Introduction
Mild Cognitive Impairment (MCI) may be conceptualized as an intermediate stage between dementia and healthy ageing in which activities of daily living are preserved (Arnáiz & Almkvist, Reference Arnáiz and Almkvist2003). While most commonly associated with Alzheimer’s disease (AD), MCI can be caused by other diseases and evidence-based recommendations for diagnosis of prodromal dementia with Lewy bodies (MCI-LB) have recently been published (McKeith et al., Reference McKeith, Ferman, Thomas, Blanc, Boeve, Fujishiro and Postuma2020). Neuropsychological impairments in dementia with Lewy bodies (DLB) and AD differ, but few well-controlled comparative studies of sufficient sample size have been done in the MCI stages (see Ciafone, Little, Thomas, & Gallagher, Reference Ciafone, Little, Thomas and Gallagher2020; Hemminghyth, Chwiszczuk, Rongve, & Breitve, Reference Hemminghyth, Chwiszczuk, Rongve and Breitve2020 for reviews). In MCI-LB, deficits have been reported predominantly in domains impaired in DLB (i.e., visuospatial function, attention, executive function; Donaghy, Taylor, et al., Reference Donaghy, Taylor, O’Brien, Barnett, Olsen, Colloby and Thomas2018; Donaghy, O’Brien, & Thomas, Reference Donaghy, O’Brien and Thomas2015) although other studies suggest a broad (Kemp et al., Reference Kemp, Philippi, Phillipps, Demuynck, Albasser, Martin-Hunyadi and Blanc2017) and heterogeneous (Hemminghyth et al., Reference Hemminghyth, Chwiszczuk, Rongve and Breitve2020) range of cognitive deficits.
In a recent review, a third of neuropsychological outcome variables from six primary studies differed significantly between MCI-LB and MCI due to AD, suggesting possible dissociation, although most studies were small or lacked biomarker data to support diagnoses (Ciafone et al., Reference Ciafone, Little, Thomas and Gallagher2020). Verbal learning and memory appeared less affected in MCI-LB (Ciafone et al., Reference Ciafone, Little, Thomas and Gallagher2020) in line with AD’s pronounced memory encoding deficits (Lange et al., Reference Lange, Bondi, Salmon, Galasko, Delis, Thomas and Thal2002; Martin, Brouwers, Cox, & Fedio, Reference Martin, Brouwers, Cox and Fedio1985). However, when compared to matched test norms, some studies suggested that substantial numbers of MCI-LB present with verbal memory impairment (Ferman et al., Reference Ferman, Smith, Kantarci, Boeve, Pankratz, Dickson and Petersen2013; Kemp et al., Reference Kemp, Philippi, Phillipps, Demuynck, Albasser, Martin-Hunyadi and Blanc2017), indicating amnesia should not be taken as a reliable discriminator of prodromal AD. Memory impairment is especially present in DLB patients with markers of concurrent AD-type pathology using cerebrospinal fluid (CSF) or post-mortem neuropathology (Howard et al., Reference Howard, Irwin, Rascovsky, Nevler, Shellikeri, Tropea and Siderowf2021; Lemstra et al., Reference Lemstra, De Beer, Teunissen, Schreuder, Scheltens, Van Der Flier and Sikkes2017). There was also heterogeneity within domains: subtypes generally differed on some but not all measures of a given domain within a single study (Ciafone et al., Reference Ciafone, Little, Thomas and Gallagher2020).
In cognitive psychology, multicomponential approaches fractionate the cognitive system into “domain-specific” components with separate functions and capacities (e.g., verbal and visuospatial) and “domain-general” resources, such as processing speed and executive functions (Logie, Reference Logie2011). Components work in parallel to complete complex tasks and scaffold memory performance (Brown & Wesley, Reference Brown and Wesley2013). Neuropsychological studies of hierarchical cognitive organization, as well as prominent resource models of age-related cognitive decline, postulate that impairments observed in domain-specific tasks, for example, delayed verbal or visuospatial memory, can be the secondary result of domain-general, primary impairments (Kemp et al., Reference Kemp, Philippi, Phillipps, Demuynck, Albasser, Martin-Hunyadi and Blanc2017; Luszcz & Bryan, Reference Luszcz and Bryan1999; MacDonald, Hultsch, Strauss, & Dixon, Reference MacDonald, Hultsch, Strauss and Dixon2003). Executive function and processing speed have both been proposed as such explanatory domain-general impairments in aging and disease. Consequently, memory deficits in MCI-LB may be underpinned by core, “domain-general” processing dysfunction, in contrast to the memory storage impairments characteristic of MCI-AD (Ciafone et al., Reference Ciafone, Little, Thomas and Gallagher2020; Jicha et al., Reference Jicha, Schmitt, Abner, Nelson, Cooper, Smith and Markesbery2010; McKeith et al., Reference McKeith, Ferman, Thomas, Blanc, Boeve, Fujishiro and Postuma2020). DLB is associated with slower processing speed than mild AD (Breitve et al., Reference Breitve, Chwiszczuk, Brønnick, Hynninen, Auestad, Aarsland and Rongve2018; Cagnin et al., Reference Cagnin, Bussè, Gardini, Jelcic, Guzzo, Gnoato and Caffarra2015), and the largest overall deficits in MCI-LB were recently reported as processing speed and executive function (Kemp et al., Reference Kemp, Philippi, Phillipps, Demuynck, Albasser, Martin-Hunyadi and Blanc2017).
There have been few studies of the neuropsychology of clinically-defined MCI-LB when compared to MCI-AD and, to our knowledge, no prospective studies of MCI-LB and healthy comparison subjects that use biomarkers identified in recent consensus diagnostic criteria. The present study was designed to examine the neuropsychological profile of MCI-LB compared with MCI-AD and healthy older people in a comprehensively assessed prospective cohort, with diagnosis supported by two validated biomarkers of Lewy body disease and in line with the recently published MCI-LB research criteria (McKeith et al., Reference McKeith, Ferman, Thomas, Blanc, Boeve, Fujishiro and Postuma2020). Specifically, we hypothesized: 1) greater deficits in visuospatial and executive function and slowed speed of processing in MCI-LB relative to MCI-AD and controls; 2) poorer performance by MCI-AD relative to MCI-LB and controls in delayed verbal recall, in line with the amnestic profile of AD; and 3) domain-specific neuropsychological impairments in MCI are underpinned by the domain-general processing resources of executive function and processing speed.
Method
Participants, diagnosis, and clinical assessments
Patients over 60 years old with a clinical diagnosis of MCI in Memory Services were recruited in the north east of England. Control participants were recruited from relatives, friends, and a volunteer database and matched overall to the MCI groups on age. Patients were identified who had symptoms which may be related to prodromal DLB, such as autonomic, visual or olfactory disturbances, or any indications of core features of DLB. Participants were excluded if there was evidence of clinical stroke or frontotemporal atrophy on magnetic resonance imaging (MRI), Parkinson’s disease (PD) established at least a year before cognitive decline, or severe mental illness (current major depression, bipolar disorder, schizophrenia). The study received ethical approval from the National Research Ethics Service Committee North East–Newcastle & North Tyneside 2 (Research Ethics Committee Identification Number 15/NE/0420). Subjects were provided written informed consent after receiving a complete description of the study and were treated in accordance with the ethical standards of the Helsinki Declaration.
After consent all participants underwent a research clinical diagnostic assessment and neurological examination by a medical doctor (RD, SL) and were offered imaging for biomarkers (123I-FP-CIT SPECT, cardiac MIBG) as detailed elsewhere (Firbank et al., Reference Firbank, O’Brien, Durcan, Allan, Barker, Ciafone and Lloyd2020; Roberts et al., Reference Roberts, Donaghy, Lloyd, Durcan, Petrides, Colloby and Firbank2020). FP-CIT and MIBG scans were rated blind to clinical information. All had MRI brain scans which were consistent with their diagnoses. At the time of the scans and clinical assessment the Movement Disorder Society (MDS) Unified Parkinson’s Disease Rating Scale (UPDRS-III; Goetz et al., Reference Goetz, Tilley, Shaftman, Stebbins, Fahn, Martinez-Martin and Dodel2008) motor subsection, Epworth Sleepiness Scale (ESS; Johns, Reference Johns1991), and Geriatric Depression Scale (GDS; D’Ath, Katona, Mullan, Evans, & Katona, Reference D’Ath, Katona, Mullan, Evans and Katona1994) were administered to study subjects. The Instrumental Activities of Daily Living (IADL; Lawton, Brody, & Médecin, Reference Lawton, Brody and Médecin1969) scale, North-East Visual Hallucinations Inventory (NEVHI; Mosimann et al., Reference Mosimann, Collerton, Dudley, Meyer, Graham, Dean and Clarke2008), Neuropsychiatric Inventory (NPI; Cummings et al., Reference Cummings, Mega, Gray, Rosenberg-Thompson, Carusi and Gornbein1994), Clinician Assessment of Fluctuation (CAF; Walker et al., Reference Walker, Ayre, Cummings, Wesnes, McKeith, O’brien and Ballard2000), and Dementia Cognitive Fluctuation Scale (DCFS; Lee et al., Reference Lee, McKeith, Mosimann, Ghosh-Nodial, Grayson, Wilson and Thomas2014) were administered to informants of patients. Clinical Dementia Rating scale (CDR; Hughes, Berg, Danziger, Coben, & Martin, Reference Hughes, Berg, Danziger, Coben and Martin1982) and Cumulative Illness Rating Scale for Geriatrics (CIRS-G; Miller et al., Reference Miller, Paradis, Houck, Mazumdar, Stack, Rifai and Reynolds1992) were completed on the basis of the clinical history and other research assessments. Premorbid IQ was estimated using the National Adult Reading Test (Nelson & Willison, Reference Nelson and Willison1991). All participants were reviewed annually at which the clinical diagnostic assessments and rating scales were repeated.
As detailed elsewhere (Thomas et al., Reference Thomas, Donaghy, Roberts, Colloby, Barnett, Petrides and McKeith2019), at baseline and annually a three-person consensus clinical panel of experienced Board Certified old age psychiatrists (AJT, PCD, JPT) independently reviewed clinical notes taken from the research assessment and confirmed diagnoses. This consensus panel method has previously been validated against autopsy and is recognized by regulatory authorities as the clinical gold standard for living patients (McKeith et al., Reference McKeith, Ballard, Perry, Ince, O’brien, Neill and Thompson2000; McKeith et al., Reference McKeith, O’Brien, Walker, Tatsch, Booij, Darcourt and Volterrani2007). A diagnosis of probable MCI-LB was given if a patient had two or more core Lewy body symptoms (with positive or negative scan results) or one core symptom in addition to a positive FP-CIT or MIBG scan, in accordance in the current consensus research criteria for diagnosis of probable MCI-LB (McKeith et al., Reference McKeith, Ferman, Thomas, Blanc, Boeve, Fujishiro and Postuma2020). Patients meeting criteria for possible MCI-LB (one core symptom or just one abnormal scan) were not included in this analysis. The clinical diagnosis of MCI-AD was made as set out in the criteria from Albert et al. (Reference Albert, DeKosky, Dickson, Dubois, Feldman, Fox and Phelps2011). Firstly, subjective and objective cognitive decline consistent with AD were established, along with generally maintained independence of function in everyday life. As directed in the criteria, other causes were then excluded including evidence of vascular cognitive impairment, primary progressive aphasia, and behavioural variant FTD, along with Lewy body disease. We had access to participant medical records and imaging results with their consent, allowing us to identify and exclude cases of probable vascular cognitive impairment.
Control subjects were free of subjective memory complaints or such concerns from others, evidence of any movement disorder, were not on antidementia or anti-PD drugs, and had Mini-Mental State Examination (MMSE) ≥26 and normal MRI scans. The present study reports comparison of probable MCI-LB (henceforth MCI-LB) with MCI-AD and controls, in line with previous work in dementia which has compared probable DLB with AD dementia.
Neuropsychological assessment
A comprehensive neuropsychological assessment was administered by a trained researcher in participant homes or a clinical research facility over the course of two or more days. Tasks included the Addenbrooke’s Cognitive Examination-Revised (ACE-R; Mioshi, Dawson, Mitchell, Arnold, & Hodges, Reference Mioshi, Dawson, Mitchell, Arnold and Hodges2006), a 100-point cognitive screening test from which MMSE (Folstein, Folstein, & McHugh, Reference Folstein, Folstein and McHugh1975) score was derived, Corsi Blocks (Corsi, Reference Corsi1972), a computerized adaptation of the Visual Patterns Task (VPT; Della Sala, Baddeley, Gray, & Wilson, Reference Della Sala, Baddeley, Gray and Wilson1997), Modified Taylor Complex Figure (MTCF; Hubley & Tremblay, Reference Hubley and Tremblay2002), Graded Naming Test (GNT; Warrington, Reference Warrington1997), Rey Auditory Verbal Learning Test [RAVLT; outcome measures: Maximum (most words recalled in any trial 1–5), Learning (trial 5–trial 1), Immediate Recall, Long Delay (30 minutes), %Long Delay (percent of Maximum recalled); Rey, Reference Rey1964], Trail-Making Test A and B (Trails A and B; Reitan, Reference Reitan1955), Digit Span (Kaplan, Fein, Morris, & Delis, Reference Kaplan, Fein, Morris and Delis1991), FAS Test of phonemic verbal fluency (Borkowski, Benton, & Spreen, Reference Borkowski, Benton and Spreen1967), Stroop Test [word (W) and color-word (CW); Golden, Reference Golden1978] and Simple Reaction Time (Ballard et al., Reference Ballard, O’Brien, Gray, Cormack, Ayre, Rowan and Walker2001). The DSST (Wechsler, Reference Wechsler1944), a sensitive measure of processing speed, was administered along with test variants Symbol Copy (Kaplan et al., Reference Kaplan, Fein, Morris and Delis1991) and Error Check (Joy, Fein, Kaplan, & Freedman, Reference Joy, Fein, Kaplan and Freedman2000). Similar in procedure to the DSST, the two variants enable statistical delineation of DSST’s cognitive and psychomotor task demands (Van der Elst, van Boxtel, van Breukelen, & Jolles, Reference Van der Elst, van Boxtel, van Breukelen and Jolles2006). In Symbol Copy, participants simply copy each symbol in the grid into an empty box directly below it as fast as possible, without consulting a coding key as in DSST, thereby isolating the DSST’s graphomotor components. Error Check, conversely, involves scanning a completed DSST for errors in relation to a key and marking any with a pencil slash, thereby capturing visual scanning speed with minimal psychomotor demands. Cognitive scores other than the ACE-R and MMSE were not used for patient diagnoses.
Data cleaning and analysis
Following Little’s Missing Completely at Random Test (MCAR) (χ 2[451] = 480.3, p = .164), missing values were replaced using expectation–maximization (Statistical Package for the Social Sciences, V. 21; IBM SPSS Corp., Reference Corp2013). Performance by group was compared using multivariate analyses of variance (MANOVA) for each cognitive domain followed by independent samples t or Mann–Whitney U tests, where appropriate. Effect sizes (g) and 95% confidence intervals were bias-corrected (Hedges & Olkin, Reference Hedges and Olkin1985). As interindividual variation in performance can be great, MCI group scores were also computed as percentile rankings. Based on control group data, the percentage of each MCI group that scored at or below the 5th and 16th percentiles (1.65 and 1.0 SDs below control means, respectively) was calculated. Variables differing significantly between MCI subtypes were also entered into a stepwise discriminant analysis to determine maximal differentiation between subtypes, excluding controls.
Domain composite scores were computed as average control-adjusted z-scores using representative outcome measures: executive function (FAS, Trails Ratio), verbal learning and memory (RAVLT Maximum and Short Delay) and visuospatial working memory (Corsi Blocks, VPT). Delayed memory was measured using RAVLT Long Delay (verbal delayed memory), and MTCF %Recall (visuospatial delayed memory). A series of hierarchical multiple regressions (Enter method) run separately for MCI-AD/controls and MCI-LB/controls tested the mediating role of domain-general resources [executive function (FAS, Trails Ratio) and processing speed (DSST)] on domain-specific impairments (visuospatial and verbal learning and delayed memory) following a statistical procedure similar to Nebes et al. (Reference Nebes, Butters, Mulsant, Pollock, Zmuda, Houck and Reynolds2000). In all models, variance associated with age and estimated premorbid IQ [National Adult Reading Test (NART)] was initially accounted for in Step 1 and retained in subsequent models if significant. The proportion of diagnosis-related variance in the domain-specific measures was first determined by entering “group” (control, MCI-AD or MCI-LB) as a predictor variable (Step 2). Next, models were run in which the domain-general variables of interest (processing speed and executive function) were entered iteratively at Step 2 before group (Step 3). The variance explained (ΔR 2) by group in these two models were then compared to calculate “group-associated variance explained” as the percent decrease in variance explained by group when it is entered at Step 3 (after processing speed or executive function) versus at Step 2. Group-associated variance explained therefore quantifies the domain-general predictor’s (processing speed or executive function) mediation of the deficit due to MCI subtype status in a particular domain-specific measure (Nebes et al., Reference Nebes, Butters, Mulsant, Pollock, Zmuda, Houck and Reynolds2000). Lastly, multiple regressions were run separately by group to predict DSST performance by its subtests (Symbol Copy, Error Check) and gross motor impairment (UPDRS).
Results
One hundred and fifty four participants consented to the study, including n = 34 controls with complete study data. Of n = 120 MCI, n = 16 withdrew for various reasons (see online supplement fig. A1). Patients were diagnosed as probable MCI-LB (n = 44), MCI-AD (n = 39) or possible MCI-LB (n = 21; as earlier, these were excluded from further analyses). MCI subtypes were equivalent on age, premorbid IQ and global cognition (MMSE). MCI-LB consisted of more males and showed greater severity on neuropsychiatric and functional measures (UPDRS, ESS, CAF, GDS, CIRS-G, IADL; see Table 1). Controls with abnormal MIBG (n = 2) or FP-CIT (n = 2) had normal clinical presentation, intact cognition and no other evidence of LB disease and were retained as healthy comparison subjects.
Table 1. Demographics and clinical scales of MCI with Lewy bodies (MCI-LB; n = 44), MCI due to Alzheimer’s disease (MCI-AD; n = 39) and controls (n = 34), with significance (p) of between-group comparisons of MCI subtypes

Parametric data reported as mean and standard deviation (SD), nonparametric data reported as median and interquartile range (IQR). Mann–Whitney U tests, t, and Chi-squared tests used depending on the nature of the data. Bold denotes p < .05.
MMSE: Mini-Mental State Examination; NART: National Adult Reading Test; CIRS-G: Cumulative Illness Rating Scale for Geriatrics; UPDRS: Unified Parkinson’s Disease Rating Scale (MDS Revision); NEVHI: North-East Visual Hallucinations Interview; ESS: Epworth Sleepiness Scale; DCFS: Diagnostic Cognitive Fluctuations Scale; CAF: Clinician Assessment of Fluctuation; GDS: Geriatric Depression Scale; NPI: Neuropsychiatric Inventory; IADL: Instrumental Activities of Daily Living Scale; CDR: Clinical Dementia Rating Scale.
Informant based scales MCI-AD n = 37, NPI MCI-AD n = 36; MCI-LB n = 40, NEVHI MCI-LB n = 41.
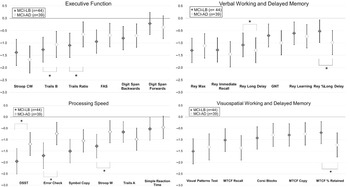
Overall neuropsychological performance
MANOVA of the four principal neuropsychological domains demonstrated statistically significant group differences: executive function, F(12,170) = 5.35, p < .001; Wilk’s Λ = .527, partial η 2 = .27, processing speed, F(12,166) = 4.35, p < .001; Wilk’s Λ = .579, partial η 2 = .24, visuospatial, F(10,142) = 3.36, p = .001; Wilk’s Λ = .654, partial η 2 = .19, and verbal learning and memory, F(12,208) = 5.32, p < .001; Wilk’s Λ = .585, partial η 2 = .24. As expected, both MCI groups scored significantly below controls on all neuropsychological measures (ps < .01) except Forward Digit Span, χ 2(2) = 3.05, p = .218, and Simple Reaction Time (SRT) mu, χ 2(2) = 2.34, p = .310. Effect sizes (g) and 95% confidence intervals are presented in forest plots by domains (Figure 1), showing MCI differences relative to controls and a pattern of divergence between MCI subtypes, particularly in processing speed and delayed recall tasks, both visuospatial and verbal. MCI-LB performed significantly worse than MCI-AD on Trails B (p = .03, g = .55), Trails Ratio (A/B; p = .04, g = .51), DSST (p = .04, g = .48), Error Check (p < .001, g = .75), and Stroop W (p = .01, g = .54). MCI-AD performed significantly below MCI-LB on delayed verbal recall (RAVLT Long Delay, p = .04, g = .37; RAVLT %Long Delay, p = .01, g = .48) and delayed visuospatial recall (MTCF %Recall, p = .01, g = .62).

Fig. 1. Bias-adjusted effect sizes and 95% CI (error bars) of control-centered (n = 34) performance on neuropsychological tasks by MCI due to Alzheimer’s disease (MCI-AD; n = 39) and MCI with Lewy bodies (MCI-LB; n = 44), plotted by domain (Executive Function, Processing Speed, Verbal Learning and Memory, Visuospatial Working and Delayed Memory). Significant differences between MCI subtypes indicated with asterisk (*).
The majority of MCI-LB patients performed at or below the 16th percentile (1 SD or more below control means) on processing speed measures (84.1% on Trails B, 88.6% DSST; see online supplement). In the visuospatial domain, percentile standings below the 5th percentile were similar between subtypes in visuospatial working memory (VPT; MCI-LB 58.8%, MCI-AD: 53.8%) and figure drawing (MCI-LB: 40.9%, MCI-AD: 48.7%). However, a higher proportion of the MCI-AD group were impaired at the 5th percentile (1.65 SDs) in visuospatial delayed recall (MTCF %Recall; MCI-AD: 43.6%, MCI-LB: 29.5%) and verbal delayed recall (RAVLT Long Delay; MCI-AD: 59.0%, MCI-LB: 27.3%).
Stepwise discriminant analysis excluding controls was applied to variables differing significantly between MCI subtypes. The model resulted in three variables in three steps: Error Check, F(1,81) = 9.91, p = .002, MTCF %Recall, F(2,80) = 9.84, p < .001, and Trails Ratio, F(3,79) = 8.80, p < .001. MTCF %Recall had the highest standardized discriminant function coefficient (.74), followed by Error Check (−.62) and Trails Ratio (0.54). The canonical loadings were ≥.30 for all neuropsychological variables entered into the analysis except RAVLT Long Delay and %Recall, suggesting a combination of visuospatial memory and executive-weighted cognitive processing. The discriminant function correctly classified subtype in 65.1% of all MCI cases, with 72.7% specificity and 56.4% sensitivity.
Analysis of the hierarchical organization
In controls, no significant relationships were observed in simple correlational assessment of the relationship between processing resources (DSST, executive function) and visuospatial and verbal variables (working memory and delayed memory; all ps > .05). In MCI-LB, DSST was correlated with visuospatial working memory (r s = .524, p < .001) and delayed visuospatial memory (r s = .366, p = .015). In MCI-AD, executive function and visuospatial working memory were correlated, (r s = .331, p = .039), and DSST was correlated with all working and delayed memory measures: visuospatial working memory (r s = .394, p = .013), delayed visuospatial memory (r s = .405, p = .010), verbal learning and memory (r s = .444, p = .005), and delayed verbal memory (r s = .366, p = .022).
Processing speed (DSST) was a stronger predictor of group-associated variance in verbal learning and memory, visuospatial working memory, and delayed visuospatial memory than executive function in both the MCI-LB/controls and MCI-AD/controls analyses (Table 2). In delayed verbal memory, processing speed explained 53.9% and 29.0% of group-associated variance in MCI-LB/controls and MCI-AD/controls, respectively, but the relationship with executive function was not significant in either grouping (p = .203, p = .082, respectively). If entered after executive function, processing speed also explained additional unique variance in visuospatial working memory, verbal learning and memory, and delayed visuospatial memory scores in both groups. However, when order of entry was reversed, executive function did not add additional unique variance after accounting for processing speed. Processing speed’s mediation of measures of visuospatial working memory (81.8% of MCI-LB-associated variance explained) and delayed verbal memory (53.9% of MCI-LB-associated variance explained) was stronger in MCI-LB than in MCI-AD (60.0% and 29.0% of MCI-AD-associated variance explained, respectively).
Table 2. Results of hierarchical regression analyses examining the effects of Mild Cognitive Impairment (MCI) with Lewy bodies (LB; n = 44) and Alzheimer’s disease (AD; n = 39) relative to healthy control subjects (n = 34), and the processing speed and executive function measures on neuropsychological domain performance

% Group-associated variance explained is calculated as the percent decrease of variance explained by MCI status [after estimated premorbid IQ (NART IQ) and age] when processing speed or executive function is accounted for in the previous step when predicting performance in a neuropsychological domain. For example, cell 1 shows that 21.0% of variance in Verbal Learning and Memory is explained by group (MCI-LB or control). In cell 2, group has been entered after processing speed, resulting in group explaining only ΔR 2 = .07. Therefore, cell 2 also shows that processing speed has accounted for 66.7% group-associated variance in Verbal Learning and Memory (.21–.07/.21). In cell 4, we show 8.0% of additional variance in Verbal Learning and Memory is explained by processing speed if executive function is accounted for previously. See supplementary materials for full model.
Processing speed and motor function
After age and NART, UPDRS scores accounted for 18% of DSST score variance in MCI-AD (F[1,34] = 7.87, p = .008), but did not predict DSST scores in controls (ΔR 2 = .00, F[1,28] = .01, p = .922), nor MCI-LB (ΔR 2 = .00, F[1,36] = .01, p = .920). Error Check, which isolates visual scanning efficiency, explained the largest amount of DSST score variance in all three groups (controls: 75%, F(1,29) = 47.50, p < .001; MCI-LB: 77%, F(1,38) = 106.25, p < .001; MCI-AD: 76%, F(1,33) = 119.74, p < .001), and explained an additional 3% of unique variance after accounting for graphomotor speed (Symbol Copy) in controls, 15% in MCI-LB (p < .001), and 20% in MCI-AD (p < .001). Graphomotor speed explained less variance in controls (11%, F[1,29] = 6.21, p = .019) than MCI subtypes (MCI-LB: 49%, F[1,38] = 56.68, p < .001; MCI-AD: 40%, F[1,33] = 34.34, p < .001). However, after accounting for visual scanning, graphomotor speed no longer significantly predicted DSST in controls (ΔR 2 = .03, F[1,28] = 4.07, p = .053) and explained only small additional variance in MCI-LB (ΔR 2 = .04, F[1,37] = 8.77, p = .005) and MCI-AD (ΔR 2 = .03, F[1,32] = 4.43, p = .043).
Discussion
The present study aimed to characterize the neuropsychological profile of MCI-LB compared to MCI-AD and healthy older people, and to identify if impairments in MCI are related to deficits in domain-general cognitive resources, such as executive dysfunction or slowed processing speed. Both MCI subtypes scored significantly lower than healthy controls on all neuropsychological measures except immediate memory and simple reaction time. However, divergence between MCI groups was also evident, despite having a similar level of global cognitive impairment (MMSE and CDR). The MCI-LB group was impaired relative to the MCI-AD group on measures of cognitive processing speed and executive function, in line with previous work (Ciafone et al., Reference Ciafone, Little, Thomas and Gallagher2020), but generally had similar levels of visuospatial dysfunction as MCI-AD, contrary to expectations (Cagnin et al., Reference Cagnin, Bussè, Gardini, Jelcic, Guzzo, Gnoato and Caffarra2015; Donaghy, Taylor, et al., Reference Donaghy, Taylor, O’Brien, Barnett, Olsen, Colloby and Thomas2018).
Examination of the hierarchical neuropsychological organization revealed a profile in MCI that was not evident in healthy older adults. Working memory impairment and multidomain amnesia in MCI were substantially related to slowed speed of processing, as measured by the DSST, a well-established test sensitive to neurological dysfunction and validated in a variety of populations (Van der Elst et al., Reference Van der Elst, van Boxtel, van Breukelen and Jolles2006). Processing speed, a distinct yet interrelated concept with executive function, is the domain-general speed of execution of basic cognitive functions. This process thereby limits completion of time-sensitive actions (e.g., memory formation, which necessitates information processing before working memory decay; Luszcz & Bryan, Reference Luszcz and Bryan1999; Nebes et al., Reference Nebes, Butters, Mulsant, Pollock, Zmuda, Houck and Reynolds2000). Processing speed was also a better explanatory factor than the executive function composite (verbal fluency and Trails Ratio) in both subtypes. In MCI-LB, executive function did explain a significant proportion of verbal learning and memory and delayed memory impairment, but this relationship was completely accounted for by differences in processing speed. This mediating role of speed of processing could be argued to be due to the motor impairments associated with MCI-LB. However, subanalyses of the DSST indicated that this measure was not related to motor impairment (UPDRS) in MCI-LB and was more strongly related to the cognitive aspect of the task (visual scanning) than to slowed graphomotor speed, in line with previous reports in Lewy body dementia (Firbank, O’Brien, & Taylor, Reference Firbank, O’Brien and Taylor2018) and PD (Johnson et al., Reference Johnson, Almeida, Stough, Thompson, Singarayer and Jog2004). LB disease is associated with substantial deficits in the cholinergic system (Ballard et al., Reference Ballard, O’Brien, Gray, Cormack, Ayre, Rowan and Walker2001), key to the attentional abilities involved in information processing. Presynaptic dysfunction driven by alpha-synuclein aggregates is present even at early stages of LB disease (Kramer & Schulz-Schaeffer, Reference Kramer and Schulz-Schaeffer2007; Schulz-Schaeffer, Reference Schulz-Schaeffer2010), and our results similarly demonstrate processing speed slowing in the MCI phase. Both MCI subtypes showed a hierarchical structure of performance predicted by their speed of processing, although the magnitude of the effect was notably smaller in MCI-AD than in MCI-LB in the case of visuospatial working memory and delayed verbal memory. Taken together, while MCI-LB had significantly slower processing speed than MCI-AD, it may nevertheless be a feature common to neurodegenerative diseases.
Given the lack of evidence of poorer visuospatial function in MCI-LB relative to MCI-AD in the present study, future work should investigate the trajectory of visuospatial decline in MCI. In a longitudinal analysis of a previous cohort, we found that visuospatial function declined more rapidly in MCI-LB (Hamilton et al., Reference Hamilton, Matthews, Donaghy, Taylor, O’Brien, Barnett and McKeith2021). This finding was also reported by another group in DLB compared with AD (Smirnov et al., Reference Smirnov, Galasko, Edland, Filoteo, Hansen and Salmon2020), although not by van de Beek et al. (Reference van de Beek, van Steenoven, van der Zande, Barkhof, Teunissen, van der Flier and Lemstra2020) in MCI-LB versus MCI-AD. Complex visual hallucinations also predict more rapid decline in MCI-LB (Hamilton et al., Reference Hamilton, Matthews, Donaghy, Taylor, O’Brien, Barnett and Thomas2020). Visuospatial function is suggested to have greater dependency on the executive system than verbal function, indicating a lack of symmetry in multicomponential models of working memory (Thompson et al., Reference Thompson, Hamilton, Gray, Quinn, Mackin, Young and Ferrier2006). While exploratory, it is possible that pronounced visuospatial dysfunction may only become apparent in DLB as a secondary effect as executive dysfunction worsens over the disease course. Executive function is a multifaceted construct, empirically delineated to include processes like set-shifting, updating, and inhibition (Miyake et al., Reference Miyake, Friedman, Emerson, Witzki, Howerter and Wager2000). The executive function measures employed in the present study (Trails and phonemic verbal fluency) are primarily dependant on set-shifting (Snyder, Miyake, & Hankin, Reference Snyder, Miyake and Hankin2015), noted as impaired in MCI-LB (Cagnin et al., Reference Cagnin, Bussè, Gardini, Jelcic, Guzzo, Gnoato and Caffarra2015; Jicha et al., Reference Jicha, Schmitt, Abner, Nelson, Cooper, Smith and Markesbery2010). While executive functions share a common mechanism (Snyder, Reference Snyder2013), more extensive testing could capture the construct more fully. Furthermore, a limitation of the present study is the omission of additional basic visuospatial working memory measures, such as line orientation tests, that may be less dependent on executive abilities.
Delayed recall conditions, whether for verbal or visuospatial (MTCF) stimuli, revealed amnestic impairment in MCI-AD, suggesting a profile similar to advanced AD. For example, 59% of MCI-AD patients scored at or below the 5th percentile of controls on tests of delayed verbal memory. However, more than a quarter of MCI-LB patients also demonstrated delayed verbal memory deficits below the 5th percentile of controls. Moreover, the stepwise discriminant analysis resulted in a model omitting verbal memory as predictive of group membership. Previous work by Ferman et al. (Reference Ferman, Smith, Kantarci, Boeve, Pankratz, Dickson and Petersen2013) showed that, although single-domain amnestic MCI rarely progresses to DLB, memory impairment is common in prodromal DLB patients with attention and/or visuospatial dysfunction (24.5%). Therefore, despite significantly poorer performance in MCI-AD at a group level, memory impairments can present in clinically-defined MCI-LB patients (Ferman et al., Reference Ferman, Smith, Kantarci, Boeve, Pankratz, Dickson and Petersen2013; Kemp et al., Reference Kemp, Philippi, Phillipps, Demuynck, Albasser, Martin-Hunyadi and Blanc2017). The extent to which an amnestic presentation in LB disease is attributable to co-occurring AD neuropathology remains debated (Ferman et al., Reference Ferman, Smith, Kantarci, Boeve, Pankratz, Dickson and Petersen2013) but it is a frequent presentation, with a recent analysis of 670 brains finding over 11% of people with dementia had both high grade AD and DLB (McAleese et al., Reference McAleese, Colloby, Thomas, Al-Sarraj, Ansorge, Neal and Attems2021). However, recent work failed to find differences in neuropsychological or neuropsychiatric profile and cognitive fluctuations between amyloid-positive and amyloid-negative DLB cases using PET imaging (Donaghy, Firbank, et al., Reference Donaghy, Firbank, Thomas, Lloyd, Petrides, Barnett and O’Brien2018). The phenomenon of multiple pathologies and the possible interactions of concurrent AD and DLB pathology in many people with dementia challenge attempts to delineate clear, aetiologically-specific neuropsychological profiles, with less than a quarter of cases in the above analysis having pure pathology (McAleese et al., Reference McAleese, Colloby, Thomas, Al-Sarraj, Ansorge, Neal and Attems2021). However, the present study benefited from the utilization of two biomarkers of LB disease and annually-repeated neuropsychological and clinical assessments. While it is a limitation of our study that we were not able to incorporate AD biomarkers such as amyloid imaging and cerebrospinal fluid, the fact we rigorously excluded vascular, Lewy body, and frontotemporal aetiologies means our MCI-AD group would predominantly have been people with AD. In general, the discriminant utility of neuropsychological assessment used in isolation has been shown to be limited in MCI (Donaghy et al., Reference Donaghy, Ciafone, Durcan, Hamilton, Barker, Lloyd and Taylor2020), emphasizing the importance of continued validation of the proposed MCI-LB biomarkers.
In summary, the present study suggests that MCI-LB and MCI-AD display cognitive impairments in line with the advanced stages of DLB and AD, respectively, although there was considerable overlap in their general neuropsychological profile. MCI-LB was characterized by executive dysfunction and slowed speed of processing, while MCI-AD displayed an amnestic profile. The assessment of the findings within their hierarchical framework indicated that deficits in higher-order cognitive activities in both MCI subtypes were mediated by processing speed, a profile which was strongest in MCI-LB and entirely absent in healthy controls.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1355617721001181
Financial Support
This study was supported by a major project research grant from Alzheimer’s Research UK (ARUK-PG2015-13); a doctoral studentship from the Medical Research Council (J.C.); ligand for the FP-CIT scans provided by GE Healthcare; an Alzheimer’s Society healthcare professional Fellowship (G.R.); infrastructure and support for authors based at Newcastle by the National Institute for Health Research (NIHR) Newcastle Biomedical Research Centre, a partnership between Newcastle upon Tyne Hospitals NHS Foundation Trust and Newcastle University; and the NIHR Cambridge Biomedical Research Centre (J.O.B).
Conflicts of Interest
AT has received support from GE Healthcare for investigator led research including the provision of FP-CIT in this study. Outside of this work JPT has acted as a consultant for Kyowa Kirin, Heptares Sosei, and received grant funding from Heptares Sosei and speaker fees from GE Healthcare. GR and GP have received honoraria from GE Healthcare for delivering educational workshops on FP-CIT imaging. Outside of this work JOB has acted as a consultant for TauRx, Axon, Eisai, Roche, and GE Healthcare and received grant funding from Alliance Medical and Merck. RD has received an educational travel grant from Britannia outside of this work. JC, PCD, CAH, SL, SC, MF, LA report no financial relationships with commercial interests.