Impact statement
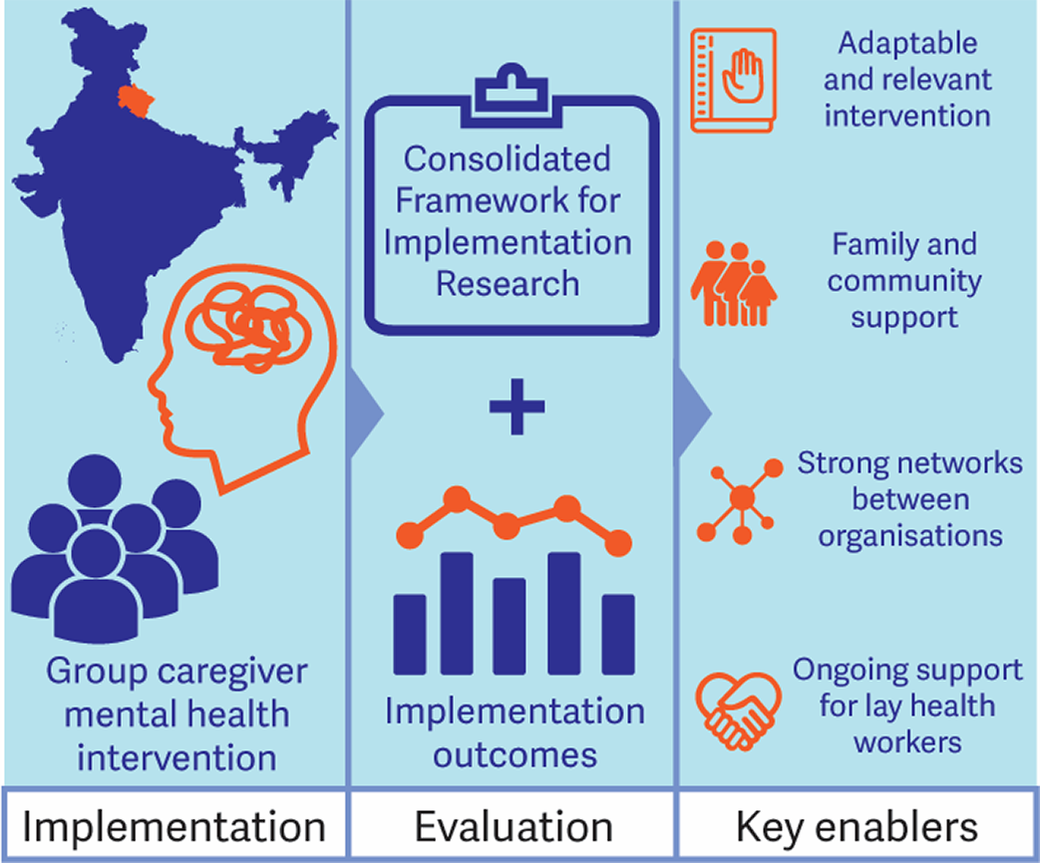
Nearly every disabled person in South Asia (such as people with difficulties walking or with mental health problems) is supported by family caregivers for their activities of daily living. Caregivers are central in the disability ecosystem in settings like India, where there is limited public and social support for disabled people. Yet caregiving is heavy and unceasing work and most caregivers receive little support meaning that they are at higher risk of experiencing mental distress. Few studies describe what works to strengthen the mental health and well-being of caregivers, and even fewer describe how an intervention can work well when rolled out among other organisations. This is essential to know in order to deliver interventions to larger numbers of people. This study tries to address this gap. In 2021, we had evaluated this caregiver mental health intervention (Nae Umeed or New Hope) and found it was effective. In this project, we aimed to describe the process of rolling out Nae Umeed with seven other organisations to learn what works well and what does not. We found Nae Umeed was a relevant and adaptable intervention that participants were positive about. Participation went better when participants also experienced family support to join in group sessions and try out the new ideas at home. We identified factors that made it work well from the perspective of organisations such as finding that the community health workers who facilitated groups needed to connect relationally with the community and to be supported with resources and training. Nae Umeed did not go as well if participants were too overloaded with other responsibilities, or if they experienced stigma. The group format allowed people to form new friendships which also provided social support after the programme finished. Nae Umeed merits consideration and rollout in other settings in South Asia.
Introduction
Approximately one in six adults is caregivers (Tur-Sinai et al., Reference Tur-Sinai, Teti, Rommel, Hlebec and Lamura2020). Caregiving, defined as the provision of care to another person with a long-term care need outside of any formal framework (Tur-Sinai et al., Reference Tur-Sinai, Teti, Rommel, Hlebec and Lamura2020), is crucial to the sustainability of health and social care systems, but also can be associated with negative mental health consequences for the caregiver (Pinquart and Sörensen, Reference Pinquart and Sörensen2003; Talley and Crews, Reference Talley and Crews2007). Caregivers in low- and middle-income countries (LMICs) have an estimated 50% higher odds of depression than non-caregivers, even after controlling for socioeconomic factors that may in part mediate mental health effects (Magaña et al., Reference Magaña, Martínez and Loyola2020).
In India, caregivers who are socioeconomically disadvantaged are additionally vulnerable to mental ill-health. Women report high caregiver “burden” and make up the largest proportion of caregivers (Kumar and Gupta, Reference Kumar and Gupta2014; Mandowara et al., Reference Mandowara, Patel, Amin, Phatak and Desai2020; Madavanakadu et al., Reference Madavanakadu, Grills, Scaria, Benny and Joubert2021). Additionally, caregivers who are socially isolated (Jagannathan et al., Reference Jagannathan, Thirthalli, Hamza, Nagendra and Gangadhar2014; Mathias et al., Reference Mathias, Kermode, Sebastian, Davar and Goicolea2019; Bapat and Shankar, Reference Bapat and Shankar2021), under financial strain (Bapat and Shankar, Reference Bapat and Shankar2021; Madavanakadu et al., Reference Madavanakadu, Grills, Scaria, Benny and Joubert2021), or less educated (Jagannathan et al., Reference Jagannathan, Thirthalli, Hamza, Nagendra and Gangadhar2014; Mandowara et al., Reference Mandowara, Patel, Amin, Phatak and Desai2020; Bapat and Shankar, Reference Bapat and Shankar2021; Menon et al., Reference Menon, Patil, Ramaswamy, Gattani, Castelino, Dhekale, Gota, Sekar, Deodhar, Mahajan, Daptardar, Prabhash, Banavali, Badwe and Noronha2022) are more vulnerable to adverse mental health. A further challenge is that access to quality affordable primary health care in India is limited, especially rurally (Patel et al., Reference Patel, Parikh, Nandraj, Balasubramaniam, Narayan, Paul, Kumar, Chatterjee and Reddy2015). The importance of caregiver mental health in India is likely to rise as the population ages, the burden of non-communicable diseases increases, and there is limited responsiveness to emerging needs in the social welfare and health systems (Bollyky et al., Reference Bollyky, Templin, Cohen and Dieleman2017).
Relatively little progress has been made on strategies to support caregiver well-being and mental health in India. Globally, mostly in high- and middle-income settings, a variety of interventions to improve caregiver mental health have been developed (Sörensen et al., Reference Sörensen, Pinquart and Duberstein2002; Hinton et al., Reference Hinton, Kohrt and Kleinman2019), however, these may be of limited utility in lower resource settings. In India, a few interventions have been trialled in single health services or districts (Das et al., Reference Das, Saravanan, Karunakaran, Manoranjitham, Ezhilarasu and Jacob2006; Dias et al., Reference Dias, Dewey, D’Souza, Dhume, Motghare, Shaji, Menon, Prince and Patel2008; Kulhara et al., Reference Kulhara, Chakrabarti, Avasthi, Sharma and Sharma2009; Chakraborty et al., Reference Chakraborty, Bhatia, Anderson, Nimgaonkar and Deshpande2014; Chatterjee et al., Reference Chatterjee, Naik, John, Dabholkar, Balaji, Koschorke, Varghese, Thara, Weiss, Williams, McCrone, Patel and Thornicroft2014; Lamech et al., Reference Lamech, Lakshminarayanan, Vaitheswaran, John and Rangaswamy2020; Baruah et al., Reference Baruah, Varghese, Loganathan, Mehta, Gallagher-Thompson, Zandi, Dua and Pot2021; Singh et al., Reference Singh, Singh, Gupta and Singh2021; Sims et al., Reference Sims, Juliet, Joseph, Gopal, Raghavan, Venkatraman and Padmavati2022; Stoner et al., Reference Stoner, Lakshminarayanan, Mograbi, Vaitheswaran, Bertrand, Brum, Durgante, Ferri, Mkenda, Walker, Dotchin, Paddick, Chandra, Krishna, Du, Shaji, Fisher and Spector2022), but have not been implemented at scale. Scaling-up of interventions in LMICs has been identified as a gap in implementation research (Meffert et al., Reference Meffert, Neylan, Chambers and Verdeli2016; Alonge et al., Reference Alonge, Rodriguez, Brandes, Geng, Reveiz and Peters2019).
Nae Umeed (New Hope) is a community-based group intervention aiming to improve caregiver mental health by building knowledge and skills in psycho-social health and social participation. The intervention was developed by Burans (2022), a partnership initiative focussed on improving mental health in communities in Uttarakhand, India. Nae Umeed was piloted in 2019 and 2020 in Dehradun, the capital of Uttarakhand (Bailie et al., Reference Bailie, Pillai, Singh, Leishman, Grills and Mathias2023). Following this, in 2022, Burans scaled up implementation with other organisations in the Uttarakhand Community Health Cluster (CHGN-UKC). This study aimed to evaluate this scale-up implementation, with sub-objectives of describing the implementation and its outcomes and exploring barriers and enablers to implementation.
Methods
Intervention
Nae Umeed consists of 14 modules designed to be delivered within community settings to groups of 8–12 participants by trusted local community health workers. The curriculum covers self-care, caregiving, psychosocial well-being, behaviour management, drugs, accessing support and entitlements, and managing household finances. The intervention design is described in greater detail elsewhere (Emmanuel Hospital Association, 2019, Bailie et al., Reference Bailie, Pillai, Singh, Leishman, Grills and Mathias2023). In a pre-post effectiveness study as part of the 2020 Dehradun implementation, participants showed significant improvement in self-rated depression, well-being, and social participation (Bailie et al., Reference Bailie, Pillai, Singh, Leishman, Grills and Mathias2023), consistent with previous findings for the effectiveness of psychosocial group interventions (Sörensen et al., Reference Sörensen, Pinquart and Duberstein2002).
Implementation context and strategy
Implementation was conducted in Uttarakhand, North India, a state with a population of about 10 million people, of whom 70% live rurally, 20% are scheduled caste or tribe and 80% are literate. There is very limited access to outpatient care or counselling for people with mental health problems (Mathias et al., Reference Mathias, Goicolea, Kermode, Singh, Shidhaye and Sebastian2015). Women are typically responsible for most domestic and household tasks.
Burans implemented Nae Umeed in conjunction with CHGN-UKC, a partnership of community health and development non-governmental organisations (NGOs) that collaborate on training, resource development, advocacy, and research partnerships (Grills et al., Reference Grills, Varghese, Hughes, Jolly and Kumar2016; Uttarakhand Community Health Cluster, 2022). The implementation strategy aimed to engage and support CHGN-UKC partners to deliver Nae Umeed within their existing work areas. CHGN-UKC partners were invited to participate in the implementation of Nae Umeed and seven partners participated.
Burans provided centralised technical assistance and training on the intervention and partners allocated community health workers (facilitators) to deliver the intervention. Facilitators were responsible for forming groups in their local catchments through existing community networks, conducting meetings, and recording attendance. Burans project staff supervised training, conducted support visits, and assisted with field issues. The training involved several one-day workshops spaced over the intervention. Facilitators were able to access support via a Whatsapp group. Burans paid an allowance to facilitators to cover travel costs.
Facilitators formed 16 groups with 158 participants across the districts of Dehradun (10 groups), Tehri (4 groups), and Uttarkashi (2 groups). Modules were delivered from April to September 2022. Groups in Tehri and Uttarkashi were formed in rural mountainous regions, where the main source of income is agriculture, and where there is limited access to quality education and healthcare. Groups in Dehradun were formed in both rural and semi-urban areas. The main source of income in these areas is daily wage labour and access to education and health care facilities is easier.
Positionality
D.A., S.R. and L.B. are Indian nationals who speak Hindi as their first language and are employed by Burans, Herbertpur Christian Hospital (HCH). K.M. was employed by Burans, HCH for 11 years and speaks Hindi. K.M. and N.J.G. have both worked in Uttarakhand for more than a decade and are currently based in universities in Australasia. C.R.B. is an Australian national who worked as a public health medicine trainee with Burans for a six month period.
Study design
Our observational mixed-methods evaluation consisted of (1) Qualitative exploration of implementation determinants using the updated Consolidated Framework for Implementation Research (CFIR) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022), and; (2) Quantitative assessment of implementation outcomes (reach, dose delivered) using administrative and survey data.
The CFIR is an implementation determinants framework consisting of 48 constructs across five domains covering the Intervention (Nae Umeed), and implementation context including Outer Setting, Inner Setting, Individuals, and Implementation Process (Damschroder et al., Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009, Reference Damschroder, Reardon, Widerquist and Lowery2022; Figure 1). In operationalising the CFIR, we considered the Inner Setting domain to consist of Burans and implementing partners, and the Outer Setting domain to consist of the contexts within which they operate. Based on an initial scoping discussion with implementers we developed semi-structured in-depth interview (IDI) and focus group discussion (FGD) guides using the CFIR interview guide tool (CFIR Research Team, 2022) and a framework for the design and delivery of group interventions (Hoddinott et al., Reference Hoddinott, Allan, Avenell and Britten2010) to include specific questions addressing the constructs: Intervention design, Local conditions/attitudes, Available resources, Access to knowledge and information, Assessing needs and context, and Engaging. We included open-ended questions to capture data on other constructs.
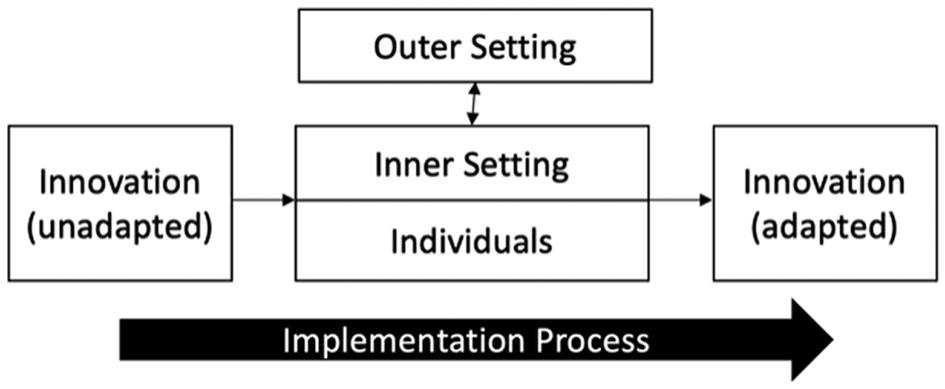
Figure 1. Schematic diagram of the Consolidated Framework for Implementation Research (CFIR). Adapted from Damschroder et al. (Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009, Reference Damschroder, Reardon, Widerquist and Lowery2022).
We defined reach (Glasgow et al., Reference Glasgow, Harden, Gaglio, Rabin, Smith, Porter, Ory and Estabrooks2019) according to representation among participants of the disadvantaged demographic groups which are the primary targets of Nae Umeed. We operationalised the dose delivered (Rowbotham et al., Reference Rowbotham, Conte and Hawe2019) per session, as the number of participants attending divided by the number of participants recruited at baseline. In reporting this study we adhered to the Standards for Reporting Implementation Studies (StaRI) Statement (Pinnock et al., Reference Pinnock, Barwick, Carpenter, Eldridge, Grandes, Griffiths, Rycroft-Malone, Meissner, Murray, Patel, Sheikh and Taylor2017).
Data collection
Qualitative
D.A. and C.R.B. conducted IDIs (25 total) and FGDs (six total) with implementers (six IDIs), group facilitators (five IDIs, one FGD), and participants (14 IDIs, 5 FGDs) who were selected to reflect a range of stakeholder roles and intersectional identities. IDIs and FGDs lasted approximately 1 hour and were conducted in October and November 2022. We conducted FGDs and IDIs in person in Hindi, except for four IDIs with implementers which we conducted in English via videoconference. All IDIs and FGDs were audio recorded, transcribed, and translated into English where applicable. Transcripts were checked for accuracy by the interviewer.
Quantitative
With participant consent, facilitators recorded anonymised demographic data from participants attending final meetings, using a standardised data collection instrument. We requested routine group attendance records from facilitators.
Data analysis
Qualitative
D.A. and C.R.B. assigned codes defined by the CFIR constructs and subconstructs, using Open Code 4.03 (ICT Services and System Development and Department of Epidemiology and Global Health, 2015). First, we each coded the same three transcripts, then met to review and resolve discrepancies. We coded the remainder of transcripts independently, with D.A., C.R.B., and K.M. meeting regularly to discuss coding decisions. We grouped coded data into categories defined by the CFIR domains. We interpreted data within each category by inductively developing themes relating to one or more implementation determinants.
Quantitative
D.A. and C.R.B. analysed quantitative data such as attendance simply and descriptively.
Ethics statement
Approval for this project was provided by the institutional ethics committee of the Emmanuel Hospital Association (protocol number: 240). Participants provided verbal and written consent to participate in data collection.
Results
Implementation determinants
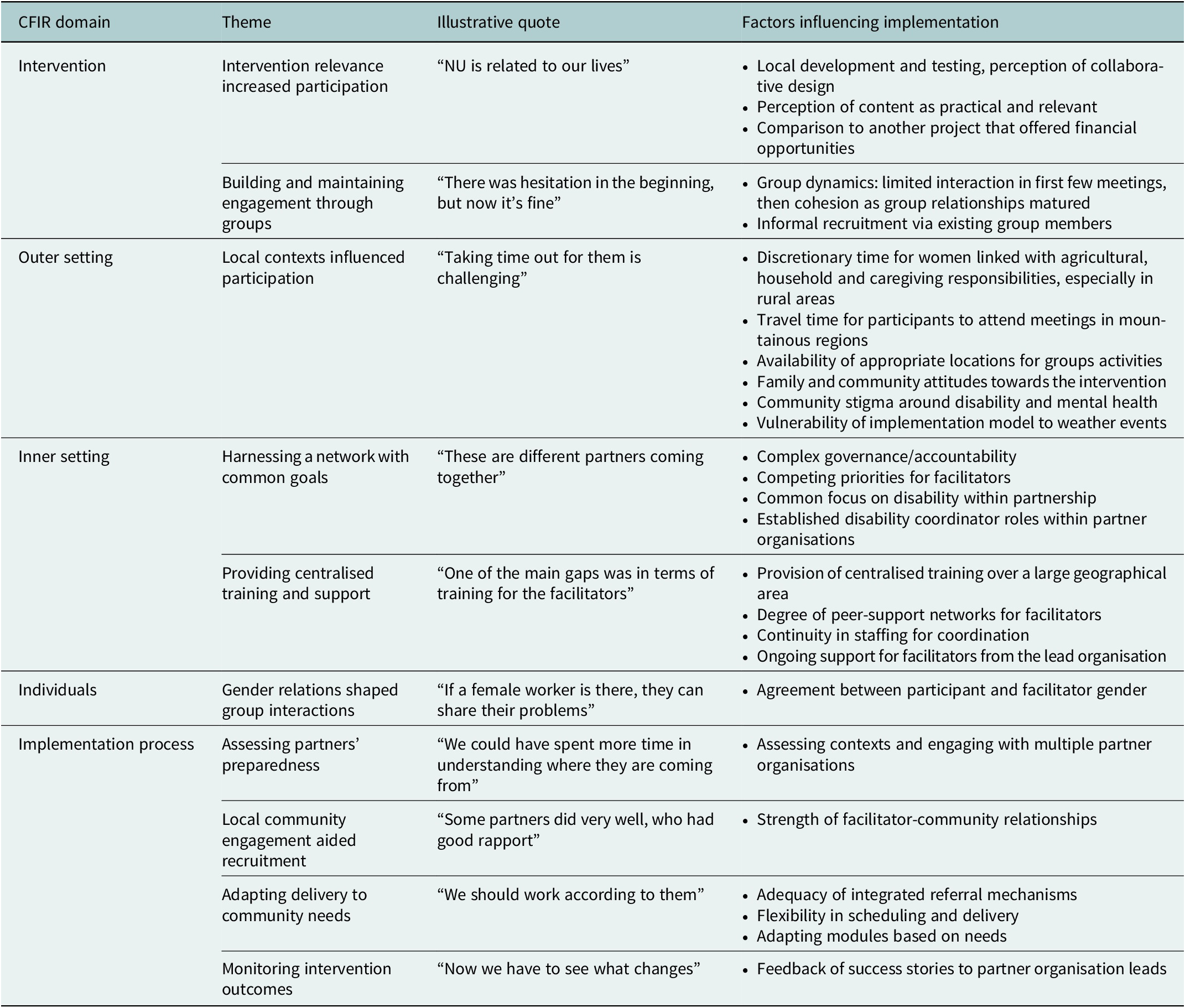
Results of the qualitative analysis are presented under the domains of the CFIR framework. Within each domain, key themes are presented using a heading followed by a verbatim quote-linked running header. Table 1 summarises key themes and the identified implementation determinants within each domain.
Table 1. Summary of themes and implementation determinants identified through interviews and focus groups
Intervention
Intervention relevance increased participation – “[Nae Umeed] is related to our lives”.
Participants expressed favourable views on the Intervention Design (content and presentation of the intervention) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) and found Nae Umeed content relevant and accessible which increased their enthusiasm for participation. One facilitator summarised this:
[Nae Umeed] is related to our lives, women’s lives. (It included) the things that we have to do every day like managing a budget and taking care of everyone’s medications (Facilitator).
Participants described the most useful modules as those on self-care, medication, and financial inclusion. One woman described how she became more attentive with medication:
After learning from here that we need to take medicines on time, I take my medicines on time and also give them to my child as well on time. Earlier, I was very careless with taking the medicines. Now, I am very meticulous (Participant).
Less favourable views of the intervention were expressed by some participants and facilitators in the context of Intervention Relative Advantage (comparison to other interventions in current use) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022). Many participants’ families were involved in a Disability Inclusive Livelihoods Initiatives Project (DILIP), which offered economic opportunities for the families of people with disability by providing training in income-generating skills (e.g. agriculture) and small start-up donations (e.g. goats). Despite Nae Umeed and DILIP having distinct objectives, some facilitators suggested that DILIP shaped expectations of Nae Umeed, acting as a disincentive to participation. However, these suggestions in some instances more broadly reflected a general desire for more economic opportunities. One facilitator suggested:
Since some members [of Nae Umeed] were already a part of DILIP, they were expecting some monetary help or donation. This impacted their will to join the groups (Facilitator).
Building and maintaining engagement through groups – “There was hesitation in the beginning, but now it’s fine”.
Participants described how groups provided safe environments for shared learning and cohesion. Group participants described sharing their problems and receiving support or advice from others who were going through similar challenges to themselves:
People come here and share about their life. We listen to each other and give suggestions about what can be done. It feels good to listen to solutions. Everyone offers different suggestions (Participant).
In some cases, facilitators described poor engagement initially, which slowly improved as participants developed closer relationships and became more comfortable with the group:
When the group started, people did not know each other so it was difficult, and they could not share much in the beginning. But towards the end, they built good relations with the participants, they could share what they felt with the group and that was helpful in bringing out new ideas (Facilitator).
Some participants subsequently brought friends or relations into the groups, resulting in informal “snowball” recruitment.
Outer setting
Local contexts influenced participation – “Taking time out for them is challenging”.
Participation was shaped by Local Attitudes and Local Conditions (beliefs, values, and socioeconomic/environmental conditions affecting implementation or delivery) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022). In rural areas, scheduling meetings was challenging due to prevailing gender relations which limit discretionary time for women with competing agricultural, household and caregiving responsibilities:
[…] the women are doing all the household things, looking after the children and husband’s health and everything. Taking time out for them is challenging (Implementer).
Travel-associated time and financial burden were additional barriers for participants in the more remote mountain areas, where groups consisted of people from multiple villages.
We have to walk 4–5 kilometres to come for the groups. Sometimes it becomes difficult as we have work in the fields. We cannot afford to take a jeep [public conveyance] (Participant).
Other practical constraints included finding a private space to meet:
It was very difficult for us, as there is not that much space in anyone’s house […] And when we used to do it in the outside area, people used to gather and ask questions (Participant).
Participants and facilitators described community conceptions of disability causation as either karmic or a “curse”. Episodes of verbal harassment of people with disability were cited as evidence of community stigma. These attitudes resulted in some families being reluctant to engage in Nae Umeed.
Earlier we were very apprehensive about sharing our daughter’s condition with others and that is why I did not join the group. But now after listening to other women in the group I feel I am not alone. I feel confident and supported (Participant).
Implementers noted vulnerability of the implementation, monitoring and reporting to environmental Critical Incidents (disrupting large-scale events) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) in the form of a heavy monsoon season.
During the rainy season, due to bad weather conditions and landslides, it became difficult to make frequent visits to different villages for reporting and monitoring (Implementer).
Inner setting
Harnessing a network with common goals – “These are different partners coming together”.
Implementation was facilitated by Mission Alignment (alignment of implementation and delivery with overarching organisational goals) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) with CHGN-UKC’s focus on supporting people with disability. There were well-established Relational Connections (networks within and across Inner Setting boundaries) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) in the form of groups within the cluster working on disability and mental health. An implementer described how organisational structures, such as having a disability coordinator within each partner, provided a workforce that already networked with families of people with disability:
We already have disability coordinators in each project […] and they are normally involved in the disability program – so combining disability and mental health; that was a good idea (Implementer).
Quality Communications (information sharing practices) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) within the cluster were used to spread awareness of the intervention and promote buy-in from partners. An implementer described how a regular cluster-wide meeting, “Linking to Learn” (L2L) allowed sharing of the intervention with a larger audience:
[…] the main purpose [of L2L] is that many organisations work in a remote area and organising, training, and updating is difficult for them. So CHGN can organise teaching and awareness training on health issues (Implementer).
The partnership model also provided challenges. Implementers described varying Relative Priority (importance of implementation compared to other initiatives) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) among partner organisations. Given the coordinating organisation did not provide direct funding to partners, Burans had little influence over commitments to delivery. Facilitators had to balance delivery of Nae Umeed with routine work of their home organisations:
As I am working with two different organisations, I have two different tasks to deal with, which are both important to me (Facilitator).
Structural Characteristics (infrastructure) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) within Burans, including staffing changes, initially limited support visits, impacting partner engagement. This was addressed by engaging a designated coordinator and increasing the frequency of visits.
Initially we [at Burans] were not able to hand over the implementation responsibility to a single person since the team was undergoing changes. But once a person was appointed, it all went smoothly (Implementer).
Implementers and facilitators reflected on tension between these characteristics of the Inner Setting and a perceived need to continue to support caregivers after completion of the intervention to sustain long-term outcomes:
It is also a responsibility for Burans to ensure that people who have been connected through these groups remain connected. That is very important (Implementer).
To address this issue of sustainability, some suggested training group members to continue supporting caregivers after completion of the curriculum to maintain impacts of Nae Umeed (for example by forming self-help groups for micro-credit and savings):
It is important for us to ensure that the group members hold meetings to maintain social support (Facilitator).
Providing centralised training and support – “A more systematic approach to training the facilitators would have worked better”.
Access to Knowledge and Information (accessibility of guidance or training to implement and deliver the intervention) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) was recognised as critical to implementation. Implementers and facilitators described the training as covering the intervention content but noted potential areas for training improvement. These included more focus on group formation and facilitation skills, and communicating the goals and purpose of the intervention. Logistic issues emerged with the initial training plan as described by one implementer:
[…] the facilitators from the hills come from very long distances. So coming for a one-day training, it meant like three days of their work. Which was not easy for them, to also go back and do the work they have in their organisation (Implementer).
In response to feedback, the implementation model was adapted so that some training was provided during monitoring visits. Ongoing support visits were valued and implementers viewed their role as supporting collaborative problem-solving with facilitators, rather than as monitoring fidelity or adherence to the intervention:
[facilitators] should feel that they are supported by Burans. It should not seem to them that we are people who came from outside and just checked what was happening (Implementer).
Individuals
Gender relations shaped group interactions – “It would be helpful to have a female facilitator as well”.
Differences between the genders of facilitators (mostly male) and participants (mostly female), were described as limiting engagement between facilitators and participants on difficult topics or personal problems. While participants downplayed the importance of facilitator gender, implementers and facilitators offered varying viewpoints. Some described a reluctance of female participants to engage with male facilitators:
Because if I’m a male person, [participants in villages] will not share feelings or the problems they’re going through. If a female worker is there, they can share their problems and we can build good rapport with them (Implementer).
Others suggested that the ability of facilitators to build and maintain rapport, irrespective of gender, was more important in determining engagement.
Implementation process
Assessing partners’ preparedness – “We could have spent more time in understanding where they are coming from”.
Implementers emphasised the importance of Assessing Needs and Assessing Context (collecting information about group priorities and barriers to implementation and delivery) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) of the target population and partners to successful implementation. They described that further assessment with partners in more rural and remote districts might have led to modification of the implementation plan. Implementers suggested pre-implementation visits with partners and questionnaires for potential participants as possible strategies for Assessing Needs. For example, to accommodate travel difficulties, and varying facilitator backgrounds:
I think if we could have spent more time in also understanding where these partners are coming from, and to understand more about their working methods, how they work in their organisations, to understand more of their context […] what we shared in orientation applied very well to some of the organisations, but with some I think it became more difficult (Implementer).
Implementers also reflected on the importance of Engaging leaders of partner organisations (encouraging participation in implementation) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) to increase the visibility of work done by facilitators and ensuring that facilitators were valued within their organisations:
[…] if we plan more with leaders then we can work [more effectively] with disability coordinators from each organisation (Implementer).
Local community engagement aided recruitment – “Some partners did very well, especially those who had good rapport”.
Participant Engagement was fostered by strong relationships between facilitators and community. Although some facilitators reported recruitment difficulties, many were able to recruit from their existing formal support networks and sometimes turned away potential participants because of high demand.
Adapting (modifying the intervention or setting for optimal fit) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) was recognised as critical in maintaining participant engagement. As a result of barriers in the Outer Setting, including family and community attitudes and competing demands on time, participants often arrived late to meetings or sent another family member to attend. Facilitators described learning to incorporate flexibility in the delivery to maintain engagement.
We taught them things, but we learnt from them as well. We understood that we cannot force them to come to the meetings at a particular time, but we need to take into consideration their suggestions as well. […] We understood that we should work according to them, only then will they understand us. […] There might be many other things that the person might be facing at the family level (Facilitator).
Facilitators described common modifications including adding content on health and medicines, and tips for saving money. A shortage of services drove some of these modifications. One facilitator reported feeling ill-equipped to deal with requests for help:
We were not told this in the module that when people [ask questions about getting medication or a medical appointment] whom do we refer to and from whom we can expect help (Facilitator).
Facilitators often adapted the content from the manual using local language and dialects because some participants found the language complicated. They also made modifications such as the use of more interactive activities including games and visual aids.
Monitoring intervention outcomes – “Now we have to see what changes”.
Notes recorded by facilitators on individual participant outcomes as part of Reflecting and Evaluating (collecting information about the success of implementation or intervention) (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) were reported to be useful in motivating partners.
[The partners] all remain. And they have also seen, because whenever feedback from the women came, we all always gave feedback to the organisation head, and he/she was very pleased to see the changes (Implementer).
However, implementers emphasised the importance of planned monitoring following completion of the curriculum to assess sustained intervention and implementation impacts.
[…] after a few months when we’ll revisit then we’ll see […] we have to see what changes – we can see the changes in their attitude, or in their work, or in their connection with the person with disability (Implementer).
Implementation outcomes
Reach
Sociodemographic data collection instruments were returned for 75 participants from 11 groups (Table 2), representing half the number of participants initially recruited. Three-quarters were female, half had completed less than 5 years of education, and one in five were of scheduled caste or tribe. Three-quarters reported having a person with disability in the household, most commonly a child of the participant.
Table 2. Sociodemographic characteristics of a sample of 75 Nae Umeed participants

a Age was not recorded for some participants due to an issue with collection forms.
Dose delivered
Attendance was 75–80% of those who registered for the programme over the first nine modules, using data for a subset of 10 groups. Data were not available for the final five modules (Figure 2).

Figure 2. Overall attendance for the first nine Nae Umeed modules as a proportion of the number of participants recruited at baseline.
Discussion
Several factors that influenced implementation in this study align with those described in the implementation of other mental health programmes in LMICs (Esponda et al., Reference Esponda, Hartman, Qureshi, Sadler, Cohen and Kakuma2020; Greene et al., Reference Greene, Huang, Giusto, Lovero, Stockton, Shelton, Santos, Saúte and Wainberg2021; Le et al., Reference Le, Eschliman, Grivel, Tang, Cho, Yang, Tay, Li, Bass and Yang2022), including service user engagement, a relevant and adaptable intervention, family support, stigma, provider skills and connection with community, team relationships, common organisational goals, staffing, training, monitoring, and referral systems (Esponda et al., Reference Esponda, Hartman, Qureshi, Sadler, Cohen and Kakuma2020, Greene et al., Reference Greene, Huang, Giusto, Lovero, Stockton, Shelton, Santos, Saúte and Wainberg2021, Le et al., Reference Le, Eschliman, Grivel, Tang, Cho, Yang, Tay, Li, Bass and Yang2022). Factors that we found were important which are less widely described in the literature included the influences of a group delivery format, competing responsibilities for caregivers in rural areas, challenges and opportunities associated with partnership delivery, and the varying influences of gender norms and relations across multiple CFIR domains. While the implementation successfully reached members of target vulnerable groups, issues in achieving sustained participant engagement highlight the potential for achieving better implementation and mental health outcomes by harnessing enablers and addressing barriers.
Reduction in participation to approximately 80% of baseline recruitment by the fourth module suggests that engagement was central for implementation success. Barriers to participation affecting some participants but not others, including lengthy travel, less supportive family, or expectations that were not met by the intervention may have led to selective early attrition. Fairly stable attendance following this early period (noting that attendance data was not available for the final five modules) may have been facilitated by the formation of supportive relationships within groups (Hoddinott et al., Reference Hoddinott, Allan, Avenell and Britten2010), and adaptations to the implementation process to better support facilitators.
The group format of Nae Umeed may have facilitated improved mental health outcomes via multiple mechanisms. An increased sense of social connection and support was described by participants as resulting from the formation of new friendships. The group provided an opportunity to safely rehearse new skills (such as talk about emotions or speak of challenges), as well as a perception of collective strength from group membership. Our finding suggested these mechanisms acted to increase agency and action to access resources for mental health, consistent with other studies of psychosocial support group intervention in South Asian settings (Jordans et al., Reference Jordans, Aldridge, Luitel, Baingana and Kohrt2017; Morrison et al., Reference Morrison, Osrin, Alcock, Azad, Bamjan, Budhathoki, Kuddus, Mala, Manandhar, Nkhata, Pathak, Phiri, Rath, Tripathy, Costello and Houweling2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019). A group format may also increase the reach of an intervention because fewer trained facilitators are required. Psychosocial support groups merit further attention in both research and the development of interventions as an effective, relevant, acceptable, and scalable platform to promote mental health in communities.
Our findings illustrate how effective delivery of group interventions requires careful consideration of facilitators and setting in the planning phase. Mental health interventions delivered by lay health workers can benefit from building on existing community relationships outside of formal healthcare settings (Kohrt et al., Reference Kohrt, Asher, Bhardwaj, Fazel, Jordans, Mutamba, Nadkarni, Pedersen, Singla and Patel2018), and available evidence suggests that they are effective in improving quality of life and day-to-day functioning (van Ginneken et al., Reference van Ginneken, Chin, Lim, Ussif, Singh, Shahmalak, Purgato, Rojas-García, Uphoff, McMullen, Foss, Thapa Pachya, Rashidian, Borghesani, Henschke, Chong and Lewin2021). However, as we found, they can place an additional burden on providers with other responsibilities (Kohrt et al., Reference Kohrt, Asher, Bhardwaj, Fazel, Jordans, Mutamba, Nadkarni, Pedersen, Singla and Patel2018), and rely on appropriate community settings for delivery which may not always be readily available (Puffer and Ayuku, Reference Puffer and Ayuku2022). Our findings also reinforce the need for ongoing support and training to maintain motivation and fidelity in the face of challenges related managing multiple responsibilities and engaging participants (for example discordance between facilitator and participant gender) (Wall et al., Reference Wall, Kaiser, Friis-Healy, Ayuku and Puffer2020).
Several key determinants identified in this study influenced participation through altering intervention demand and accessibility. Existing relationships between facilitators and communities aided recruitment. Intervention relevance, achieved through design in partnership with mental health workers and communities, facilitated retention. Determinants of service demand have been suggested as effective targets for implementing mental health interventions that are best addressed through community engagement to increase trust and achieve supply of interventions that are culturally relevant and sensitive to local needs (Greene et al., Reference Greene, Huang, Giusto, Lovero, Stockton, Shelton, Santos, Saúte and Wainberg2021). However, despite local design and piloting in Dehradun, scaling implementation to nearby areas brought a new set of barriers affecting demand including varying community and family attitudes, and travel and agricultural chores for participants. Although there is limited research in this area (Kohrt et al., Reference Kohrt, Asher, Bhardwaj, Fazel, Jordans, Mutamba, Nadkarni, Pedersen, Singla and Patel2018), our experience highlights the importance of an iterative and responsive approach to community engagement that continues through all phases of implementation.
Challenges in engaging caregivers of people with disability is a recurrent theme in the area of disability work in India, stemming from limitations to the time and resources of caregivers, and to reach of social and health services (Madavanakadu et al., Reference Madavanakadu, Grills, Scaria, Benny and Joubert2021). Social isolation limits caregivers’ awareness and utilisation of available services, and poor health among caregivers limits the care that a person with disability receives. Improving the well-being of vulnerable caregivers can help them to engage with service providers, facilitating the delivery of appropriate services to those with disability (Devassy et al., Reference Devassy, Green, Cheguvera, Yohannan, Grills and Joubert2022). In this study, the implementation of Nae Umeed reached vulnerable target population groups including women and people with less education, although participants identifying as scheduled caste or tribe were similar to the Uttarakhand population. These findings reinforce the value of community-based models to engage with marginalised populations (Kohrt et al., Reference Kohrt, Asher, Bhardwaj, Fazel, Jordans, Mutamba, Nadkarni, Pedersen, Singla and Patel2018).
The partnership model in this study demonstrated how a cooperative approach across organisations could deliver a single intervention to support caregivers. NGOs can facilitate access to health services, particularly for the vulnerable, by providing free or low-cost community-based care (Sanadgol et al., Reference Sanadgol, Doshmangir, Majdzadeh and Gordeev2021). Each partner in the delivery of Nae Umeed had existing disability interests, so were able to identify caregivers of people with disability in their community. However, NGOs typically work independently and may have inadequate resources to undertake an intervention like Nae Umeed. In this example, the CHGN-UKC network worked collaboratively on implementation, a strategy that is important in India where there are more than 20,000 active non-profit health institutions (Central Statistics Office, 2012). The clustering approach of CHGN-UKC may help to increase access to resources, opportunities for collaboration, and credibility with the government (Grills et al., Reference Grills, Robinson and Phillip2012; Safe et al., Reference Safe, Grills, Wainwright and Lankester2014; Grills et al., Reference Grills, Varghese, Hughes, Jolly and Kumar2016). The CHGN-UKC cluster also provides an avenue for the findings presented here to be disseminated across providers and contexts.
The study also raises issues of the complexity in jointly delivering an intervention with different organisational entities, with little funding. Some partners were slow to implement due to competing priorities and lack of ownership of the intervention. The need for substantive engagement with partners and their leaders to support the implementation was evident in the findings of this study (Grills et al., Reference Grills, Robinson and Phillip2012).
Our study had several limitations. The CFIR has been widely applied, in high-income settings (Damschroder et al., Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009; Kirk et al., Reference Kirk, Kelley, Yankey, Birken, Abadie and Damschroder2016), yet may be less appropriate to LMICs where patterns or presentations of implementation determinants differ (Means et al., Reference Means, Kemp, Gwayi-Chore, Gimbel, Soi, Sherr, Wagenaar, Wasserheit and Weiner2020). We felt that the updated CFIR (Damschroder et al., Reference Damschroder, Reardon, Widerquist and Lowery2022) proved adequate to cover and classify determinants discussed in IDIs and FGDs. However, we recognise that our results primarily reflect determinants that we asked directly about or that study participants considered important. We found constructs related to individual characteristics less relevant, consistent with the experience of other authors, possibly due to organisational cultures having less focus on individuality in some LMICs (Means et al., Reference Means, Kemp, Gwayi-Chore, Gimbel, Soi, Sherr, Wagenaar, Wasserheit and Weiner2020). Assessment of implementation outcomes was hampered by missing data for some groups, and attendance data for the final five modules. There is no reliable data on the demographics of caregivers in Uttarakhand, making our assessment of reach rudimentary. Assessment of other implementation outcomes, such as cost and fidelity, would help to inform decisions around the use of similar implementation strategies but were infeasible to assess in this evaluation.
This study contributes to evidence gaps in the implementation of mental health programmes in LMICs (Esponda et al., Reference Esponda, Hartman, Qureshi, Sadler, Cohen and Kakuma2020). It is strengthened by the participation of service users in the evaluation and by implementation by a community-based organisation. It is relevant to the implementation of interventions that target caregivers, group interventions or those that focus mainly on prevention. The findings of this study can also inform others looking to implement group mental health and caregiver interventions in LMIC settings. There are few programmes and interventions targeting the needs of carers, although they are central to supporting people with psychosocial and other disabilities in LMIC (Hinton et al., Reference Hinton, Tran, Nguyen, Ho and Gitlin2019). Policymakers and national mental health and disability programmes should develop and implement interventions that increase mental health for carers (Hanlon et al., Reference Hanlon, Semrau, Alem, Abayneh, Abdulmalik, Docrat, Evans-Lacko, Gureje, Jordans, Lempp, Mugisha, Petersen, Shidhaye and Thornicroft2018), with a focus on studies of implementation processes. There are critical gaps in knowledge around what strengthens the psychosocial well-being of caregivers, particularly in LMIC, and implementation research should focus on interventions developed for local contexts (Bogart and Uyeda, Reference Bogart and Uyeda2009).
Conclusions
In evaluating the implementation of a locally developed group caregiver mental health intervention in urban and rural North India, this study identifies contextually relevant priorities for intervention and implementation strategy design. Supporting caregivers and their mental health yields positive outcomes for both carers and the family members with disabilities that they support. This is a high-priority group and improving their mental health and social participation requires active attention and coordinated action to support the psychosocial and socioeconomic needs of caregivers across the government and not-for-profit sectors.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2023.79.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. The complete data are not publicly available due to their containing information that could compromise the privacy of research participants.
Acknowledgements
Thanks to the whole Burans team in Dehradun district for the support in implementing Nae Umeed and to the CHGN-Cluster for support in implementation at the peri-urban site. Thanks to the Institutional Ethics Committee of EHA for ongoing input to study design and to Herbertpur Christian Hospital for their ongoing support to all implementation and evaluation work.
Author contribution
Conceptualization: K.M.; Data collection: S.R., L.B.; Formal analysis: C.R.B.; Investigation: D.A., S.R., L.B.; Methodology: C.R.B., D.A., K.M.; Supervision: K.M.; Writing – original draft: C.R.B., D.A.; Writing – review and editing: N.J.G. and K.M. Note that D.A. and C.R.B. are joint first authors.
Financial support
Research costs were covered by existing program funds.
Competing interest
The authors declare that they have no competing interests in the publication of this article.
Ethics statement
Approval for this project was provided by the institutional ethics committee of the Emmanuel Hospital Association (protocol number: 240).








Comments
COVER LETTER
Dear Editors of Global mental health,
We have chosen your journal to submit this paper as it highlights the contribution and value of implementation research to understand interventions, and is a noted gap in low and middle income countries. It is also well-paired with our pre-post evaluation of the same intervention which is currently under 2nd review with your journal.
First, this paper identifies the importance of context for intervention and implementation strategy design. It is based on a locally developed mental health intervention for caregivers in North India. It will inform others looking to implement group mental health and caregiver interventions in South Asian settings.
Secondly, this study focuses on implementation barriers and enablers – using the updated Consolidated Framework for Implementation Research (CFIR) which increases the scalability, generalisability and relevance of the findings and informs others looking to implement group mental health and caregiver interventions in LMIC and South Asian settings. We additionally focused on domains like group delivery format, competing responsibilities for caregivers and challenges and opportunities associated with the partnership delivery model.
Thirdly, the study has been undertaken by a multidisciplinary, multi-country authorship team. DA, LB and SR are social work based mental health practitioners based in a non-profit organisation in North India; KM works and researches in community mental health in India and New Zealand, NG and CB are public health physicians working between Australia and India.
Please note that the position of first authorship is with equal contribution by Disha Agarwal and Chris Bailie and so we request you note that these are joint first authors.
Thank you for your consideration of this paper for publication.
Kaaren Mathias (corresponding and senior author)