Introduction
Antrochoanal polyp is a benign lesion that arises from the maxillary sinus mucosa, extends through the main or accessory ostium towards the middle meatus, and protrudes posteriorly to the nasopharynx.Reference Maldonado, Martínez, Alobid and Mullol1 It is usually unilateral, although rare cases of bilateral lesions have been reported.Reference Iziki, Rouadi, Abada, Roubal and Mahtar2 Antrochoanal polyp represents about 4–6 per cent of all nasal polyps in the general population, and it is more common among children and young adults.Reference Yaman, Yilmaz, Karali, Guclu and Ozturk3 The most common presenting symptom is nasal obstruction. Other less frequent complaints are rhinorrhoea, epistaxis and snoring.Reference Sarafraz, Niazi and Araghi4 The ‘gold standard’ methods for antrochoanal polyp diagnosis are nasal endoscopy (Figure 1) and computed tomography (CT) (Figure 2).

Figure 1. Endoscopic view of the left nasal cavity. The white arrow points to the remnant of the antrochoanal polyp seen through a widened accessory ostium of the maxillary sinus. MT = middle turbinate
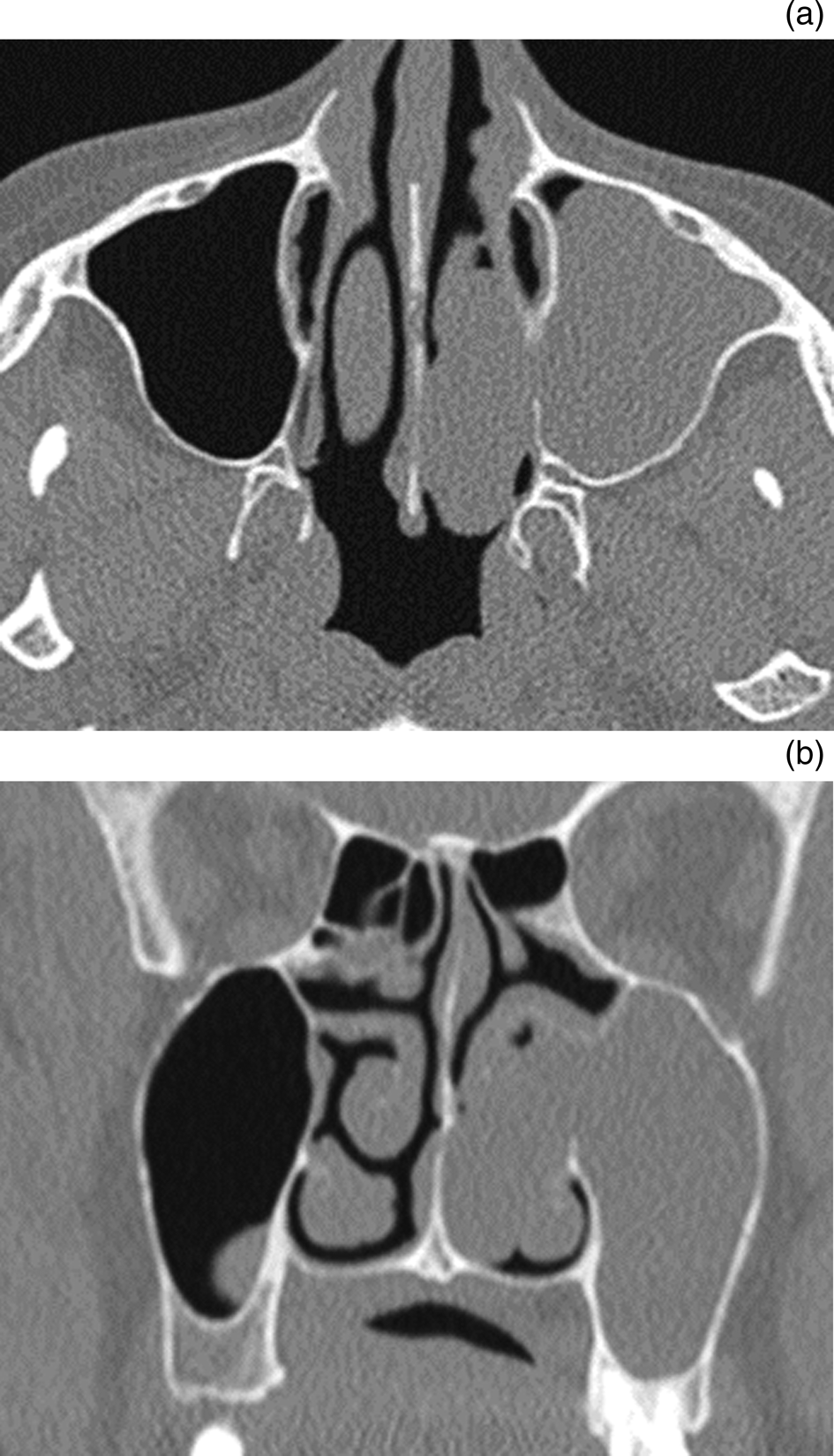
Figure 2. Computed tomography of paranasal sinuses showing soft tissue opacity filling the maxillary sinus and nasal cavity in (a) axial plane and (b) coronal plane.
The pathogenesis of antrochoanal polyp is not fully understood. Chronic processes of the nasal cavity (e.g. chronic sinusitis and allergic rhinitis) are among the main aetiologies implicated in the development of antrochoanal polyp.Reference Chen, Schloss and Azouz5–Reference Frosini, Picarella and De Campora7 Other theories include lymphatic obstruction, dental trauma and microvascular disease.Reference Mostafa, Fawzy, Jabri and Ayad8 The role of anatomical pathologies, including septal deviation, concha bullosa and turbinate hypertrophy, is controversial. Based on the Bernoulli phenomenon, it was hypothesised that a narrowing of the nasal passage as a result of these alterations creates a negative pressure that encourages herniation of the polyp through the maxillary sinus into the nasal cavity.Reference Frosini, Picarella and De Campora7
Our study aimed to examine the association between deviated nasal septum and antrochoanal polyp, and to promote decision-making when these two pathologies co-exist.
Materials and methods
This study was a collaboration between two tertiary medical centres. We retrospectively reviewed electronic medical records of patients diagnosed with antrochoanal polyp and referred to surgery at either one of our medical centres between 2009 and 2019. Patients who had undergone septoplasty in the past or did not have a CT scan prior to surgery were excluded. The data collected included demographic details, presenting symptoms, disease side and surgical parameters.
Senior rhinologists from each centre reviewed the CT scans of patients and determined the presence of septal deviation and its laterality in relation to that of the antrochoanal polyp. In order to explore the effect of the deviation shape, we used the classification proposed by MladinaReference Mladina9 (Table 1) and assigned each septal deviation its type based on the CT scan.
Table 1. Mladina classification for nasal septal deviation

Statistical analyses were performed using SPSS® (version 26) statistical software. A chi-square test was conducted to evaluate the association between septal deviation and polyp laterality and to examine the effect of the type of deviation.
Results and analysis
Eighty-seven patients were operated on for antrochoanal polyp in the participating medical centres during the study period. Thirty-nine patients were excluded (35 patients who did not have a CT scan prior to surgery and 4 who had undergone septoplasty in the past). Thus, 48 patients were included in the final analysis. Their demographic details and clinical features are presented in Table 2.
Antrochoanal polyps were found equally on both sides of the nasal cavity. Deviation of the septum was present in 37 patients (77.1 per cent); its laterality is detailed in Table 2. In order to gain access and remove the antrochoanal polyp completely, simultaneous septoplasty was performed in 11 (22.9 per cent) patients.
Antrochoanal polyp was found ipsilaterally to the side of the deviated septum in 21 of 48 patients (43.75 per cent), as presented in Figure 3. No statistically significant correlation was found between the side of the antrochoanal polyp and the laterality of the deviated septum (p = 0.664).

Figure 3. Bar chart presenting the laterality of the antrochoanal polyp in relation to the side of the deviated nasal septum. ACP = antrochoanal polyp
Table 3 depicts the frequency of the different types of deviation according to the Mladina classification in our cohort. No statistically significant association was found between the type of deviation and the laterality of the antrochoanal polyp and deviated septum (p = 0.159).
Table 3. Types of nasal septal deviation according to Mladina classification*

* n = 37. ACP = antrochoanal polyp
Discussion
Although the first description of antrochoanal polyp dates back to 1906, its pathogenesis has not been clarified to this day, and several theories have emerged. Berg et al.Reference Berg, Carenfelt, Silfverswärd and Sobin10 found macro- and microscopic similarities between the antral part of antrochoanal polyps and the intramural cyst of the maxillary sinus. Thus, they hypothesised that antrochoanal polyp develops from an expanding intramural cyst. Chronic inflammation, infectious or allergic, has also been suggested as an aetiological factor. Chen et al.Reference Chen, Schloss and Azouz5 argued that mucous gland obstruction caused by inflammation leads to the development of the cystic part of antrochoanal polyp. In contrast, Piquet et al.Reference Piquet, Chevalier, Leger, Rouquette and Leconte-Houcke11 claimed it was secondary to stenosis of the lymph duct caused by chronic phlogosis. Lee and HuangReference Lee and Huang12 supported chronic sinusitis as an aetiological factor because over half of their patients had a history of chronic sinusitis.
• The antrochoanal polyp is almost always a unilateral lesion
• It represents about 5 per cent of all nasal polyps in the general population and is more common among children and young adults
• The role of nasal septum deviation in antrochoanal polyp pathogenesis is controversial
• The antrochoanal polyp side does not correlate with the laterality and Mladina type of nasal septum deviation
• Septal deviation repair is not mandatory as a part of a surgical procedure for the antrochoanal polyp unless the deviation prevents a complete excision of the lesion
What causes the cyst to herniate outside the maxillary sinus is also not fully understood. Frosini et al.Reference Frosini, Picarella and De Campora7 suggested that increased pressure inside the maxillary sinus resulting from simultaneous obstruction of the accessory and natural ostium is the cause. In their review of 200 cases, nasal disorders (e.g. septal deviation, inferior turbinate hypertrophy and concha bullosa) were present in 83 per cent of patients and, as a group, was the only factor associated with antrochoanal polyp. They suggested that these anatomical alterations could further increase the pressure gradient between the maxillary sinus and middle meatus and thus play a role in the pathogenesis of antrochoanal polyp. Consistent with this, Hekmatnia et al.Reference Hekmatnia, Shirvani, Mahmoodi and Hashemi13 also found an association between antrochoanal polyp and septal deviation. However, none of these studies referred to the laterality of the deviated septum. Although Balikci et al.Reference Balikci, Ozkul, Uvacin, Yasar, Karakas and Gurdal14 found septal deviation in half of their patients, it was not different from the incidence in the general population.Reference Mladina, Cujić, Subarić and Vuković15
In our study, there was no correlation between the laterality of the septal deviation and the side of antrochoanal polyp growth. We believe this is because not all septal deviations were significant enough to cause a narrowing of the nasal passage that was sufficiently substantial to change the pressure within the nasal cavity. The different findings of our study can be explained, firstly by the fact that the presence of septal deviation is based, at least to some degree, on the physician's subjective opinion (particularly in cases of mild deviation). Secondly, there are different methods for evaluating the septum (e.g. anterior rhinoscopy, endoscopy, imaging) without uniformity between the studies.
Our study has two main limitations. Because of its retrospective nature, clinical data on the history of chronic sinusitis were missing for a portion of the participants and therefore could not be analysed. Furthermore, we could not measure the airflow within the nasal cavity and thus objectively assess the influence of the deviated septum.
Conclusion
Septal deviation was not found to be associated with antrochoanal polyp. Therefore, routine repair of such deviation as part of a surgical procedure for antrochoanal polyp is not mandatory unless it prevents a complete excision of the lesion.
Competing interests
None declared









