, for the majority of patients on low or moderate doses, these differences had little impact on whether they were included in the high-dose group and therefore subject to high dose monitoring guidelines.
For the minority of patients receiving doses in the higher range, however, the method used for calculating total daily dose was important. The BNF maximum method was more sensitive for some drugs (Group C) and the CPZE method was apparently more sensitive for others (Group A). Nine of the 12 patients in Group A received flupenthixol decanoate depot. Only three of these were prescribed an additional regular oral antipsychotic - suggesting that they were relatively well maintained. One patient in this group received two different oral antipsychotics and two patients were maintained on clozapine alone.
Of the six Group C patients, five were prescribed depot medication and four of these also received other regular oral antipsychotics.
In spite of the success of the new atypical antipsychotics in the treatment of schizophrenia, there will remain a number of patients who, for reasons of adherence, response or side-effects, will continue to require high-dose depot treatment. When determining optimal therapy for these patients high potency preparations should be considered in order to minimise the risks of toxicity. Although the question of which antipsychotic to use in patients with refractory illnesses was not designed to be addressed by this study, consideration of BNF maximum dose and chlorpromazine equivalence has highlighted flupenthixol decanoate as one of the least toxic, most potent depot preparations available. Despite BNF warnings that flupenthixol has an activating effect and should not be given to patients who are acutely disturbed, at higher doses it is known to have a sedative effect (Reference GunbyGunby, 1974; Reference GerlachGerlach, 1977). It has the added advantage of lacking significant cardiotoxicity.
The method of expressing total antipsychotic dose as a percentage of the BNF maximum was easy to understand and calculate and recent copies of the BNF were widely available. It helps ensure patients at risk of antipsychotic toxicity are easily identified such that monitoring guidelines can be followed.





eLetters
No eLetters have been published for this article.