The prevalence of overweight and obesity has increased in developed and developing countries, particularly over the last 30 years( 1 ). According to BMI, the WHO estimates that 1·6 billion adults are overweight (BMI ≥ 25·0 kg/m2) and 400 million of these are obese (BMI ≥ 30·0 kg/m2)( 2 ). Weight gain is determined by interactions among genetic, environmental, psychological and social factors, which result in an imbalance between energy intake and expenditure( Reference Prentice and Jeb 3 ). Lifestyle changes that lead to decreased physical activity and poor diet are identified as the basis for this energy imbalance( Reference Swinburn, Egger and Raza 4 ).
Systematic reviews have shown that the traditional approaches to overweight, based on clinical and pharmacological treatments, have achieved limited success( Reference Hardeman, Griffin and Johnston 5 – Reference Lemmens, Oenema and Klepp 7 ). There is a consensus that public health actions for overweight prevention and control should adopt ecological models that recognise the existence of multiple factors associated with weight gain( Reference Swinburn, Gill and Kumanyika 8 , Reference Brown, Kelly and Summerbell 9 ).
Furthermore, studies suggest that continued interventional contracts, such as goal setting and self-monitoring, with support from the environment, can lead to sustained weight maintenance and loss( Reference Wing and Phelan 10 – Reference Butryn, Phelan and Hill 12 ). Most self-regulatory theories assume that self-monitoring precedes the self-evaluation of progress made towards one's goal and subsequent self-reinforcement( Reference Kanfer 13 , Reference Kirschenbaum 14 ).
Weight monitoring can provide an opportunity for positive reinforcement when changes in behaviour are associated with weight loss or the avoidance of weight gain( Reference Butryn, Phelan and Hill 12 ). Among the possible sites for the development of interventions to prevent weight gain, the workplace is considered an ideal setting for these initiatives given that it provides easy and regular access to a large number of people. In addition, interventional programmes can combine environmental and individual strategies and may encourage sustained behaviour changes( Reference Glanz, Patterson and Kristal 15 , Reference Bull, Gillette and Glasgow 16 ).
However, few interventional studies on weight gain prevention at the workplace have been conducted in developing countries. Thus, the aim of the present study was to evaluate the impact of a worksite intervention to prevent weight gain among adult workers.
Methods
A controlled community trial was performed in four large companies in the city of São Paulo, Brazil, three of which comprised the intervention group (IG; pharmaceutical, communication and service-sector companies) and one of which was the control group (CG; a service-sector company). The study tested the hypotheses that the use of interactive software developed to aid the self-monitoring of weight and to send messages by email incentivising the adoption of a healthy lifestyle would support the weight management of workers.
We estimated the sample size for each study group to total 174 individuals and decided to consider a 0·69 kg difference in body weight at the end of the intervention as a benchmark for comparison between IG and CG (two-tailed test with a significance level of 5 % and a test power of 80 %). This expected variation was based on the mean annual weight gain of individuals aged between 21 and 64 years living in the city of São Paulo, which was obtained from the Surveillance System of Protection and Risk Factors for Chronic Diseases( Reference Moura, Morais Neto and Moura 17 ). The literature points to an annual weight gain of between 0·5 and 2 kg in American and European adults( Reference Williamson, Kahn and Byers 18 – Reference Visscher, Kromhout and Seidell 20 ). Eligible participants were workers aged 18–64 years with a BMI between 20·0 and 39·9 kg/m2. Exclusion criteria were minimal and included pregnant women, workers on a diet and users of drugs that affect weight. Figure 1 shows the trial profile.
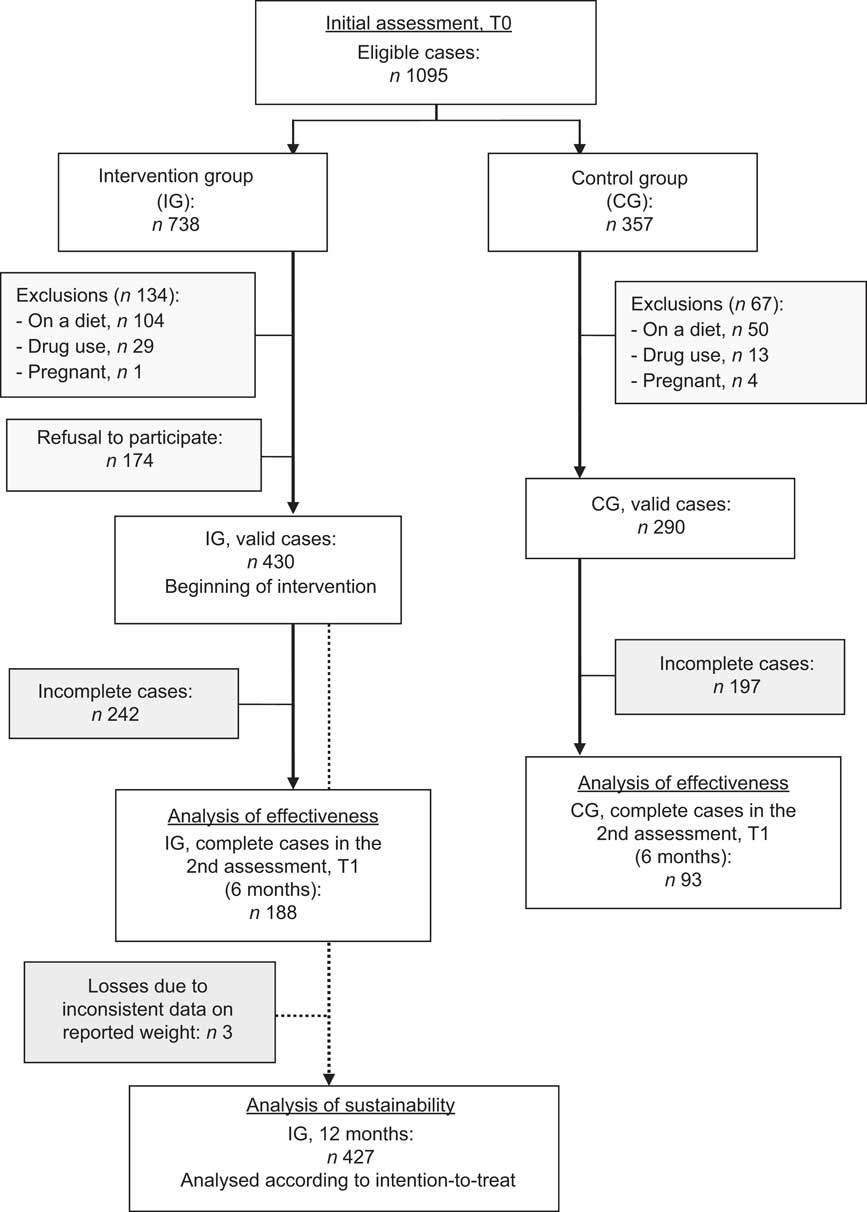
Fig. 1 Trial profile of participants; Healthy Weight Program, São Paulo, Brazil, 2008
Participants were recruited through companies and all workers were invited to participate. Randomisation occurred at the company level to avoid the possible contamination of interventional conditions. The proposed intervention adopted an educational health promotion approach based on the constructs of cognitive social theory and self-monitoring of health, and involved a combination of educational and organisational support (the companies left scales in accessible locations in the workplaces) for the behavioural changes( Reference Green and Kreuter 21 ).
The theoretical matrix used in the intervention's design, implementation and assessment was the model of planning of health promotion programmes proposed by Bartholomew et al. (2006), the Intervention Mapping Framework. The Intervention Mapping model proposes a sequence of six phases to plan an interventional programme that include such aspects as the following: (i) knowledge about the problem and behavioural determinants involved; (ii) definition of goals aimed at changes; (iii) selection based on the theory of intervention methods; (iv) selection of action strategies and tools; (v) development of an adoption and implementation plan; and (vi) programme impact assessment( Reference Bartholomew, Parcel and Kok 22 ).
The intervention was supported by interactive software developed specifically to aid the self-monitoring of weight, entitled the Healthy Weight Program (HWP). Workers had their email address registered and received an invitation to monitor their weight with the HWP software. Once registered to use the program, workers received a welcome message and practical recommendations for diet and physical activity in the form of short standard texts. One month later, a new message was sent by email, reminding participants to report their self-measured weights in the program using a quick link to the software.
When each new self-measured weight was sent by the worker, the software delivered the results of the assessment in the form of a progress chart and provided new diet and physical activity recommendations. This process occurred on a monthly basis until the twelfth month, when the intervention ended. The feedback, which included data on weight progress and goal weight and messages on healthy diet and physical activity, was designed according to the BMI and weight change of the participants during this period.
In-person data collection to assess the effectiveness of the intervention was performed at two points during the study: before the intervention at baseline (T0) and 6 months later (T1). At both time points, weight, height and waist circumference measurements of the IG and CG participants were taken. Standard techniques were used to obtain these measurements: height and weight were measured with individuals in light clothes and without shoes using standard apparatus. Weight was measured to the nearest 0·1 kg on a calibrated scale. Height and waist circumference were measured to the nearest 0·5 cm with a stadiometer and measuring tape, respectively( Reference Lohman, Roche and Matorell 23 ).
To evaluate the effectiveness of the intervention, we examined the changes in weight, BMI and waist circumference. Pearson's χ 2 test and Student's t test for independent samples were used to observe differences between the groups. Only individuals with complete data (measurements collected at T0 and T1) were considered in the assessment of the effectiveness of the intervention. The paired Student's t test was applied for intra-group comparisons (T0 v. T1) and Student's t test for independent samples was applied for comparisons between groups (IG v. CG). The crude effects of the intervention were estimated by univariate linear regression analysis and corresponded to the IG regression coefficient and 95 % confidence interval. The adjusted effects of the intervention corresponded to the IG regression coefficient and 95 % confidence interval in the linear regression model, after adjustment for the initial condition according to the initial BMI and sociodemographic variables (sex, age and level of education).
The indicator of the effect defined to assess the sustainability of the intervention was the weight change (kg) at 12 months, which was obtained from the measurements recorded in the HWP software. The sustainability evaluated the adequacy of this intervention to prevent weight gain and assessed factors associated with weight change among individuals exposed to the intervention. Thus, it was possible to evaluate the benefit of the intervention only using the weights sent in using the HWP software. Considering the fact that up to eleven weight measurements could be reported by participants throughout 12 months, the data were analysed according to the intention-to-treat method, which uses the LOCF (Last Outcome Measure Carried Forward) technique. This is characterised by considering the most recent measurement of an individual until the final assessment, assuming that the condition of the individual remains unchanged( Reference Altman 24 ). The main advantage of this technique is that it avoids the exclusion of individuals who dropped out of the study because they were not losing or maintaining weight. All IG participants who adhered to the intervention were included, i.e. those who sent at least one weight measurement to the HWP software.
The mean reported weight change and its 95 % confidence interval were explored according to the initial anthropometric and sociodemographic characteristics and the level of adherence to the intervention throughout 12 months (categorised into tertiles of frequencies of weight measurements sent to the HWP software). Student's t test was used to compare variables with two categories, while ANOVA was used for variables with three categories to compare weight variation according to sociodemographic characteristics.
Results
A total of 188 individuals in the IG (43·7 % of valid cases) and ninety-three in the CG (32·1 % of valid cases) were studied to analyse effectiveness. Incomplete cases were designated as individuals who did not complete the second measurement of weight, even if they continued to send their weight via the HWP software. Participants who completed both measurements of weight (complete cases) in the CG did not differ from those who did not (incomplete cases). In contrast, when participants in the IG were compared, incomplete cases without the second measure of weight had a mean initial weight (74·1 kg) significantly higher than the complete cases (71·1 kg; P < 0·05), although showing no difference in mean BMI. When the two allocation groups were compared, the IG showed a lower proportion of individuals aged between 18 and 29 years and a higher proportion of those who reported their ethnicity as white (P < 0·05) compared with the CG (Table 1).
Table 1 Sociodemographic and anthropometric characteristics of the study population according to allocation group and conclusion of the follow-up; Healthy Weight Program, São Paulo, Brazil, 2008

IG, intervention group; CG, control group; IC, incomplete cases (at 6 months follow-up); CC, complete cases (at 6 months follow-up).
*Pearson's χ 2 test for inter-allocation group comparison for CC: P < 0·05.
†Student's t test for intra-allocation group comparison: P < 0·05.
Table 2 assesses the crude and adjusted impact of the intervention by comparing the means of the anthropometric indicators in the IG and CG before the beginning of the programme and 6 months after it. With regard to body weight, IG participants showed a mean reduction of 0·62 kg. The net effect of the intervention was −0·77 kg, after adjustment for initial BMI, sex, age and level of education. In addition, reductions in BMI (adjusted effect equal to −0·28 kg/m2) and waist circumference (−1·05 cm) were observed.
Table 2 Crude and adjusted impacts of the intervention on anthropometric indicators after 6 months; Healthy Weight Program, São Paulo, Brazil, 2008
IG, intervention group; CG, control group; T0, initial assessment data; T1, assessment data after 6 months of intervention; Δ, difference between T0 and T1, WC, waist circumference.
*The crude effect corresponds to the IG regression coefficient (95 % CI) in a univariate linear regression model.
†The adjusted effect corresponds to the IG regression coefficient (95 % CI) in a linear regression model adjusted for initial BMI, sex, age and level of education.
Participants showed a different response to the intervention depending on their initial BMI category. In the CG, overweight participants (BMI ≥ 25·0 kg/m2) did not demonstrate a significant change in weight, whereas individuals with an initial BMI within the normal range (BMI < 25·0 kg/m2) showed significant increases in weight (+0·84 kg; P < 0·05) and BMI (+0·28 kg/m2; P < 0·05). With regard to the IG, the variations in weight (−1·03 kg; P < 0·05) and BMI (−0·38 kg/m2; P < 0·05) were significant only among overweight participants (Fig. 2).
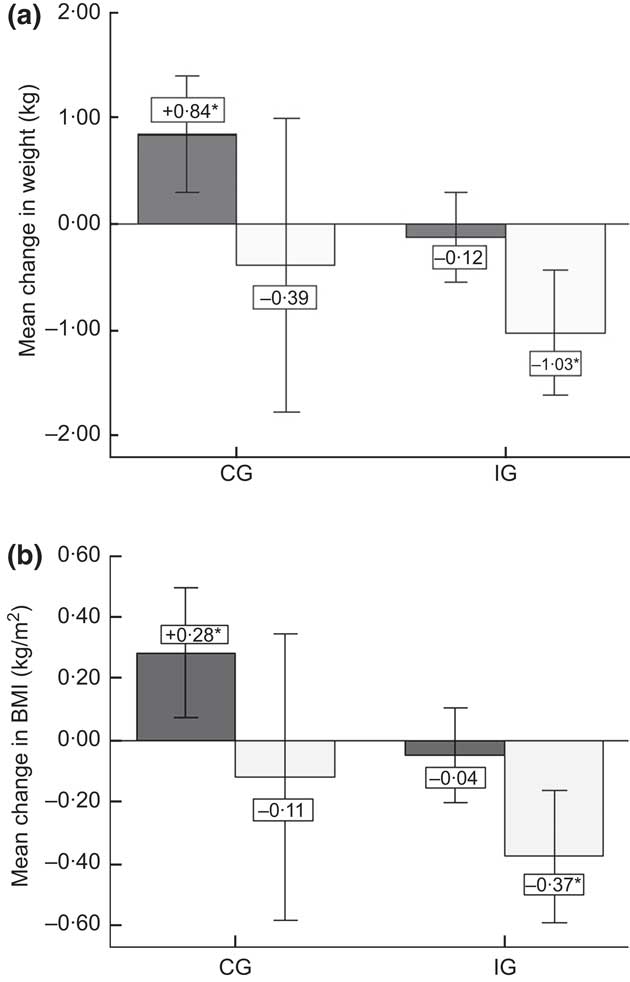
Fig. 2 Mean change in (a) self-reported weight and (b) BMI in the analysis of effectiveness at 6 months (n 281) according to allocation group (IG, intervention group; CG, control group) and initial presence of overweight (![]() , normal weight, BMI < 25·0 kg/m2;
, normal weight, BMI < 25·0 kg/m2; ![]() , overweight, BMI ≥ 25·0 kg/m2); Healthy Weight Program, São Paulo, Brazil, 2008. Values are means with their 95 % confidence intervals represented by vertical bars; *mean change (6 months v. 0 months) was significant (P < 0·05)
, overweight, BMI ≥ 25·0 kg/m2); Healthy Weight Program, São Paulo, Brazil, 2008. Values are means with their 95 % confidence intervals represented by vertical bars; *mean change (6 months v. 0 months) was significant (P < 0·05)
In the sustainability analysis, the progress of self-reported weight was assessed in the HWP software among IG participants after the 12 months of the study. Programme participants, beyond not gaining weight, actually showed a reduction in body weight (−0·72 kg). The weight change differed according to age group and was higher in individuals aged between 30 and 39 years (P = 0·024); the initial BMI category was assessed to have a greater effect on weight change among obese individuals (P < 0·001).
With regard to interventional adherence, there was a significant change in weight in the second and third tertiles of the frequency of weight measurements sent to the HWP software, at −0·93 kg (P < 0·001) and −0·83 kg (P < 0·001), respectively (Table 3). At the end of the 12 months of intervention, the majority maintained or lost weight (30·7 % and 43·1 %, respectively), whereas 26·2 % of participants gained weight.
Table 3 Mean change in self-reported weight at 12 months according to sociodemographic characteristics, initial BMI category and level of adherence; Healthy Weight Program, São Paulo, Brazil, 2008
*Student's t test or ANOVA (P < 0·05 indicates significance).
†Level of adherence to the intervention was described as tertiles of frequency of weight measurements sent to the HWP software, with the 1st tertile representing one to three weight measurements sent (n 136); the 2nd tertile, between four and seven (n 147); and the 3rd tertile, between eight and eleven (n 144).
Discussion
The proposed intervention was effective, resulting in significant reductions in weight, BMI and waist circumference in the IG compared with the CG. The net impact of the intervention on IG individuals’ body weight was −0·73 kg, while CG individuals’ weight increased. The intervention also resulted in a reduction of −0·26 kg/m2 in BMI and −0·99 cm in waist circumference in the IG. The analysis also showed that the intervention was effective at the end of 12 months, when individuals had a negative mean variation in weight.
Our findings are in agreement with the literature, which has consistently associated regular body weight monitoring with the maintenance and better control of weight( Reference Butryn, Phelan and Hill 12 , Reference O'Neil and Brown 25 , Reference Linde, Jeffery and Finch 26 ). Some studies have advocated the frequency of weighing on a daily or weekly basis( Reference Wing, Tate and Gorin 11 , Reference Levitsky, Garay and Nausbaum 27 , Reference Alm, Neumark-Sztainer and Story 28 ), as the self-monitoring of weight has been associated with the success of the intervention in the majority of studies( Reference Burke, Wang and Sevick 29 ).
The review conducted by Van Wormer et al. (2008) concluded that there is sufficient evidence supporting regular weight measurements as a self-monitoring strategy to maintain and control body weight. However, the impossibility of identifying the exact frequency of weight measurements and the duration of monitoring that are most effective should be emphasised( Reference Vanwormer, French and Pereira 30 ). Nevertheless, in the present study, the requirement of measuring body weight at least once monthly was able to achieve significant reductions in body measurements.
Detailed measurements of adherence to self-monitoring have not been frequently reported. As a result, little is known about the level to which individuals adhere( Reference Alm, Neumark-Sztainer and Story 28 ). A systematic literature review notes that the participation of workers in health promotion programmes performed at the workplace varies between 10 % and 64 %, with a median of 33 % and a higher frequency among women (OR = 1·67)( Reference Robroek, Van Lenthe and Van Empelen 31 ). In the present study, the second assessment of anthropometric indicators could be performed only in 43·7 % of individuals in the IG and in 32·1 % in the CG, and there was no significant difference in the participation rate between the sexes. The low participation in the second measurement of weight could be explained by the complexity of the task of obtaining anthropometric measurements at the workplace due to dynamic business organisation. There was no significant difference between complete and incomplete cases when analysed for effectiveness, and thus the losses most likely did not affect the internal validity of the study. Seeking to resolve this problem and to analyse a higher number of intervention participants we performed the sustainability analysis, where the weight change recorded in the HWP software over 12 months was the indicator used to evaluate the weight gain prevention.
In the analysis of sustainability we used the LOCF technique, which considers that the variable analysed remains unchanged through the remainder of the study, if the workers have continued to participate. In none of the studies was a ‘true’ intention-to-treat approach assessed. The higher the dropout rate, the more likely the approach of carrying the last observation forward is to produce unreliable results. To minimise this limitation, we analysed the results according to the rate of adherence to the intervention.
The majority of IG participants adhered to the proposed intervention. However, the frequency of weight measurements sent to the HWP software monthly was gradually reduced. The median of number of weight measurements sent at the end of 12 months was five, with three in the 25th percentile and nine in the 75th percentile. Eysenbach (2005) argues that participation rates between 40 % and 50 % in the form of non-adherence to or abandonment of the programme and the loss to follow-up are common in online health interventions( Reference Eysenbach 32 ). When considering interventions performed at the workplace and transmitted over the Internet in particular, a study that tested the effectiveness of an annual anti-smoking programme obtained a participation rate of 28·5 %( Reference Graham, Cobb and Raymond 33 ). In contrast, a weight-loss intervention aimed at adult workers of a hospital showed attrition rates of 15 % at 3 months and 22 % at the end of 6 months( Reference Tate, Wing and Winett 34 ).
When interpreting the effect of adherence to the intervention on weight change, the fact that adherence was assessed according to the frequency of weight measurements sent monthly should be considered; i.e. adherence is directly associated with the length of time participants remain in the programme. The decreasing commitment of participants over time is another challenge of online interventions( Reference Bennett and Glasgow 35 ). In addition, most of the weight lost in weight-loss programmes occurs during the first 6 months of an intervention( Reference Bennett and Glasgow 35 ). There is little or no evidence of the long-term effectiveness of online interventions for the prevention of weight gain( Reference Svetkey, Stevens and Brantley 36 ).
Conclusion
The present study suggests that the behavioural intervention based on regular self-monitoring of weight was effective in maintaining weight among participants with adequate initial weight and in promoting significant reductions among those who were overweight at the end of 6 months. In addition, the analysis of sustainability revealed that the majority of participants either maintained or lost weight throughout 12 months and that those who showed greater adherence obtained better results at the end of the programme. More research on longer-term weight maintenance is needed.
Acknowledgements
Sources of funding: This research was supported by São Paulo Research Foundation (FAPESP) of Brazil (process number 2007/02540-1). FAPESP had no role in the design, analysis or writing of this article. Conflicts of interest: There are no conflicts of interest. Ethics: The study was approved by the ethics committee of the School of Public Health, University of São Paulo (number 1684). Authors’ contributions: P.C.J., D.H.B. and F.S. participated in the conception, analysis and interpretation of the data; with a significant contribution towards producing the draft or undertaking critical review of the content; and with participation in the approval of the final version of the manuscript.







